Cardiology Presentation
- 1. Cardiology
- 2. Outline • Basic Physiology • Investigations • Hypertension • Angina • Acute Coronary Syndrome • Atrial Fibrillation/Flutter • Heart Block • Heart Failure • DVT/PE • Pericarditis • Infective Endocarditis • Cardiac Tamponade
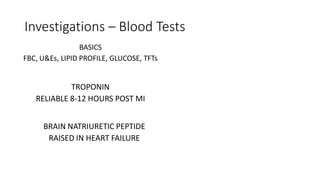
- 4. Investigations – Blood Tests BASICS FBC, U&Es, LIPID PROFILE, GLUCOSE, TFTs TROPONIN RELIABLE 8-12 HOURS POST MI BRAIN NATRIURETIC PEPTIDE RAISED IN HEART FAILURE
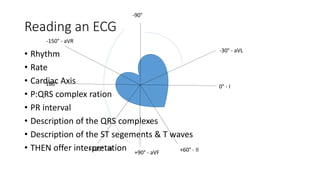
- 6. Reading an ECG • Rhythm • Rate • Cardiac Axis • P:QRS complex ration • PR interval • Description of the QRS complexes • Description of the ST segements & T waves • THEN offer interpretation 0° - I -30° - aVL +60° - II -90° +90° - aVF +120° - III 180° -150° - aVR
- 7. Investigations - Other • Blood Pressure • CXR • Holter Monitor • Stress Testing • Tilt Table Test • CT coronary calcium • Echocardiography • Angiography
- 8. Scoring Systems • TIMI Risk Score • GRACE scoring • CHA2DS2-VASc • Framingham Risk Score • Wells Clinical Prediction for DVT & PE
- 9. Hypertension A 62-year old male attends your GP surgery with concerns about his blood pressure. His father suffered from heart disease and died at 70-years old from a heart attack. He tries to keep as active as possible taking 30- minute walks every day, but does admit to drinking 3 pints of strong beer a day and smoking 5 cigarettes a day for the past 30 years. He accepts his diet probably isn’t the healthiest eating a full English every day for breakfast and snacking regularly throughout the day on chocolate biscuits and crisps, but he feels he needs the energy otherwise he won’t be able to manage his farm. On examination his blood pressure is 152/95. BP TARGETS Clinic BP ABPM/HBPM AGE <80 140/90 135/85 AGE >80 150/90 145/85 Diabetes 130/80 -
- 10. A 47-year old female presents to A&E complaining of chest pain. It started two hours ago when she was out on a jog. It felt like a tight band around her chest and she became short of breath. An ambulance quickly arrived and gave her 300mg aspirin as well as a spray underneath her tongue. The pain quickly subsided and she now feels well at rest. Angina Assessing Risk 10-29% 30-60% 61-90% CT calcium scoring Functional Imaging Coronary Angiography 1.All patients should receive aspirin, a statin and a short-acting nitrate in the absence of a contraindication 2.Use either a beta-blocker or calcium channel blocker first line 3.If poor response to initial treatment increase to maximum tolerated dose 4.After monotherapy use beta-clocker AND calcium channel blocker 5.If neither is tolerated use a long-acting nitrate, ivabradine, nicorandil or ranolazine
- 11. Angina A 60-year old man with stable angina presents for a routine review. He reports he is still symptomatic despite treatment with verapamil. The pain is starting to come on with minimal activity and his functioning is severely impeded. He has a spray which does still help with the symptoms.
- 12. A 56-year old male presents with sharp crushing chest pain that radiates down his left arm. He appears to be cold and clammy and short for breath, although his O2 saturations are stable at 98%. He is tachycardic and hypertensive and reports having a previous diagnosis of Angina. He has been given aspirin and GTN spray but this has not alleviated the symptoms. Acute Coronary Syndrome Unstable Angina NSTEMI STEMI 1. 300mg aspirin and continue indefinitely 2. Offer fondaparinux/unfractionated heparin Use GRACE scoring system Low risk (<1.5%) Low risk (1.5-3%) Intermediate risk (3.0-6.0%) High risk (6.0-9.0%) Highest risk (>9.0%)
- 13. STEMI • M • O • N • A • R • C • H • S -orphine -xygen -itrates -spirin and atenolol -eperfusion and ramipril -lopidogrel -eparin/LMWH -imvastatin Primary Percutaneous Coronary Intervention
- 14. Complications • Cardiac arrest • Cardiogenic shock • Chronic heart failure • Tachyarrhythmias • Bradyarrhythmias • Pericarditis • Left ventricular aneurysm • Left ventricular free wall rupture • Ventricular septal defect • Acute mitral regurgitation
- 15. Secondary Prevention • ACE inhibitor • Beta-blocker • Aspirin • Statin • Clopidogrel (after appropriate risk assessment if NSTEMI or 4 weeks if STEMI)
- 16. Atrial Fibrillation A 72-year old female presents complaining of feeling regularly short of breath and feeling dizzy. She reports that she hasn’t lost consciousness at anytime and that the episodes last only 5 minutes at a time. They are very distressing and she is worried she is going to die when the attack comes on. • What is the extent of the AF? • What lifestyle advice can I give? • What is the stroke risk? • Which drugs do I prescribe? • Does the patient need cardioversion?
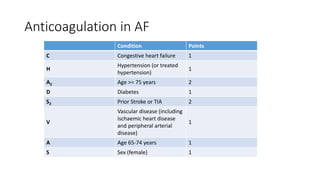
- 17. Anticoagulation in AF Condition Points C Congestive heart failure 1 H Hypertension (or treated hypertension) 1 A2 Age >= 75 years 2 D Diabetes 1 S2 Prior Stroke or TIA 2 V Vascular disease (including ischaemic heart disease and peripheral arterial disease) 1 A Age 65-74 years 1 S Sex (female) 1
- 18. Complications of Atrial Fibrillation •STROKE • Heart failure
- 20. Atrial Flutter • Atrial rate is around 300/min • Heart rate dependent on conduction • 2:1 block heart rate will be 150 • Management same as AF • Medication may be less effective • More sensitive to cardioversion • Radiofrequency ablation of tricuspid valve isthmus is curative for most patients
- 21. A 45-year old male with a BMI of 56 attended his GP surgery today for a nurses appointment. He regularly drinks 12 units a day and smokes 15 cigarettes per day. His diet is high in red meat and his father died of a myocardial infarction at the age of 53. The nurse is alarmed by the appearance of his ECG as shown below. Heart Block First degree Heart blockSecond degree Heart block Mobitz type 1Mobitz type 22:1/3:1 conductionComplete Heart block NEEDS PACEMAKER!!!!!
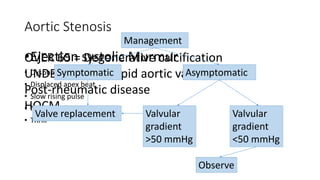
- 24. Aortic Stenosis •Ejection systolic Murmur • Dyspnoea • Displaced apex beat • Slow rising pulse • Narrow pulse pressure • Thrill OVER 65 = Degenerative calcification UNDER 65 = Bicuspid aortic valve Post-rheumatic disease HOCM Management Symptomatic Asymptomatic Valve replacement Valvular gradient >50 mmHg Valvular gradient <50 mmHg Observe
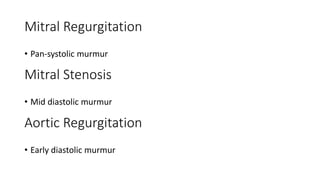
- 25. Mitral Regurgitation • Pan-systolic murmur Mitral Stenosis • Mid diastolic murmur Aortic Regurgitation • Early diastolic murmur
- 26. Heart Failure A 72-year old male with established Atrial Fibrillation presents to the Emergency Department with increasing shortness of breath. He finds he is unable to perform strenuous activities anymore and can struggle with housework on occasion. He does not have any chest pain but has noticed ankle swelling and needs to be propped up on 4 pillows at night when he sleeps. His GP has seen him previously and started him on Simvastatin, Bisoprolol and Ramipril.
- 27. Heart Failure LEFT • Dyspnoea • Orthopnoea • Paroxysmal nocturnal dyspnoea • Wheezing • Dizziness • Confusion RIGHT • Oedema • Nocturia • Ascites LEFT • Displaced apex beat • Gallop rhythm • Heart murmurs RIGHT • Oedema • Hepatomegaly • Raised JVP • Parasternal Heave
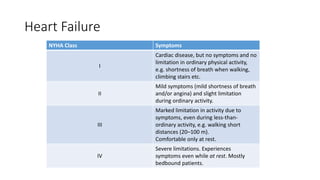
- 28. Heart Failure NYHA Class Symptoms I Cardiac disease, but no symptoms and no limitation in ordinary physical activity, e.g. shortness of breath when walking, climbing stairs etc. II Mild symptoms (mild shortness of breath and/or angina) and slight limitation during ordinary activity. III Marked limitation in activity due to symptoms, even during less-than- ordinary activity, e.g. walking short distances (20–100 m). Comfortable only at rest. IV Severe limitations. Experiences symptoms even while at rest. Mostly bedbound patients.
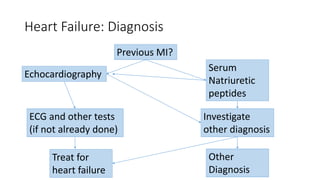
- 29. Heart Failure: Diagnosis Previous MI? Echocardiography Serum Natriuretic peptides ECG and other tests (if not already done) Treat for heart failure Other Diagnosis Investigate other diagnosis
- 30. Treatment of Heart Failure Lifestyle Advice & Vaccination Manage co-morbid conditions ACEi + Beta-blocker ARB if ACEi not tolerated Aldosterone antagonist/ARB/ hydralazine + nitrate Ivabradine/ Cardiac Resynchronisation Therapy alternatives!! Drug treatment for all heart failure Other Interventions Monitoring
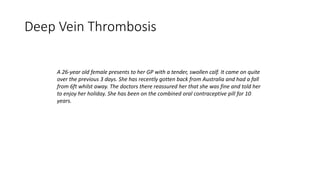
- 31. Deep Vein Thrombosis A 26-year old female presents to her GP with a tender, swollen calf. It came on quite over the previous 3 days. She has recently gotten back from Australia and had a fall from 6ft whilst away. The doctors there reassured her that she was fine and told her to enjoy her holiday. She has been on the combined oral contraceptive pill for 10 years.
- 33. Other things to consider… • Musculoskeletal • Cardiovascular • Other conditions
- 34. Diagnosis Clinical feature Points Active cancer (treatment within 6 months, or palliation) 1 Paralysis, paresis, or immobilization of lower extremity 1 Bedridden for more than 3 days because of surgery (within 4 weeks) 1 Localized tenderness along distribution of deep veins 1 Entire leg swollen 1 Unilateral calf swelling of greater than 3 cm (below tibial tuberosity) 1 Unilateral pitting edema 1 Collateral superficial veins 1 Alternative diagnosis as likely as or more likely than DVT -2 Total points
- 35. Management • ACUTE MANAGEMENT • Warfarin and LMWH • Admit if necessary!!! • CHRONIC MANAGEMENT • Warfarin • Aim for INR 2.5 (between 2-3) • Below-knee compression stockings • Advice
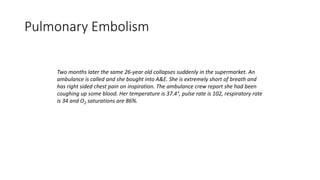
- 36. Pulmonary Embolism Two months later the same 26-year old collapses suddenly in the supermarket. An ambulance is called and she bought into A&E. She is extremely short of breath and has right sided chest pain on inspiration. The ambulance crew report she had been coughing up some blood. Her temperature is 37.4°, pulse rate is 102, respiratory rate is 34 and O2 saturations are 86%.
- 37. Background Information • Lung tissue ventilated but not perfused • Alveolar collapse • Reduction in cross-sectional area of pulmonary arterial bed • Elevation of pulmonary arterial pressure • Reduction in cardiac output • Lung tissue may infarct • Large/multiple emboli can abruptly increase arterial pressure to an afterload level that can’t be matched by the right ventricle • Sudden death may occur due to acute right ventricular failure
- 38. • Annual incidence of 3-4 per 100 000 in the UK • Untreated risk of death is 87% • Treated this falls to 2.3% • Can lead to CHRONIC THOMBOEMBOLIC PULMONARY HYPERTENSION
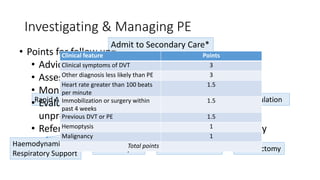
- 39. Investigating & Managing PE Admit to Secondary Care* Confirm PE Rapid Anticoagulation Oral Anticoagulation IF MASSIVE Haemodynamic & Respiratory Support Thrombolysis IVC Filter Insertion Embolectomy • Points for follow up= • Advice & treatment to prevent DVT • Assess risks and benefits of lifelong anticoagulation • Monitor INR • Evaluate and investigate for cancer if the VTE was unprovoked • Refer to specialist if pregnant/considering pregnancy Clinical feature Points Clinical symptoms of DVT 3 Other diagnosis less likely than PE 3 Heart rate greater than 100 beats per minute 1.5 Immobilization or surgery within past 4 weeks 1.5 Previous DVT or PE 1.5 Hemoptysis 1 Malignancy 1 Total points
- 40. Pericarditis A 41-year old man is admitted with left-sided pleuritic chest pain. He has a dry cough and reports that the pain is relieved by sitting forward. For the past three days he has been experiencing flu-like symptoms. His temperature is 38°C and you notice oedema in his legs.
- 41. ECG findings
- 42. Acute • Infective • NSAIDs • Antibiotics if indicated Chronic • Radio/chemotherap y • Autoimmune disorders • Treatment depends on underlying cause Recurring • Addition of colchicine can help prevent symptoms returning
- 43. Infective Endocarditis A 27-year old male, a known IV drug abuser, presents to A&E with muscle aches, lethargy, and pleuritic chest pain. He reports feeling ‘fluey’ for a long time previously and having drastic weight loss. Examination of his heart reveals a new murmur.
- 45. • F • R • O • M • J • A • N • E ever oth spots sler nodes urmur aneway lesions nemia ail haemorrhage mboli
- 46. Modified Duke Criteria • Pathological criteria • Positive histology/microbiology sample obtained at autopsy or cardiac surgery • Major criteria • Positive blood cultures • Evidence of endocardial involvement • Minor criteria • Predisposing heart condition or IV drug use • Microbiological evidence does not meet major criteria • Fever >38°C • Vascular phenomena • Immunological phenomena
- 47. Cardiac Tamponade • RARE • LETHAL • SYMPTOMS VERY WITH UNDERLYING CAUSE AND SPEED OF ONSET • Management = ABCs, Referral to Senior Physician for Pericardiocentesis Cardiac tamponade Constrictive pericarditis JVP Absent Y descent X + Y present Pulsus paradoxus Present Absent Kussmaul's sign Rare Present Characteristic features Pericardial calcification on CXR
Editor's Notes
- Holter Monitor = 24 hour ECG tape Cardiac stress test = ECG + blood pressure monitoring on treadmill. Can be combined with echocardiography or nuclear imaging (thalidomide) to assess blood flow to the heart. CT coronary calcium – identifies extent of calcified plaque in coronary arteries. Use in patients with 10-29% risk of having Coronary Artery Disease
- TIMI identifies % risk at 14 days of all-cause mortality, new/recurrent MI or severe recurrent ischaemia GRACE scoring identifies probability of Death or Death/MI in hospital or at 6 months. CHAD2S2Vasc is probability of a patient with AF having a stroke within a year. Framingham Risk Score estimates the 10-year cardiovascular risk Wells Clinical Score indicates likelihood of DVT or PE at that time
- Classify hypertension into stages. Stage 1 = Clinic BP >= 140/90 and subsequent ABPM average 135/85. Stage 2 = +10 for clinic BP and +15 for ABPM. Severe = clinc systolic >=180 or diastolic >= 110. FIRST STEP = offer ambulatory/home blood pressure monitoring. LIFESTYLE INTERVENTIONS:- diet & exercise, alcohol, caffeine, salt intake, smoking, local initiatives, relaxation therapies Diuretic – use chlorthalidone or indapamide. STEP 4:- DIURETIC TREATMENT FIRST:- if K+ <4.5 use spironolactone 25mg OD. If K+>4.5 add higher dose thiazide. If not tolerated, contraindicated or ineffective add alpha or beta blocker.
- FIRST – ABC approach and rule out acute coronary syndrome (troponin and ECG) Risk of CAD – age, sex and type of angina. Rule out other causes of chest pain
- Verapamil CAN’T be given with a beta blocker. Risk of heart failure. Diltiazem used with caution (risk of AV block) Must give amlodipine/felodipine. Isosorbide mononitrate.
- Low risk = initial conservative management Low risk (>1.5-3.0%) = 300mg clopidorel and continue for 12 months) THEN if recurrent ischaemia coronary angiography Intermediate and above = 300mg clopidogrel and continue for 12 months. Add a glycoprotein inhibitor (tirofiban or eptifabatide). Bvalirudin as an alternative to combination heparin therapy. Coronary angiography (with PCI if indicated) within 96 hours. Discuss with cardiologist then do either CABG or PCI or conservative if indicated.
- Dressler’s syndrome:- occurs 2-6 weeks post MI. Autoimmune reaction against antigenic proteins. Fever, pleuritic pain, pericardial effusion and raised ESR. Treated with NSAIDs. Aneurysm = persistent ST elevation and left ventricular failure Free wall rupture:- seen 1-2 weeks afterwards present with acte heart failure and cardiac tamponade. VSD = acute heart failure with pan systolic murmur.
- Rate control = beta-blockers, calcium channel blockers, digoxin Rhythm control = amiodarone if structural heart disease, fleicanide if no structural heart disease Anticoagulation & cardioversion: if onset >48 hours anticoagulate 3 weeks prior to cardioversion and 4 weeks after.
- No specific treatment for RBBB LBBB may be caused my ischaemia or aortic stenosis. Treat underlying cause.
- Due to accessory pathway – bundle of kent Treatment = cardioversion. Electrical if haemodynamically unstable. Pharmacological if stable. Radiofrequency catheter ablation.
- Smoking, alcohol, sexual activity, flying, driving Yearly influenza vaccines & one-off pneumococcal vaccine Ivabradine used ONLY in NYHA II-IV, HR >75, with LV ejection fraction <35%. MUST have been stable on aldosterone antagonist, ACEi & beta-blockers DRUG Treatment = diuretics (frusemide), amlodipine, anticoagulants (for sinus rhythym with history of thromboembolism, left ventricular aneurysm, intracardiac thrombus), aspirin 75-150mg daily, POSITIVE inotropic agents (dobutamine/milrinone), amiodarone (ONLY AFTER SPECIALIST CONSULTATION) Other interventions = implantable defibrillator, valve replacements Monitoring = Medication reviews, cardiac function reviews, monitor U&Es, serum creatinine, & eGFR. Consider monitoring BNP in hospital or if drug treatment is difficult. Serum digoxin 8-12 hours post-last dose if toxicity suspected.
- Haemodynamic changes = venous stasis, mitral stenosis/varicose veins Endothelial injury/dysfunction = hypertension, chronic inflammation, bacteria Hypercoagulability = hyperviscosity, antithrombin III deficiency, nephrotic syndrome, trauma, cancer, pregnancy, race, age, smoker, obesity
- MSK = calf muscle tear/strain, haematoma, sprain or rupture of tendon, fracture CVS = superficial thrombophlebitis, Post-thrombotic syndrome, Venous obstruction, Vasculitis, Heart Failure Other = Ruptured Baker’s cyst, cellulitis, dependent oedema, lymphatic obstruction, septic arthritis, cirrhosis, nephrotic syndrome
- Refer for same-day assessment if pregnant/in the puerperium/IV drug user/no d-dimer test available If LIKELY to have DVT (Wells Score of 2 or more) refer for same-day assessment/management If UNLIKELY to have DVT take blood sample for D-dimer testing
- Admission criteria = patient at enhanced risk of bleeding, IV drug abuser, dementia, PE, bilateral DVT, pregnant Engage in regular walking exercise, elevate leg when sitting, extended travel should be delayed for 2 weeks after starting treatment
- CTEPH occurs in 0.5-5% of people. Emboli replaced over months or years by fibrous tissue
- Well Score = <2: low risk (3.4%). 2-6: moderate risk (27.8%). >6 points: high risk (78.4%) *Unless d-dimer test result could be available immediately D-dimer testing, CXR & ECG to exclude alternatives, ABG, CTPA, VQ scan, lower limb compression venous ultrasound ECHOCARDIOGRAPHY IF HYPOTENSIVE, absence of RHF excludes PE
- Relatively common – 5% of all A&E admissions are pericarditis.
- Diffuse st segment elevation “saddle changes” PR depression
- Two types of recurring: incessant = once NSAIDs withdrawn symptoms return. Intermittent = long gaps between symptoms
- Staph aureus – 30% of IE associated with prosthetic valves. Most common cause overall. HIGH MORTALITY. Streptococci:- Viridans = 50-60% of subacute IE cases Group D strep = subacute and 3rd most common cause Intermedius = 15% of all cases of IE A,C & G strep = high mortality Group B strep = acute disease, high mortality. Occurs in pregnancy and elderly.
- Blood cultures = consistent with infective endocarditis e.g. STREP VIRIDANS and the HACEK group. Persistent staphu aureus/epidemidis bacteraemia. Positive serology for coxielle burnetti, bartonella or chlamydia psittaci. Positive molecular assays for gene targets Evidence of endocardial involvement = positive echocardiogram or new valvular regurgitations. MANAGEMENT = ADMIT. Empirical therapy = amoxicillin and gentamicin/vancomycin and gentamicin and rifampicin (if prostetic valve/penicillin allergic) Staph = flucloxacillin Streptococci = benzylpenicillin Prosthetic valve = benzylpenicillin + gentimicin ALWAYS FOLLOW LOCAL GUIDELINES