Six muscles outside the eye govern its movements. These muscles are the four rectus muscles—the inferior, medial, lateral, and superior recti—and the superior and inferior oblique muscles. The rectus muscles arise from a fibrous ring that encircles the optic nerve at the optic foramen, the opening through which the nerve passes, and are attached to the sclera, the opaque portion of the eyeball, in front of the equator, or widest part, of the eye. The superior oblique muscle arises near the rim of the optic foramen and somewhat nearer the nose than the origin of the rectus medialis. It ends in a rounded tendon that passes through a fibrous ring, the trochlea, that is attached to the frontal bone. The trochlea acts as a pulley. The tendon is attached to the sclera back of the equator of the eye.
The inferior oblique muscle originates from the floor of the orbit, passes under the eyeball like a sling, and is attached to the sclera between the attachments of the superior and lateral rectus muscles. The rectus muscles direct the gaze upward and downward and from side to side. The inferior oblique muscle tends to direct the eye upward, and the superior oblique to depress the eye; because of the obliqueness of the pull, each causes the eye to roll, and in an opposite direction.
The oblique muscles are strictly antagonistic to each other, but they work with the vertical rectus muscles in so far as the superior rectus and inferior oblique both tend to elevate the gaze and the inferior rectus and superior oblique both tend to depress the gaze. The superior and inferior recti do not produce a pure action of elevation or depression because their plane of action is not exactly vertical; in consequence, as with the obliques, they cause some degree of rolling (torsion), but by no means so great as that caused by the obliques; the direction of rolling caused by the rectus muscle is opposite to that of its synergistic oblique; the superior rectus causes the eye to roll inward, and the inferior oblique outward.
The eye
General description
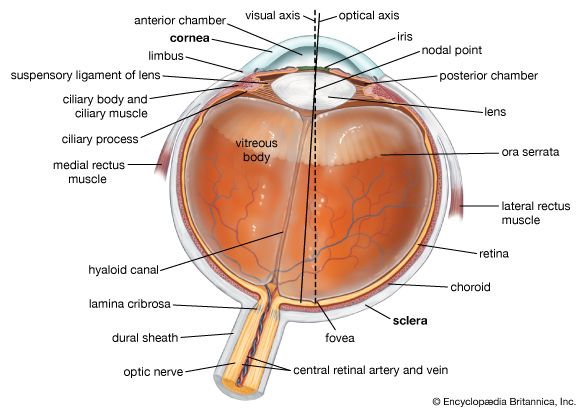
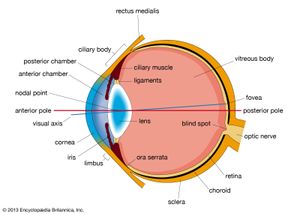
The eyeball is not a simple sphere but can be viewed as the result of fusing a small portion of a small, strongly curved sphere with a large portion of a large, not so strongly curved sphere. The small piece, occupying about one-sixth of the whole, has a radius of 8 mm (0.3 inch); it is transparent and is called the cornea; the remainder, the scleral segment, is opaque and has a radius of 12 mm (0.5 inch). The ring where the two areas join is called the limbus. Thus, on looking directly into the eye from in front one sees the white sclera surrounding the cornea; because the latter is transparent one sees, instead of the cornea, a ring of tissue lying within the eye, the iris. The iris is the structure that determines the colour of the eye. The centre of this ring is called the pupil. It appears dark because the light passing into the eye is not reflected back to any great extent. By use of an ophthalmoscope, an instrument that permits the observer to illuminate the interior of the eyeball while observing through the pupil, the appearance of the interior lining of the globe can be made out. Called the fundus oculi, it is characterized by the large blood vessels that supply blood to the retina; these are especially distinct as they cross over the pallid optic disk, or papilla, the region where the optic nerve fibres leave the globe.
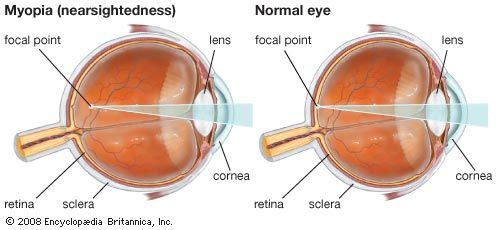
The dimensions of the eye are reasonably constant, varying among normal individuals by only a millimetre or two; the sagittal (vertical) diameter is about 24 mm (about one inch) and is usually less than the transverse diameter. At birth the sagittal diameter is about 16 to 17 mm (about 0.65 inch), it increases rapidly to about 22.5 to 23 mm (about 0.89 inch) by the age of three years, and between age three and 13 the globe attains its full size. The weight is about 7.5 grams (0.25 ounce) and its volume about 6.5 cm3 (0.4 cubic inch).
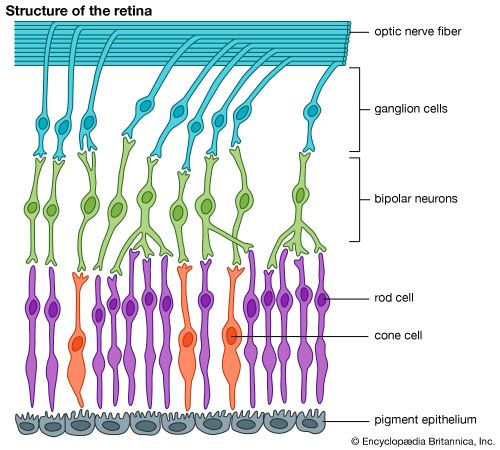
The eye is made up of three coats, which enclose the optically clear aqueous humour, lens, and vitreous body. The outermost coat consists of the cornea and the sclera; the middle coat contains the main blood supply to the eye and consists, from the back forward, of the choroid, the ciliary body, and the iris. The innermost layer is the retina, lying on the choroid and receiving most of its nourishment from the vessels within the choroid, the remainder of its nourishment being derived from the retinal vessels that lie on its surface and are visible in the ophthalmoscope. The ciliary body and iris have a very thin covering, the ciliary epithelium and posterior epithelium of the iris, which is continuous with the retina.
Within the cavities formed by this triple-layered coat there are the crystalline lens, suspended by fine transparent fibres—the suspensory ligament or zonule of Zinn—from the ciliary body; the aqueous humour, a clear fluid filling the spaces between the cornea and the lens and iris; and the vitreous body, a clear jelly filling the much larger cavity enclosed by the sclera, the ciliary body, and the lens. The anterior chamber of the eye is defined as the space between the cornea and the forward surfaces of the iris and lens, while the posterior chamber is the much smaller space between the rear surface of the iris and the ciliary body, zonule, and lens; the two chambers both contain aqueous humour and are in connection through the pupil.
Outer and middle tunics of the globe
The outermost coat
The outermost coat is made up of the cornea and the sclera. The cornea is the transparent window of the eye. It contains five distinguishable layers; the epithelium, or outer covering; Bowman’s membrane; the stroma, or supporting structure; Descemet’s membrane; and the endothelium, or inner lining. Up to 90 percent of the thickness of the cornea is made up of the stroma. The epithelium, which is a continuation of the epithelium of the conjunctiva, is itself made up of about six layers of cells. The superficial layer is continuously being shed, and the layers are renewed by multiplication of the cells in the innermost, or basal, layer.
The stroma appears as a set of lamellae, or plates, running parallel with the surface and superimposed on each other like the leaves of a book; between the lamellae lie the corneal corpuscles, cells that synthesize new collagen (connective tissue protein) essential for the repair and maintenance of this layer. The lamellae are made up of microscopically visible fibres that run parallel to form sheets; in successive lamellae the fibres make a large angle with each other. The lamellae in man are about 1.5 to 2.5 microns (one micron = 0.001 mm) thick, so that there are about 200 lamellae in the human cornea. The fibrous basis of the stroma is collagen.
Immediately above the stroma, adjacent to the epithelium, is Bowman’s membrane, about eight to 14 microns thick; with the electron microscope it is evident that it is really stroma, but with the collagen fibrils not arranged in the orderly fashion seen in the rest of the stroma.
Beneath the stroma are Descemet’s membrane and the endothelium. The former is about five to 10 microns thick and is made up of a different type of collagen from that in the stroma; it is secreted by the cells of the endothelium, which is a single layer of flattened cells. There is apparently no continuous renewal of these cells as with the epithelium, so that damage to this layer is a more serious matter.
The sclera is essentially the continuation backward of the cornea, the collagen fibres of the cornea being, in effect, continuous with those of the sclera. The sclera is pierced by numerous nerves and blood vessels; the largest of these holes is that formed by the optic nerve, the posterior scleral foramen. The outer two-thirds of the sclera in this region continue backward along the nerve to blend with its covering, or dural sheath—in fact, the sclera may be regarded as a continuation of the dura mater, the outer covering of the brain. The inner third of the sclera, combined with some choroidal tissue, stretches across the opening, and the sheet thus formed is perforated to permit the passage of fasciculi (bundles of fibres) of the optic nerve. This region is called the lamina cribrosa. The blood vessels of the sclera are largely confined to a superficial layer of tissue, and these, along with the conjunctival vessels, are responsible for the bright redness of the inflamed eye. As with the cornea, the innermost layer is a single layer of endothelial cells; above this is the lamina fusca, characterized by large numbers of pigment cells.
The most obvious difference between the opaque sclera and the transparent cornea is the irregularity in the sizes and arrangement of the collagen fibrils in the sclera by contrast with the almost uniform thickness and strictly parallel array in the cornea; in addition, the cornea has a much higher percentage of mucopolysaccharide (a carbohydrate that has among its repeating units a nitrogenous sugar, hexosamine) as embedding material for the collagen fibrils. It has been shown that the regular arrangement of the fibrils is, in fact, the essential factor leading to the transparency of the cornea.
When the cornea is damaged—e.g., by a virus infection—the collagen laid down in the repair processes is not regularly arranged, with the result that an opaque patch called a leukoma, may occur.
When an eye is removed or a person dies, the cornea soon loses its transparency, becoming hazy; this is due to the taking in of fluid from the aqueous humour, the cornea becoming thicker as it becomes hazier. The cornea can be made to reassume its transparency by maintaining it in a warm, well-aerated chamber, at about 31 °C (88 °F, its normal temperature); associated with this return of transparency is a loss of fluid.
Modern studies have shown that, under normal conditions, the cornea tends to take in fluid, mainly from the aqueous humour and from the small blood vessels at the limbus, but this is counteracted by a pump that expels the fluid as fast as it enters. This pumping action depends on an adequate supply of energy, and any situation that prejudices this supply causes the cornea to swell—the pump fails, or works so slowly that it cannot keep pace with the leak. Death is one cause of the failure of the pump, but this is primarily because of the loss of temperature; place the dead eye in a warm chamber and the reserves of metabolic energy it contains in the form of sugar and glycogen are adequate to keep the cornea transparent for 24 hours or more. When it is required to store corneas for grafting, as in an eye bank, it is best to remove the cornea from the globe to prevent it from absorbing fluid from the aqueous humour. The structure responsible for the pumping action is almost certainly the endothelium, so that damage to this lining can lead to a loss of transparency with swelling.
The cornea is exquisitely sensitive to pain. This is mediated by sensory nerve fibres, called ciliary nerves, that run just underneath the endothelium; they belong to the ophthalmic branch of the fifth cranial nerve, the large sensory nerve of the head. The ciliary nerves leave the globe through openings in the sclera, not in company with the optic nerve, which is concerned exclusively with responses of the retina to light.