Neosaxitoxin
| |

| |
| Names | |
|---|---|
| IUPAC name | |
| Other names
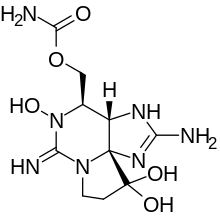
1H,10H-Pyrrolo(1,2-c)purine-10,10-diol, 2-amino-4-(((aminocarbonyl)oxy)methyl)-3a,4,5,6,8,9-hexahydro-5-hydroxy-6-imino-, (3aS,4R,10aS)-; 1H,10H-Pyrrolo(1,2-c)purine-10,10-diol, 2-amino-4-((aminocarbonyl)oxy)methyl-3a,4,5,6,8,9-hexahydro-5-hydroxy-6-imino-,(3aS,4R,10aS)-; 1H,10H-Pyrrolo(1,2-c)purine-10,10-diol, 2-amino-4-((aminocarbonyl)oxy)methyl-3a,4,5,6,8,9-hexahydro-5-hydroxy-6-imino-,(3aS-(3aalpha,4alpha,10aR*))-
| |
| Identifiers | |
3D model (JSmol)
|
|
| ChEBI | |
| ChemSpider | |
| ECHA InfoCard | 100.237.662 |
| KEGG | |
PubChem CID
|
|
| UNII | |
CompTox Dashboard (EPA)
|
|
| |
| |
| Properties | |
| C10H17N7O5 | |
| Molar mass | 315.286 |
| Hazards | |
| GHS labelling: | |

| |
| Danger | |
| H300 | |
| P264, P270, P301+P310, P321, P330, P405, P501 | |
Except where otherwise noted, data are given for materials in their standard state (at 25 °C [77 °F], 100 kPa).
| |
Neosaxitoxin (NSTX) is included, as other saxitoxin-analogs, in a broad group of natural neurotoxic alkaloids, commonly known as the paralytic shellfish toxins (PSTs). The parent compound of PSTs, saxitoxin (STX), is a tricyclic perhydropurine alkaloid, which can be substituted at various positions, leading to more than 30 naturally occurring STX analogues. All of them are related imidazoline guanidinium derivatives.[3]
Sources
[edit]NSTX, and other PSTs, are produced by several species of marine dinoflagellates (eukaryotes) and freshwater cyanobacteria, blue-green algae (prokaryotes), which can form extensive blooms around the world.[4] Under special conditions, during harmful algal blooms (HAB) or red tide, all these toxins may build up in filter-feeding shellfish, such as mussels, clams and oysters, and can produce an outbreak of Paralytic Shellfish Poisoning (PSP).[5]
Saxitoxin analogues associated to PSP can be divided into three categories:[6]
- Carbamate compounds, including saxitoxin, neosaxitoxin and gonyautoxins 1–4.
- N-sulfocarbamoyl compounds, including C and B toxins.
- Decarbamoyl compounds with respect to the presence or absence of 1-N-hydroxyl, 11-hydroxysulfate, and 21-N-sulfocarbamoyl substitutions as well as epimerization at the C-11 position.
Structure and properties
[edit]NSTX is quite similar to saxitoxin, like all the neurotoxins associated to PSP, the only difference is that NSTX shows one hydroxyl group bonded to nitrogen "1", where saxitoxyn contains one hydrogen.[7]
This purine is highly hydrophilic[8] and thermostable, it is not destroyed by cooking.[9] Moreover, is very stable in usual storage, specially in acidic condition.[10]
Mechanism of action
[edit]NSTX blocks the extracellular portion,[11] the outer vestibule,[12] of some voltage gated sodium channels in a very powerful and reversible manner, without affection of other ion channels.
"Voltage-gated", also called "voltage-sensitive" and "voltage-dependent" sodium channel also known as "VGSCs" or "Nav channel" are crucial elements of normal physiology in a variety of animals, including flies, leeches, squid and jellyfish, as well as mammalian and non-mammalian vertebrates. This large integral membrane protein plays an essential role in the initiation and propagation of action potentials in neurons, myocytes and other excitable cells.[13]
Nav channels form the basis for electrical excitability in animals. Nav channels evolved from Ca2+ channels and were present in the common ancestor of choanoflagellates and animals, although this channel was likely permeable to both Na+ and Ca2+. Thus, like many other neuronal channels and receptors, Nav channels predated neurons. Invertebrates possess two Nav channels (Nav1 and Nav2), whereas vertebrate Nav channels are of the Nav1 family.[14]
Sodium-channel proteins in the mammalian brain are composed of an association that include one alpha subunit and one or more auxiliary beta subunits. Nine types of alpha subunits have been described (Nav1.1 to Nav1.9), and a tenth related isoform (Nax) may also play some role as a Nav channel. Based in this information, ten Nav classes can be described: Nav1.1 to Nav1.9, and Nax.[15]
Former five,[16] but more recently, six[17] neurotoxin receptor sites have been recognized between the seven receptor site[18] located in the vertebrate sodium channel receptor alpha subunit:
- Site 1 binds the sodium channel blockers tetrodotoxin and saxitoxin.
- Site 2 binds lipid-soluble sodium channel activators such as veratridine.
- Site 3 binds alpha-scorpion and sea anemone toxins, which slow sodium channel inactivation.
- Site 4 binds beta-scorpion toxins, which affect sodium channel activation.
- Site 5 binds the polyether ladder brevetoxins and ciguatoxin.
- Site 6 binds delta-conotoxin.
- Local anesthetic receptor site binds local anesthetics, antiarrhythmic drugs and antiepileptic drugs
NSTX and other site 1 blockers have high affinity (very low dissociation constant) and high specificity for Nav channels. The action of NSTX produces minimal effect on cardiac Nav, where it exhibits about 20–60 fold lesser affinity than in Nav channels from rat skeletal muscle and rat brain.[19] Most data emphasize the role of "STX resistant" Nav channel 1.5 in human heart.[20][21]
Toxins such as neosaxitoxin and tetrodotoxin have less affinity for most cardiac Nav channels than for most Nav channels in nerve tissue. Moreover, NSTX is so active on nerve Nav channel than is roughly a million-fold more potent than lidocaine.[22]
Effects on humans
[edit]This mechanism of action can produce two well known kinds of effects in humans:
Toxic effect, associated to plasmatic levels of NSTX
[edit]It can be approximately described using one of the classical model of neurotoxic disease, known from ancient times as red tide, the most harmful algal bloom (HAB). This well known clinical model is the "paralytic shellfish poisoning".[23]
Of course, there are great differences between different algal blooms,[24][25][26][27] because of the mix of species included in each HAB, usually related to environmental conditions;[28] because of the levels and quality of PSTs produced in each HAB, that may be modulated by concurrent microorganism;[29][30][31][32] and, last but not least, because of the specific properties of each kind of PST, for example:
- Brevetoxins are lipid-soluble (hydrophobic) polyether marine toxins; their predominant effect is excitatory (blocked by tetrodotoxin), mediated by the enhancement of cellular Na+ influx; and bind to site 5 on Nav (like ciguatoxin).[33]
- Tetrodotoxin (TTX) toxicity is associated with marked and surprising cardiovascular effects (i.e.: hypotension and bradycardia).[34] Those effects are unexpected because of notorious TTX-resistance observed in vertebrate cardiac Nav channel. Moreover, this characteristic of the mammalian cardiac Nav channel is attributed to the cardiac predominance of the TTX-resistant Nav channel isoform (Nav1.5).[35] On the contrary, as presumed on physiologic basis, NSTX produces just mild and transient cardiovascular abnormalities during experimental intoxication (there are no data on pure NSTX clinical toxicity).
- STX has two positive charges, in contrast to TTX's single charge and GTX2/3, a naturally occurring STX congener with a net +1 charge. In view of their rather different structures, it is not surprising that STX and TTX bind in a different fashion to VGSCs. In fact, when Phe 385 near the selectivity filter of Nav1.2 is mutated to Cys, the channel's affinity for TTX is reduced 3,000-fold, whereas that for STX is reduced (only) 340-fold.[36]
- There are very limited data on the relative potency of different PSTs, and developing alternative methods to animal bioassays for marine-toxin detection is an urgent need.[37]
In spite of its heterogeneous and poorly understood epidemiology, the clinical picture of PSP could be useful to anticipate clinical effects of systemic NSTX.
- In the most frequent and benign situation, the patient suffers just mild, short-lived paresthesias of the mouth or extremities.
- In moderate cases perioral tingling progressing to numbness spreading to face and neck can be observed.[38]
- In severe cases, patient can suffer apnea secondary to motor block, requiring mechanical ventilation.[39]
Usually, the victims of mild and severe acute intoxications eliminate the toxin in urine during the first 24 hours after ingestion, and improve to full recovery in the first day of intrahospital care (when vital support is provided in a timely manner).[40]
When outbreaks of PSP occur in remote locations, where medical assistance is limited, reported lethality is under 10% in adults, but can reach 50% in children younger than six years old. This difference could be secondary to dissimilar doses and composition of involved mixes of PSTs; delay in medical support; or some kind of susceptibility of children.[41] More recent information suggest that lethality could be around 1% of symptomatic patients,[42] including cases where air transportation was required from remote locations of Alaska.[43]
Electrophysiologic observations demonstrated sub clinical abnormalities lasting for some days[44] or weeks[45] after clinical recovery .
Some evidence suggest the presence of metabolic pathways for the sequential oxidation and glucuronidation of PST in vitro, both being the initial detoxication reactions for the excretion of these toxins in humans.[46]
Forensic analysis of fatalities after severe cases, conclude that PSP toxins are metabolically transformed by humans and that they are removed from the body by excretion in the urine and feces like any other xenobiotic compound.[47]
Considering the heterogeneous nature of toxins mixes contained in contaminated bivalve molluscs, the safe limit of toxin content in shellfish adequate for human ingestion is expressed in "saxitoxin equivalents". According to the Food and Agriculture Organization of the United Nations (FAO) and European Parliament, this limit is 80 microgram of saxitoxin equivalent per 100 gram of mussel meat (each mussel weights around 23 g).[48][49] The U.S. Food and Drug Administration extends the same definition to "fish" quality, but the term "fish" refers to fresh or saltwater fin fish, crustaceans, other forms of aquatic animal life other than birds or mammals, and all mollusks; and incorporate the use of "ppm" as another measure for saxitoxin equivalent concentration in mentioned foods.[50]
Paradoxically, the chronic and/or repeated exposure to marine seafood toxins, which is a much more realistic phenomenon, has not been fully examined.[51][52] One study in rats exposed to chronic (12 weeks) NSTX administration demonstrated some reduction in water and food intake, and a mild degree of transient cholestasis, probably associated to fasting, without other abnormalities.[53]
Anesthetic effect, produced by local infiltration of NSTX
[edit]This action has been demonstrated in animals[54] and humans.[55][56][57][58][59]
The medical use of the NSTX anesthetic effect is supported by three reasons:
- NSTX anesthetic duration:
- Any current available local anesthetic hardly produces clinical effects 12 hours after a single injection.[60] Then, in cases of severe or prolonged pain, some patients need repeated injections, catheters, pumps and opioids[61][62] to feel comfortable, with different kinds of side effects, costs and risks.[63]
- On the other hand, NSTX local infiltration produces long lasting anesthesia, well over all the current available local anesthetics. Some investigations demonstrated anesthetic effect lasting over one week after single injection in rodents, using extended release formulation, without histologic or functional sequelae.[64]
- Additionally, two human reports demonstrated strong potentiation between NSTX anesthetic effect, bupivacaine and epinephrine.[65][66]
- NSTX local safety:
- All available local anesthetic are associated with local damage in different models.[67][68][69][70][71] This undesired effect could be enhanced by sustained release formulations.[72]
- On the contrary, several investigations show local safety of saxitoxin-related neurotoxins, including very sensitive models, and there is no reason to presume otherwise for NSTX.[73][74][75][76]
- NSTX systemic safety:
- In spite of advances of ultrasound guided injections, acute systemic local anesthetic toxicity is still an unsolved clinical problem, and can produce devastating consequences, related to the neurologic and cardiovascular effects of all available local anesthetics.[77][78]
- Otherwise, clinical experience and animal models shows the relative safety of accidental and experimental NSTX intoxication (when appropriate support therapy is provided in a timely manner).[79]
- Recent investigation in sheep shows a safe limit, due to motor block, over 1 μg/kg for intravenous injection of NSTX, with full recovery after a brief course of mechanical ventilation.[80]
- Regarding systemic safety, saxitoxins diffuse through the blood–brain barrier,[81] but, because of Nav channel specificity, acute toxicity is associated to a very low risk of seizures. This establishes an important difference with current local anesthetic toxicity.[82]
- As could be predicted from its ion channel selectivity,[83] NSTX intoxication clinical picture is almost devoid of arrhythmias, establishing another difference with available local anesthetic's numerous cardiac effects.[84]
- And last but not least, some degree of improving in therapeutic index of NSTX can be observed when is mixed with bupivacaine and/or epinephrine.[85]
In conclusion, NSTX is a well defined molecule with a long-lasting and sometimes dangerous relationship with human subjects. Recent investigations suggest a clinical application as a new local anesthetic that sounds "too good to be true", but more investigation is required.[86]
See also
[edit]References
[edit]- ^ United States National Library of Medicine (NLM). ChemoIDplus Advanced. Registry number: 64296-20-4 (accessed: May 12, 2012) [1]
- ^ National Center for Biotechnology Information (NCBI). PubChem Compound (accessed: May 12, 2012) [2]
- ^ Mihali TK, Kellmann R, Neilan BA (March 2009). "Characterisation of the paralytic shellfish toxin biosynthesis gene clusters in Anabaena circinalis AWQC131C and Aphanizomenon sp. NH-5". BMC Biochemistry. 10: 8. doi:10.1186/1471-2091-10-8. PMC 2679770. PMID 19331657.
- ^ Wiese M, D'Agostino PM, Mihali TK, Moffitt MC, Neilan BA (July 2010). "Neurotoxic Alkaloids: Saxitoxin and Its Analogs". Marine Drugs. 8 (7): 2185–2211. doi:10.3390/md8072185. PMC 2920551. PMID 20714432.
- ^ Centers for Disease Control and Prevention (CDC). CDC's Laboratory Response to Toxins (accessed: May 8, 2012) [3]
- ^ Wang DZ (March 2008). "Neurotoxins from Marine Dinoflagellates: A Brief Review". Marine Drugs. 6 (3): 349–71. doi:10.3390/md6020349. PMC 2525493. PMID 18728731.
- ^ Hu SL, Kao CY (March 1991). "Interactions of neosaxitoxin with the sodium channel of the frog skeletal muscle fiber". The Journal of General Physiology. 97 (3): 561–78. doi:10.1085/jgp.97.3.561. PMC 2216488. PMID 1645395.
- ^ Etheridge SM (August 2010). "Paralytic shellfish poisoning: seafood safety and human health perspectives". Toxicon. 56 (2): 108–22. Bibcode:2010Txcn...56..108E. doi:10.1016/j.toxicon.2009.12.013. PMID 20035780.
- ^ Lawrence JF, Maher M, Watson-Wright W (January 1994). "Effect of cooking on the concentration of toxins associated with paralytic shellfish poison in lobster hepatopancreas". Toxicon. 32 (1): 57–64. Bibcode:1994Txcn...32...57L. doi:10.1016/0041-0101(94)90021-3. PMID 9237337.
- ^ Alfonso A, Louzao MC, Vieytes MR, Botana LM (December 1994). "Comparative study of the stability of saxitoxin and neosaxitoxin in acidic solutions and lyophilized samples". Toxicon. 32 (12): 1593–8. Bibcode:1994Txcn...32.1593A. doi:10.1016/0041-0101(94)90318-2. PMID 7725328.
- ^ Tarnawa I, Bölcskei H, Kocsis P (January 2007). "Blockers of Voltage-Gated Sodium Channels for the Treatment of Central Nervous System Diseases". Recent Patents on CNS Drug Discovery. 2 (1): 57–78. doi:10.2174/157488907779561754. PMID 18221218.
- ^ Penzotti JL, Lipkind G, Fozzard HA, Dudley SC Jr (February 2001). "Specific neosaxitoxin interactions with the Na+ channel outer vestibule determined by mutant cycle analysis". Biophysical Journal. 80 (2): 698–706. Bibcode:2001BpJ....80..698P. doi:10.1016/S0006-3495(01)76049-3. PMC 1301268. PMID 11159437.
- ^ Catterall WA. (April 2012). "Voltage-Gated Sodium Channels at 60: Structure, Function, and Pathophysiology". The Journal of Physiology. 590 (Pt 11): 2577–89. doi:10.1113/jphysiol.2011.224204. PMC 3424717. PMID 22473783.
- ^ Zakon H. (June 2012). "Adaptive evolution of voltage-gated sodium channels: the first 800 million years". Proceedings of the National Academy of Sciences of the United States of America. 109 (Suppl 1): 10619–25. Bibcode:2012PNAS..10910619Z. doi:10.1073/pnas.1201884109. PMC 3386883. PMID 22723361.
- ^ Yu FH, Catterall WA (July 2003). "Overview of the voltage-gated sodium channel family". Genome Biology. 4 (3): 207. doi:10.1186/gb-2003-4-3-207. PMC 153452. PMID 12620097.
- ^ Fainzilber M, Kofman O, Zlotkin E, Gordon D (January 1994). "A new neurotoxin receptor site on sodium channels is identified by a conotoxin that affects sodium channel inactivation in molluscs and acts as an antagonist in rat brain" (PDF). Recent Patents on CNS Drug Discovery. 269 (4): 2574–80. PMID 8300586. Retrieved May 9, 2012.
- ^ Wang J, Yarov-Yarovoy V, Kahn R, Gordon D, Gurevitz M, Scheuer T, Catterall WA (September 2011). "Mapping the receptor site for alpha-scorpion toxins on a Na+ channel voltage sensor". PNAS. 108 (37): 15426–31. Bibcode:2011PNAS..10815426W. doi:10.1073/pnas.1112320108. PMC 3174582. PMID 21876146.
- ^ Catterall WA, Goldin AL, Waxman SG (December 2005). "International Union of Pharmacology. XLVII. Nomenclature and structure-function relationships of voltage-gated sodium channels". Pharmacological Reviews. 57 (4): 397–409. doi:10.1124/pr.57.4.4. PMID 16382098. S2CID 7332624.
- ^ Guo XT, Uehara A, Ravindran A, Bryant SH, Hall S, Moczydlowski E (December 1987). "Kinetic basis for insensitivity to tetrodotoxin and saxitoxin in sodium channels of canine heart and denervated rat skeletal muscle". Biochemistry. 26 (24): 7546–56. doi:10.1021/bi00398a003. PMID 2447944.
- ^ Lowe JS, Palygin O, Bhasin N, Hund TJ, Boyden PA, Shibata E, Anderson ME, Mohler PJ (January 2008). "Voltage-gated Nav channel targeting in the heart requires an ankyrin-G dependent cellular pathway". The Journal of Cell Biology. 180 (1): 173–86. doi:10.1083/jcb.200710107. PMC 2213608. PMID 18180363.
- ^ Abriel H (May 7, 2012). "Cardiac Sodium Channel Nav1.5 Mechanosensitivity is Inhibited by Ranolazine". Circulation. 125 (22): 2681–3. doi:10.1161/CIRCULATIONAHA.112.110908. PMID 22565937.
- ^ Butterworth JF 4th (March–April 2011). "Will conventional local anesthetics soon be replaced by neurotoxins?". Regional Anesthesia and Pain Medicine. 36 (2): 101–2. doi:10.1097/AAP.0b013e31820db23e. PMID 21326065. S2CID 33189422.
{{cite journal}}: CS1 maint: numeric names: authors list (link) - ^ FAO FOOD AND NUTRITION PAPER 80. Food and Agriculture Organization of the United Nations. Chapter 2. Paralytic Shellfish Poisoning (PSP). Rome, 2004(accessed: May 6, 2012)[4][permanent dead link]
- ^ Salfate O, Vazquez J, Galván J, Sánchez A, Nazar A (May–June 1991). "Intoxicaciones por toxina paralizante de molusco en Oaxaca" (PDF). Salud Pública de México (in Spanish). 33 (3): 240–7. Retrieved May 10, 2012.
- ^ Anderson DM (August 1994). "Red tides". Scientific American. 271 (2): 62–8. Bibcode:1994SciAm.271b..62A. doi:10.1038/scientificamerican0894-62. PMID 8066432. (accessed: May 9, 2012) [5]
- ^ Sivonen K, Jones G (1999). "3. Cyanobacterial Toxins". In Chorus I, Bartram J (eds.). Toxic Cyanobacteria in Water: A guide to their public health consequences, monitoring and management. World Health Organization. ISBN 0-419-23930-8. Archived from the original on 30 March 2013. Retrieved 10 May 2012.
{{cite book}}: CS1 maint: bot: original URL status unknown (link) [6] - ^ Glibert PM, Anderson DM, Gentien P, Granéli E, Sellner KG (June 2005). "The Global, Complex Phenomena of Harmful Algal Blooms". Oceanography. 18 (2): 136–47. doi:10.5670/oceanog.2005.49. hdl:1912/2790.(accessed: May 11, 2012) [7] Archived 2006-05-10 at the Wayback Machine
- ^ Hayashi M, Yanagi T (2008). "Analysis of change of red tide species in Yodo River estuary by the numerical ecosystem model" (PDF). Marine Pollution Bulletin. 57 (1–5): 103–7. Bibcode:2008MarPB..57..103H. doi:10.1016/j.marpolbul.2008.04.015. PMID 18513758. S2CID 21200491. Archived from the original (PDF) on 2018-11-03. Retrieved 2019-12-11.
- ^ Gallacher S, Flynn KJ, Franco JM, Brueggemann EE, Hines HB (January 1997). "Evidence for production of paralytic shellfish toxins by bacteria associated with Alexandrium spp. (Dinophyta) in culture". Applied and Environmental Microbiology. 63 (1): 239–45. Bibcode:1997ApEnM..63..239G. doi:10.1128/AEM.63.1.239-245.1997. PMC 168316. PMID 9065273.
- ^ Grzebyk D, Denardou A, Berland B, Pouchus YF (August 1997). "Evidence of a new toxin in the red-tide dinoflagellate Prorocentrum minimum". Journal of Plankton Research. 19 (8): 1111–24. doi:10.1093/plankt/19.8.1111.
- ^ Zheng TL, Su JQ, Maskaoui K, Yu ZM, Hu Z, Xu JS, Hong HS (2005). "Microbial modulation in the biomass and toxin production of a red-tide causing alga". Marine Pollution Bulletin. 51 (8–12): 1018–25. Bibcode:2005MarPB..51.1018Z. doi:10.1016/j.marpolbul.2005.02.039. PMID 16291201.
- ^ Alonso Rodríguez R, Ochoa JL, Uribe Alcocer M (January–June 2005). "Grazing of heterotrophic dinoflagellate Noctiluca scintillans (Mcartney) Kofoid on Gymnodinium catenatum Graham". Revista Latinoamericana de Microbiología. 47 (1–2): 6–10. PMID 17061541.
- ^ Baden DG (May 1989). "Brevetoxins: unique polyether dinoflagellate toxins". The FASEB Journal. 3 (7): 1807–17. doi:10.1096/fasebj.3.7.2565840. PMID 2565840. S2CID 44847897.
- ^ How CK, Chern CH, Huang YC, Wang LM, Lee CH (January 2003). "Tetrodotoxin poisoning". The American Journal of Emergency Medicine. 21 (1): 51–4. doi:10.1053/ajem.2003.50008. PMID 12563582.
- ^ Vornanen M, Hassinen M, Haverinen J (2011). "Tetrodotoxin sensitivity of the vertebrate cardiac Na+ current". Marine Drugs. 9 (11): 2409–22. doi:10.3390/md9112409. PMC 3229242. PMID 22163193.
- ^ Zhang MM, Gruszczynski P, Walewska A, Bulaj G, Olivera BM, Yoshikami D (July 2010). "Cooccupancy of the outer vestibule of voltage-gated sodium channels by micro-conotoxin KIIIA and saxitoxin or tetrodotoxin". Journal of Neurophysiology. 104 (1): 88–97. doi:10.1152/jn.00145.2010. PMC 2904204. PMID 20410356.
- ^ Perez S, Vale C, Botana AM, Alonso E, Vieytes MR, Botana LM (July 2011). "Determination of toxicity equivalent factors for paralytic shellfish toxins by electrophysiological measurements in cultured neurons". Chemical Research in Toxicology. 24 (7): 1153–7. doi:10.1021/tx200173d. PMID 21619049.
- ^ Woods Hole Oceanographic Institution. Paralytic Shellfish Poisoning. Fleming LE. Last updated: May 7, 2008 (accessed: May 8, 2012)[8]
- ^ Yuen CW, Ng MH (April 2002). "Respiratory distress after consumption of sea snails" (PDF). Hong Kong Journal of Emergency Medicine. 9 (3): 159–61. doi:10.1177/102490790200900308. S2CID 115428542. Retrieved May 6, 2012.
- ^ Centers for Disease Control and Prevention (CDC) (December 2011). "Paralytic Shellfish Poisoning Southeast Alaska, May–June 2011". Morbidity and Mortality Weekly Report. 60 (45): 1554–56. PMID 22089968.(accessed: May 8, 2012)[9]
- ^ Rodrigue DC, Etzel RA, Hall S, de Porras E, Velasquez OH, Tauxe RV, Kilbourne EM, Blake PA (March 1990). "Lethal paralytic shellfish poisoning in Guatemala". American Journal of Tropical Medicine and Hygiene. 42 (3): 267–71. doi:10.4269/ajtmh.1990.42.267. PMID 2316796.
- ^ Cheng HS, Chua SO, Hung JS, Yip KK (April 1991). "Creatine kinase MB elevation in paralytic shellfish poisoning". Chest. 99 (4): 1032–3. doi:10.1378/chest.99.4.1032. PMID 2009759.
- ^ Gessner BD, Middaugh JP (April 1995). "Paralytic shellfish poisoning in Alaska: a 20-year retrospective analysis". American Journal of Epidemiology. 141 (8): 766–70. doi:10.1093/oxfordjournals.aje.a117499. PMID 7709919.
- ^ Long RR, Sargent JC, Hammer K (August 1990). "Paralytic shellfish poisoning. A case report and serial electrophysiologic observations". Neurology. 40 (8): 1310–2. doi:10.1212/wnl.40.8.1310. PMID 2381544. S2CID 33896985.
- ^ de Carvalho M, Jacinto J, Ramos N, de Oliveira V, Pinho e Melo T, de Sá J (August 1998). "Paralytic Paralytic shellfish poisoning: clinical and electrophysiological observations". Journal of Neurology. 245 (8): 551–4. doi:10.1007/s004150050241. PMID 9747920. S2CID 29180723.
- ^ García C, Barriga A, Díaz JC, Lagos M, Lagos N (January 2010). "Paralytic Route of metabolization and detoxication of paralyticshellfishtoxins in humans". Toxicon. 55 (1): 135–44. Bibcode:2010Txcn...55..135G. doi:10.1016/j.toxicon.2009.07.018. hdl:10533/141436. PMID 19632259.
- ^ García C, del Carmen Bravo M, Lagos M, Lagos N (February 2004). "Paralytic shellfish poisoning: post-mortem analysis of tissue and body fluid samples from human victims in the Patagonia fjords". Toxicon. 43 (2): 149–58. Bibcode:2004Txcn...43..149G. doi:10.1016/j.toxicon.2003.11.018. hdl:10533/175125. PMID 15019474.
- ^ FAO Food and Nutrition Paper 80. Food and Agriculture Organization of the United Nations. Chapter 8. Risk Assessment. Rome, 2004. (accessed: May 6, 2012) [10][permanent dead link]
- ^ The European Parliament and the Council of the European Union (April 2004). "Regulation (EC) N° 853/2004 of the European Parliament and of the Council of 29 April 2004 laying down specific hygiene rules for food of animal origin". Off J Eur Comm. 139: 61. (accessed: May 6, 2012)[11]
- ^ U.S. Food and Drug Administration. Fish and Fishery Products Hazards and Controls Guidance, Fourth Edition, November 2011. Chapter 6: Natural Toxins (p. 99–112). (accessed: May 6, 2012) [12] [13]
- ^ Woods Hole Oceanographic Institution. Marine Biotoxins and Harmful Algae: A National Plan. Chapter II. THE TOXINS. Risk Assessment. (accessed: May 8, 2012)[14]
- ^ Batoréu MC, Dias E, Pereira P, Franca S (May 2005). "Risk of human exposure to paralytic toxins of algal origin". Environmental Toxicology and Pharmacology. 19 (3): 401–6. Bibcode:2005EnvTP..19..401B. doi:10.1016/j.etap.2004.12.002. PMID 21783504.
- ^ Zepeda RJ, Candiracci M, Lobos N, Lux S, Miranda HF (September 2014). "Chronic Toxicity Study of Neosaxitoxin in Rats". Marine Drugs. 12 (9): 5055–71. doi:10.3390/md12095055. PMC 4178483. PMID 25257789.
- ^ Kohane DS, Lu NT, Gökgöl-Kline AC, Shubina M, Kuang Y, Hall S, Strichartz GR, Berde CB (Jan–Feb 2000). "The local anesthetic properties and toxicity of saxitonin homologues for rat sciatic nerve block in vivo". Regional Anesthesia and Pain Medicine. 25 (1): 52–9. doi:10.1097/00115550-200001000-00010. PMID 10660241.
- ^ Rodriguez-Navarro AJ, Lagos N, Lagos M, Braghetto I, Csendes A, Hamilton J, Berger Z, Wiedmaier G, Henriquez A (November 2006). "Intrasphincteric neosaxitoxin injection: evidence of lower esophageal sphincter relaxation in achalasia". American Journal of Gastroenterology. 101 (11): 2667–8. doi:10.1111/j.1572-0241.2006.00809_6.x. PMID 17090291. S2CID 1548289.
- ^ Rodriguez-Navarro AJ, Lagos N, Lagos M, Braghetto I, Csendes A, Hamilton J, Figueroa C, Truan D, Garcia C, Rojas A, Iglesias V, Brunet L, Alvarez F (February 2007). "Neosaxitoxin as a local anesthetic: preliminary observations from a first human trial". Anesthesiology. 106 (2): 339–45. doi:10.1097/00000542-200702000-00023. PMID 17264729. S2CID 19507764.
- ^ Rodríguez-Navarro AJ, Berde CB, Wiedmaier G, Mercado A, Garcia C, Iglesias V, Zurakowski D (March–April 2011). "Comparison of neosaxitoxin versus bupivacaine via port infiltration for postoperative analgesia following laparoscopic cholecystectomy: a randomized, double-blind trial". Regional Anesthesia and Pain Medicine. 36 (2): 103–9. doi:10.1097/aap.0b013e3182030662. hdl:10533/134301. PMID 21425506. S2CID 37539195.
- ^ Manríquez V, Castro Caperan D, Guzmán R, Naser M, Iglesia V, Lagos N (2015). "First evidence of neosaxitoxin as a long-acting pain blocker in bladder pain syndrome". Int Urogynecol J. 26 (6): 853–8. doi:10.1007/s00192-014-2608-2. PMID 25571865. S2CID 22432232.
- ^ Coppens SJR, Zawodny Z, Dewinter G, Neyrinck A, Balocco AL, Rex S. In search of the Holy Grail: Poisons and extended release local anesthetics. Best Pract Res Clin Anaesthesiol. 2019 Mar;33(1):3-21. doi:10.1016/j.bpa.2019.03.002 PMID 31272651
- ^ Leone S, Di Cianni S, Casati A, Fanelli G (August 2008). "Pharmacology, toxicology, and clinical use of new long acting local anesthetics, ropivacaine and levobupivacaine". Acta Biomedica. 79 (2): 92–105. PMID 18788503. (accessed: May 10, 2012) [15] Archived 2011-12-16 at the Wayback Machine
- ^ Aubrun F, Mazoit JX, Riou B (February 2012). "Postoperative intravenous morphine titration". British Journal of Anaesthesia. 108 (2): 193–201. doi:10.1093/bja/aer458. PMID 22250276.
- ^ Beilin Y, Halpern S (August 2012). "Focused review: ropivacaine versus bupivacaine for epidural labor analgesia". Anesthesia & Analgesia. 111 (2): 482–7. doi:10.1213/ANE.0b013e3181e3a08e. PMID 20529986.
- ^ Wu CL, Raja SN (June 2011). "Treatment of acute postoperative pain". Lancet. 377 (9784): 2215–25. doi:10.1016/S0140-6736(11)60245-6. PMID 21704871. S2CID 13140529.
- ^ Epstein-Barash H, Shichor I, Kwon AH, Hall S, Lawlor MW, Langer R, Kohane DS (April 2009). "Prolonged duration local anesthesia with minimal toxicity". Proceedings of the National Academy of Sciences of the United States of America. 106 (17): 7125–30. Bibcode:2009PNAS..106.7125E. doi:10.1073/pnas.0900598106. PMC 2678453. PMID 19365067.
- ^ Rodriguez-Navarro AJ, Lagos M, Figueroa C, Garcia C, Recabal P, Silva P, Iglesias V, Lagos N (November 2009). "Potentiation of local anesthetic activity of neosaxitoxin with bupivacaine or epinephrine: development of a long-acting pain blocker". Neurotoxicity Research. 16 (4): 408–15. doi:10.1007/s12640-009-9092-3. hdl:10533/141060. PMID 19636660. S2CID 23287251.
- ^ Lobo K, Donado C, Cornelissen L, Kim J, Ortiz R, Peake RW, Kellogg M, Alexander ME, Zurakowski D, Kurgansky KE, Peyton J, Bilge A, Boretsky K, McCann ME, Berde CB, Cravero J (October 2015). "A Phase 1, Dose-escalation, Double-blind, Block-randomized, Controlled Trial of Safety and Efficacy of Neosaxitoxin Alone and in Combination with 0.2% Bupivacaine, with and without Epinephrine, for Cutaneous Anesthesia". Anesthesiology. 123 (4): 873–85. doi:10.1097/ALN.0000000000000831. PMID 26275090. S2CID 22740054.
- ^ Zink W, Graf B (July–August 2004). "Review Articles: Local Anesthetic Myotoxicity". Regional Anesthesia and Pain Medicine. 29 (4): 333–40. doi:10.1016/j.rapm.2004.02.008. PMID 15305253. S2CID 26185858.
- ^ Bogatch MT, Ferachi DG, Kyle B, Popinchalk S, Howell MH, Ge D, You Z, Savoie FH (June 2006). "Cytotoxicity of lidocaine or bupivacaine on corneal endothelial cells in a rabbit model". Cornea. 25 (5): 590–6. doi:10.1097/01.ico.0000220775.93852.02. PMID 16783149. S2CID 21454799.
- ^ Perez-Castro R, Patel S, Garavito-Aguilar ZV, Rosenberg A, Recio-Pinto E, Zhang J, Blanck TJ, Xu F (March 2009). "Cytotoxicity of local anesthetics in human neuronal cells". Anesthesia & Analgesia. 108 (3): 997–1007. doi:10.1213/ane.0b013e31819385e1. PMID 19224816. S2CID 41982515.
- ^ Nouette-Gaulain K, Dadure C, Morau D, Pertuiset C, Galbes O, Hayot M, Mercier J, Sztark F, Rossignol R, Capdevila X (November 2009). "Age-dependent bupivacaine-induced muscle toxicity during continuous peripheral nerve block in rats". Anesthesiology. 111 (5): 1120–7. doi:10.1097/ALN.0b013e3181bbc949. PMID 19809284.
- ^ Bogatch MT, Ferachi DG, Kyle B, Popinchalk S, Howell MH, Ge D, You Z, Savoie FH (March 2010). "Is chemical incompatibility responsible for chondrocyte death induced by local anesthetics?". The American Journal of Sports Medicine. 38 (3): 520–6. doi:10.1177/0363546509349799. PMID 20194957. S2CID 8766478.
- ^ Padera R, Bellas E, Tse JY, Hao D, Kohane DS (May 2008). "Local Myotoxicity from Sustained Release of Bupivacaine from Microparticles". Anesthesiology. 108 (5): 921–8. doi:10.1097/ALN.0b013e31816c8a48. PMC 3939710. PMID 18431129.
- ^ Gabliks J, Barter S (April–September 1987). "Comparative cytotoxicity of aflatoxin B1 and saxitoxin in cell cultures". Molecular Toxicology. 1 (2–3): 209–16. PMID 3130568.
- ^ Schwartz DM, Duncan KG, Fields HL, Jones MR (October 1998). "Tetrodotoxin: anesthetic activity in the de-epithelialized cornea". Graefe's Archive for Clinical and Experimental Ophthalmology. 236 (10): 790–4. doi:10.1007/s004170050160. PMID 9801896. S2CID 25050842.
- ^ Duncan KG, Duncan JL, Schwartz DM (August 2001). "Saxitoxin: an anesthetic of the deepithelialized rabbit cornea". Cornea. 20 (6): 639–42. doi:10.1097/00003226-200108000-00016. PMID 11473167. S2CID 24304236.
- ^ Padera RF, Tse JY, Bellas E, Kohane DS (December 2006). "Tetrodotoxin for prolonged local anesthesia with minimal myotoxicity". Muscle Nerve. 34 (6): 747–53. doi:10.1002/mus.20618. PMID 16897761. S2CID 22726109.
- ^ Dillane D, Finucane BT (April 2010). "Local anesthetic systemic toxicity". Canadian Journal of Anesthesia. 57 (4): 368–80. doi:10.1007/s12630-010-9275-7. PMID 20151342.
- ^ Neal JM, Bernards CM, Butterworth JF, Di Gregorio G, Drasner K, Hejtmanck MR, Mulroy MF, Rosenquist RW, Weinberg GL (March–April 2010). "ASRA practice advisory on local anesthetic systemic toxicity". Regional Anesthesia and Pain Medicine. 35 (2): 152–61. doi:10.1097/AAP.0b013e3181d22fcd. PMID 20216033. S2CID 8548084.
- ^ Popkiss ME, Horstman DA, Harpur D (June 1979). "Paralytic shellfish poisoning. A report of 17 cases in Cape Town". South African Medical Journal. 55 (25): 1017–23. PMID 573505. (accessed: May 8, 2012)[16]
- ^ Wylie MC, Johnson VM, Carpino E, Mullen K, Hauser K, Nedder A, Kheir JN, Rodriguez-Navarro AJ, Zurakowski D, Berde CB (March 2012). "Respiratory, neuromuscular, and cardiovascular effects of neosaxitoxin in isoflurane-anesthetized sheep". Regional Anesthesia and Pain Medicine. 37 (2): 152–8. doi:10.1097/AAP.0b013e3182424566. PMID 22330260. S2CID 205432781.
- ^ Funari E, Testai E (February 2008). "Human Health Risk Assessment Related to Cyanotoxins Exposure". Critical Reviews in Toxicology. 38 (2): 97–125. doi:10.1080/10408440701749454. PMID 18259982. S2CID 19506251.
- ^ Guay J (December 2009). "Adverse events associated with intravenous regional anesthesia (Bier block): a systematic review of complications". Journal of Clinical Anesthesia. 21 (8): 585–94. doi:10.1016/j.jclinane.2009.01.015. PMID 20122591.
- ^ Guo XT, Uehara A, Ravindran A, Bryant SH, Hall S, Moczydlowski E (December 1987). "Kinetic basis for insensitivity to tetrodotoxin and saxitoxin in sodium channels of canine heart and denervated rat skeletal muscle". Biochemistry. 26 (24): 7546–56. doi:10.1021/bi00398a003. PMID 2447944.
- ^ Sheets MF, Fozzard HA, Lipkind GM, Hanck DA (January 2010). "Sodium channel molecular conformations and antiarrhythmic drug affinity". Trends in Cardiovascular Medicine. 20 (1): 16–21. doi:10.1016/j.tcm.2010.03.002. PMC 2917343. PMID 20685573.
- ^ Templin JS, Wylie MC, Kim JD, Kurgansky KE, Gorski G, Kheir J, Zurakowski D, Corfas G, Berde C (October 2015). "Neosaxitoxin in Rat Sciatic Block: Improved Therapeutic Index Using Combinations with Bupivacaine, with and without Epinephrine". Anesthesiology. 123 (4): 886–98. doi:10.1097/ALN.0000000000000832. PMID 26280473. S2CID 39363279.
- ^ Ip VH, Tsui BC (January 2011). "Novelty without toxicity: a quest for a safer local anesthetic". Canadian Journal of Anesthesia. 58 (1): 8–13. doi:10.1007/s12630-010-9409-y. PMID 21042902.
