EP2631245A1 - Chimeric factor H binding proteins (fHBP) containing a heterologous B domain and methods of use - Google Patents
Chimeric factor H binding proteins (fHBP) containing a heterologous B domain and methods of use Download PDFInfo
- Publication number
- EP2631245A1 EP2631245A1 EP13154049.4A EP13154049A EP2631245A1 EP 2631245 A1 EP2631245 A1 EP 2631245A1 EP 13154049 A EP13154049 A EP 13154049A EP 2631245 A1 EP2631245 A1 EP 2631245A1
- Authority
- EP
- European Patent Office
- Prior art keywords
- fhbp
- domain
- amino acid
- chimeric
- jar
- Prior art date
- Legal status (The legal status is an assumption and is not a legal conclusion. Google has not performed a legal analysis and makes no representation as to the accuracy of the status listed.)
- Withdrawn
Links
- 238000000034 method Methods 0.000 title claims abstract description 54
- 101710186862 Factor H binding protein Proteins 0.000 title claims description 638
- 230000000844 anti-bacterial effect Effects 0.000 claims abstract description 77
- 241000588650 Neisseria meningitidis Species 0.000 claims abstract description 71
- 238000009739 binding Methods 0.000 claims description 65
- 230000027455 binding Effects 0.000 claims description 64
- 210000004027 cell Anatomy 0.000 claims description 63
- 239000000203 mixture Substances 0.000 claims description 61
- 230000014509 gene expression Effects 0.000 claims description 55
- 150000007523 nucleic acids Chemical class 0.000 claims description 47
- 150000001413 amino acids Chemical group 0.000 claims description 41
- 108020004707 nucleic acids Proteins 0.000 claims description 41
- 102000039446 nucleic acids Human genes 0.000 claims description 41
- 238000006467 substitution reaction Methods 0.000 claims description 35
- 125000001429 N-terminal alpha-amino-acid group Chemical group 0.000 claims description 11
- 230000002163 immunogen Effects 0.000 claims description 11
- 241000124008 Mammalia Species 0.000 claims description 9
- 238000002360 preparation method Methods 0.000 claims description 9
- KZSNJWFQEVHDMF-UHFFFAOYSA-N Valine Natural products CC(C)C(N)C(O)=O KZSNJWFQEVHDMF-UHFFFAOYSA-N 0.000 claims description 8
- 125000001433 C-terminal amino-acid group Chemical group 0.000 claims description 7
- 235000004279 alanine Nutrition 0.000 claims description 7
- 239000000546 pharmaceutical excipient Substances 0.000 claims description 7
- 239000004474 valine Substances 0.000 claims description 7
- 239000004475 Arginine Substances 0.000 claims description 6
- WHUUTDBJXJRKMK-UHFFFAOYSA-N Glutamic acid Natural products OC(=O)C(N)CCC(O)=O WHUUTDBJXJRKMK-UHFFFAOYSA-N 0.000 claims description 6
- QNAYBMKLOCPYGJ-REOHCLBHSA-N L-alanine Chemical compound C[C@H](N)C(O)=O QNAYBMKLOCPYGJ-REOHCLBHSA-N 0.000 claims description 6
- CKLJMWTZIZZHCS-REOHCLBHSA-N L-aspartic acid Chemical compound OC(=O)[C@@H](N)CC(O)=O CKLJMWTZIZZHCS-REOHCLBHSA-N 0.000 claims description 6
- MTCFGRXMJLQNBG-UHFFFAOYSA-N Serine Natural products OCC(N)C(O)=O MTCFGRXMJLQNBG-UHFFFAOYSA-N 0.000 claims description 6
- ODKSFYDXXFIFQN-UHFFFAOYSA-N arginine Natural products OC(=O)C(N)CCCNC(N)=N ODKSFYDXXFIFQN-UHFFFAOYSA-N 0.000 claims description 6
- HNDVDQJCIGZPNO-YFKPBYRVSA-N L-histidine Chemical compound OC(=O)[C@@H](N)CC1=CN=CN1 HNDVDQJCIGZPNO-YFKPBYRVSA-N 0.000 claims description 5
- AGPKZVBTJJNPAG-WHFBIAKZSA-N L-isoleucine Chemical compound CC[C@H](C)[C@H](N)C(O)=O AGPKZVBTJJNPAG-WHFBIAKZSA-N 0.000 claims description 5
- COLNVLDHVKWLRT-QMMMGPOBSA-N L-phenylalanine Chemical compound OC(=O)[C@@H](N)CC1=CC=CC=C1 COLNVLDHVKWLRT-QMMMGPOBSA-N 0.000 claims description 5
- KZSNJWFQEVHDMF-BYPYZUCNSA-N L-valine Chemical compound CC(C)[C@H](N)C(O)=O KZSNJWFQEVHDMF-BYPYZUCNSA-N 0.000 claims description 5
- 235000003704 aspartic acid Nutrition 0.000 claims description 5
- OQFSQFPPLPISGP-UHFFFAOYSA-N beta-carboxyaspartic acid Natural products OC(=O)C(N)C(C(O)=O)C(O)=O OQFSQFPPLPISGP-UHFFFAOYSA-N 0.000 claims description 5
- 238000012258 culturing Methods 0.000 claims description 5
- 235000013922 glutamic acid Nutrition 0.000 claims description 5
- 239000004220 glutamic acid Substances 0.000 claims description 5
- ZDXPYRJPNDTMRX-UHFFFAOYSA-N glutamine Natural products OC(=O)C(N)CCC(N)=O ZDXPYRJPNDTMRX-UHFFFAOYSA-N 0.000 claims description 5
- 125000001909 leucine group Chemical class [H]N(*)C(C(*)=O)C([H])([H])C(C([H])([H])[H])C([H])([H])[H] 0.000 claims description 5
- ROHFNLRQFUQHCH-UHFFFAOYSA-N Leucine Natural products CC(C)CC(N)C(O)=O ROHFNLRQFUQHCH-UHFFFAOYSA-N 0.000 claims description 4
- HNDVDQJCIGZPNO-UHFFFAOYSA-N histidine Natural products OC(=O)C(N)CC1=CN=CN1 HNDVDQJCIGZPNO-UHFFFAOYSA-N 0.000 claims description 4
- AGPKZVBTJJNPAG-UHFFFAOYSA-N isoleucine Natural products CCC(C)C(N)C(O)=O AGPKZVBTJJNPAG-UHFFFAOYSA-N 0.000 claims description 4
- 229960000310 isoleucine Drugs 0.000 claims description 4
- COLNVLDHVKWLRT-UHFFFAOYSA-N phenylalanine Natural products OC(=O)C(N)CC1=CC=CC=C1 COLNVLDHVKWLRT-UHFFFAOYSA-N 0.000 claims description 4
- ONIBWKKTOPOVIA-UHFFFAOYSA-N Proline Natural products OC(=O)C1CCCN1 ONIBWKKTOPOVIA-UHFFFAOYSA-N 0.000 claims description 3
- 238000002255 vaccination Methods 0.000 claims description 3
- 150000003680 valines Chemical class 0.000 claims description 2
- 125000003275 alpha amino acid group Chemical group 0.000 description 233
- 108090000623 proteins and genes Proteins 0.000 description 137
- 102000004169 proteins and genes Human genes 0.000 description 89
- 235000018102 proteins Nutrition 0.000 description 87
- 210000004899 c-terminal region Anatomy 0.000 description 67
- 229960005486 vaccine Drugs 0.000 description 62
- 102000004196 processed proteins & peptides Human genes 0.000 description 57
- 108090000765 processed proteins & peptides Proteins 0.000 description 57
- 229920001184 polypeptide Polymers 0.000 description 54
- 238000004519 manufacturing process Methods 0.000 description 43
- 235000001014 amino acid Nutrition 0.000 description 37
- 230000000890 antigenic effect Effects 0.000 description 35
- 241000699670 Mus sp. Species 0.000 description 34
- 239000000427 antigen Substances 0.000 description 34
- 102000036639 antigens Human genes 0.000 description 34
- 108091007433 antigens Proteins 0.000 description 34
- 230000000875 corresponding effect Effects 0.000 description 30
- 229940024606 amino acid Drugs 0.000 description 29
- 239000013612 plasmid Substances 0.000 description 28
- DHMQDGOQFOQNFH-UHFFFAOYSA-N Glycine Chemical compound NCC(O)=O DHMQDGOQFOQNFH-UHFFFAOYSA-N 0.000 description 27
- 241000588724 Escherichia coli Species 0.000 description 22
- 125000000539 amino acid group Chemical group 0.000 description 22
- 239000012528 membrane Substances 0.000 description 22
- 239000002671 adjuvant Substances 0.000 description 21
- 210000002966 serum Anatomy 0.000 description 21
- 239000013598 vector Substances 0.000 description 21
- 230000005875 antibody response Effects 0.000 description 20
- 241000282414 Homo sapiens Species 0.000 description 19
- 230000001580 bacterial effect Effects 0.000 description 19
- 239000002775 capsule Substances 0.000 description 19
- 102000037865 fusion proteins Human genes 0.000 description 19
- 108020001507 fusion proteins Proteins 0.000 description 19
- 238000001262 western blot Methods 0.000 description 19
- 230000002950 deficient Effects 0.000 description 17
- 102000054765 polymorphisms of proteins Human genes 0.000 description 17
- 241001212279 Neisseriales Species 0.000 description 16
- 108010076504 Protein Sorting Signals Proteins 0.000 description 16
- 239000002158 endotoxin Substances 0.000 description 16
- WNROFYMDJYEPJX-UHFFFAOYSA-K aluminium hydroxide Chemical compound [OH-].[OH-].[OH-].[Al+3] WNROFYMDJYEPJX-UHFFFAOYSA-K 0.000 description 15
- 238000002965 ELISA Methods 0.000 description 14
- 239000004471 Glycine Substances 0.000 description 14
- 201000010099 disease Diseases 0.000 description 14
- 208000037265 diseases, disorders, signs and symptoms Diseases 0.000 description 14
- 230000004048 modification Effects 0.000 description 14
- 238000012986 modification Methods 0.000 description 14
- KDXKERNSBIXSRK-UHFFFAOYSA-N Lysine Natural products NCCCCC(N)C(O)=O KDXKERNSBIXSRK-UHFFFAOYSA-N 0.000 description 13
- 239000002773 nucleotide Substances 0.000 description 13
- 125000003729 nucleotide group Chemical group 0.000 description 13
- 241000894006 Bacteria Species 0.000 description 12
- 239000004472 Lysine Substances 0.000 description 12
- 150000004676 glycans Chemical class 0.000 description 12
- 230000003053 immunization Effects 0.000 description 12
- 238000002649 immunization Methods 0.000 description 12
- 229920001282 polysaccharide Polymers 0.000 description 12
- 239000005017 polysaccharide Substances 0.000 description 12
- 239000000463 material Substances 0.000 description 11
- 230000010807 negative regulation of binding Effects 0.000 description 11
- 230000001681 protective effect Effects 0.000 description 11
- 230000002829 reductive effect Effects 0.000 description 11
- 108010084884 GDP-mannose transporter Proteins 0.000 description 10
- 108010093488 His-His-His-His-His-His Proteins 0.000 description 10
- KDXKERNSBIXSRK-YFKPBYRVSA-N L-lysine Chemical compound NCCCC[C@H](N)C(O)=O KDXKERNSBIXSRK-YFKPBYRVSA-N 0.000 description 10
- 208000002352 blister Diseases 0.000 description 10
- 230000002068 genetic effect Effects 0.000 description 10
- GZQKNULLWNGMCW-PWQABINMSA-N lipid A (E. coli) Chemical compound O1[C@H](CO)[C@@H](OP(O)(O)=O)[C@H](OC(=O)C[C@@H](CCCCCCCCCCC)OC(=O)CCCCCCCCCCCCC)[C@@H](NC(=O)C[C@@H](CCCCCCCCCCC)OC(=O)CCCCCCCCCCC)[C@@H]1OC[C@@H]1[C@@H](O)[C@H](OC(=O)C[C@H](O)CCCCCCCCCCC)[C@@H](NC(=O)C[C@H](O)CCCCCCCCCCC)[C@@H](OP(O)(O)=O)O1 GZQKNULLWNGMCW-PWQABINMSA-N 0.000 description 10
- 239000006166 lysate Substances 0.000 description 10
- 230000009257 reactivity Effects 0.000 description 10
- 230000004044 response Effects 0.000 description 10
- 238000012360 testing method Methods 0.000 description 10
- 241000588653 Neisseria Species 0.000 description 9
- 102000007056 Recombinant Fusion Proteins Human genes 0.000 description 9
- 108010008281 Recombinant Fusion Proteins Proteins 0.000 description 9
- 230000015572 biosynthetic process Effects 0.000 description 9
- 230000000295 complement effect Effects 0.000 description 9
- 230000003247 decreasing effect Effects 0.000 description 9
- 239000003599 detergent Substances 0.000 description 9
- 210000004408 hybridoma Anatomy 0.000 description 9
- 229930182817 methionine Natural products 0.000 description 9
- 239000000523 sample Substances 0.000 description 9
- 150000001875 compounds Chemical class 0.000 description 8
- 230000004927 fusion Effects 0.000 description 8
- 229920006008 lipopolysaccharide Polymers 0.000 description 8
- 125000001360 methionine group Chemical group N[C@@H](CCSC)C(=O)* 0.000 description 8
- 229940035032 monophosphoryl lipid a Drugs 0.000 description 8
- 239000000243 solution Substances 0.000 description 8
- 102000004190 Enzymes Human genes 0.000 description 7
- 108090000790 Enzymes Proteins 0.000 description 7
- 108091028043 Nucleic acid sequence Proteins 0.000 description 7
- FAPWRFPIFSIZLT-UHFFFAOYSA-M Sodium chloride Chemical compound [Na+].[Cl-] FAPWRFPIFSIZLT-UHFFFAOYSA-M 0.000 description 7
- 229940088598 enzyme Drugs 0.000 description 7
- 238000009396 hybridization Methods 0.000 description 7
- 230000028993 immune response Effects 0.000 description 7
- 230000036039 immunity Effects 0.000 description 7
- 239000002953 phosphate buffered saline Substances 0.000 description 7
- 239000000047 product Substances 0.000 description 7
- 238000000746 purification Methods 0.000 description 7
- 108020004414 DNA Proteins 0.000 description 6
- 102000004895 Lipoproteins Human genes 0.000 description 6
- 108090001030 Lipoproteins Proteins 0.000 description 6
- 241000699666 Mus <mouse, genus> Species 0.000 description 6
- 241000588677 Neisseria meningitidis serogroup B Species 0.000 description 6
- 241000283973 Oryctolagus cuniculus Species 0.000 description 6
- 230000008859 change Effects 0.000 description 6
- PRAKJMSDJKAYCZ-UHFFFAOYSA-N dodecahydrosqualene Natural products CC(C)CCCC(C)CCCC(C)CCCCC(C)CCCC(C)CCCC(C)C PRAKJMSDJKAYCZ-UHFFFAOYSA-N 0.000 description 6
- 239000013604 expression vector Substances 0.000 description 6
- 238000009472 formulation Methods 0.000 description 6
- 208000015181 infectious disease Diseases 0.000 description 6
- 230000035772 mutation Effects 0.000 description 6
- 230000036961 partial effect Effects 0.000 description 6
- 230000001717 pathogenic effect Effects 0.000 description 6
- 230000001105 regulatory effect Effects 0.000 description 6
- 238000002741 site-directed mutagenesis Methods 0.000 description 6
- 208000024891 symptom Diseases 0.000 description 6
- DRHZYJAUECRAJM-DWSYSWFDSA-N (2s,3s,4s,5r,6r)-6-[[(3s,4s,4ar,6ar,6bs,8r,8ar,12as,14ar,14br)-8a-[(2s,3r,4s,5r,6r)-3-[(2s,3r,4s,5r,6s)-5-[(2s,3r,4s,5r)-4-[(2s,3r,4r)-3,4-dihydroxy-4-(hydroxymethyl)oxolan-2-yl]oxy-3,5-dihydroxyoxan-2-yl]oxy-3,4-dihydroxy-6-methyloxan-2-yl]oxy-5-[(3s,5s, Chemical compound O([C@H]1[C@H](O)[C@H](O[C@H]([C@@H]1O[C@H]1[C@@H]([C@@H](O)[C@@H](O)[C@@H](CO)O1)O)O[C@H]1CC[C@]2(C)[C@H]3CC=C4[C@@H]5CC(C)(C)CC[C@@]5([C@@H](C[C@@]4(C)[C@]3(C)CC[C@H]2[C@@]1(C=O)C)O)C(=O)O[C@@H]1O[C@H](C)[C@@H]([C@@H]([C@H]1O[C@H]1[C@@H]([C@H](O)[C@@H](O[C@H]2[C@@H]([C@@H](O[C@H]3[C@@H]([C@@](O)(CO)CO3)O)[C@H](O)CO2)O)[C@H](C)O1)O)O)OC(=O)C[C@@H](O)C[C@H](OC(=O)C[C@@H](O)C[C@@H]([C@@H](C)CC)O[C@H]1[C@@H]([C@@H](O)[C@H](CO)O1)O)[C@@H](C)CC)C(O)=O)[C@@H]1OC[C@@H](O)[C@H](O)[C@H]1O DRHZYJAUECRAJM-DWSYSWFDSA-N 0.000 description 5
- 108010039939 Cell Wall Skeleton Proteins 0.000 description 5
- 241000282412 Homo Species 0.000 description 5
- ZDXPYRJPNDTMRX-VKHMYHEASA-N L-glutamine Chemical compound OC(=O)[C@@H](N)CCC(N)=O ZDXPYRJPNDTMRX-VKHMYHEASA-N 0.000 description 5
- 238000003556 assay Methods 0.000 description 5
- SQVRNKJHWKZAKO-UHFFFAOYSA-N beta-N-Acetyl-D-neuraminic acid Natural products CC(=O)NC1C(O)CC(O)(C(O)=O)OC1C(O)C(O)CO SQVRNKJHWKZAKO-UHFFFAOYSA-N 0.000 description 5
- 210000004520 cell wall skeleton Anatomy 0.000 description 5
- 239000013522 chelant Substances 0.000 description 5
- 238000004587 chromatography analysis Methods 0.000 description 5
- 230000009260 cross reactivity Effects 0.000 description 5
- 230000001419 dependent effect Effects 0.000 description 5
- 238000012239 gene modification Methods 0.000 description 5
- 230000005017 genetic modification Effects 0.000 description 5
- 235000013617 genetically modified food Nutrition 0.000 description 5
- 239000001963 growth medium Substances 0.000 description 5
- 238000002955 isolation Methods 0.000 description 5
- 239000003550 marker Substances 0.000 description 5
- 230000001404 mediated effect Effects 0.000 description 5
- 229910052751 metal Inorganic materials 0.000 description 5
- 239000002184 metal Substances 0.000 description 5
- -1 periplasmic space Substances 0.000 description 5
- 108091033319 polynucleotide Proteins 0.000 description 5
- 102000040430 polynucleotide Human genes 0.000 description 5
- 239000002157 polynucleotide Substances 0.000 description 5
- 235000010482 polyoxyethylene sorbitan monooleate Nutrition 0.000 description 5
- 229920000053 polysorbate 80 Polymers 0.000 description 5
- 238000010188 recombinant method Methods 0.000 description 5
- SQVRNKJHWKZAKO-OQPLDHBCSA-N sialic acid Chemical compound CC(=O)N[C@@H]1[C@@H](O)C[C@@](O)(C(O)=O)OC1[C@H](O)[C@H](O)CO SQVRNKJHWKZAKO-OQPLDHBCSA-N 0.000 description 5
- 239000000126 substance Substances 0.000 description 5
- 230000002588 toxic effect Effects 0.000 description 5
- 231100000419 toxicity Toxicity 0.000 description 5
- 230000001988 toxicity Effects 0.000 description 5
- 230000002103 transcriptional effect Effects 0.000 description 5
- YBJHBAHKTGYVGT-ZKWXMUAHSA-N (+)-Biotin Chemical compound N1C(=O)N[C@@H]2[C@H](CCCCC(=O)O)SC[C@@H]21 YBJHBAHKTGYVGT-ZKWXMUAHSA-N 0.000 description 4
- MTCFGRXMJLQNBG-REOHCLBHSA-N (2S)-2-Amino-3-hydroxypropansäure Chemical compound OC[C@H](N)C(O)=O MTCFGRXMJLQNBG-REOHCLBHSA-N 0.000 description 4
- NFFPKRVXIPSSQR-JJYYJPOSSA-N (2s,3r,4r)-2,3,4,5-tetrahydroxypentanamide Chemical compound NC(=O)[C@@H](O)[C@H](O)[C@H](O)CO NFFPKRVXIPSSQR-JJYYJPOSSA-N 0.000 description 4
- YYGNTYWPHWGJRM-UHFFFAOYSA-N (6E,10E,14E,18E)-2,6,10,15,19,23-hexamethyltetracosa-2,6,10,14,18,22-hexaene Chemical compound CC(C)=CCCC(C)=CCCC(C)=CCCC=C(C)CCC=C(C)CCC=C(C)C YYGNTYWPHWGJRM-UHFFFAOYSA-N 0.000 description 4
- 108091026890 Coding region Proteins 0.000 description 4
- ODKSFYDXXFIFQN-BYPYZUCNSA-P L-argininium(2+) Chemical compound NC(=[NH2+])NCCC[C@H]([NH3+])C(O)=O ODKSFYDXXFIFQN-BYPYZUCNSA-P 0.000 description 4
- 241001465754 Metazoa Species 0.000 description 4
- 241000040340 Oat mosaic virus Species 0.000 description 4
- 108091034117 Oligonucleotide Proteins 0.000 description 4
- 229930006000 Sucrose Natural products 0.000 description 4
- CZMRCDWAGMRECN-UGDNZRGBSA-N Sucrose Chemical compound O[C@H]1[C@H](O)[C@@H](CO)O[C@@]1(CO)O[C@@H]1[C@H](O)[C@@H](O)[C@H](O)[C@@H](CO)O1 CZMRCDWAGMRECN-UGDNZRGBSA-N 0.000 description 4
- BHEOSNUKNHRBNM-UHFFFAOYSA-N Tetramethylsqualene Natural products CC(=C)C(C)CCC(=C)C(C)CCC(C)=CCCC=C(C)CCC(C)C(=C)CCC(C)C(C)=C BHEOSNUKNHRBNM-UHFFFAOYSA-N 0.000 description 4
- 238000013459 approach Methods 0.000 description 4
- 238000006243 chemical reaction Methods 0.000 description 4
- 235000018417 cysteine Nutrition 0.000 description 4
- XUJNEKJLAYXESH-UHFFFAOYSA-N cysteine Natural products SCC(N)C(O)=O XUJNEKJLAYXESH-UHFFFAOYSA-N 0.000 description 4
- CTMZLDSMFCVUNX-VMIOUTBZSA-N cytidylyl-(3'->5')-guanosine Chemical compound O=C1N=C(N)C=CN1[C@H]1[C@H](O)[C@H](OP(O)(=O)OC[C@@H]2[C@H]([C@@H](O)[C@@H](O2)N2C3=C(C(N=C(N)N3)=O)N=C2)O)[C@@H](CO)O1 CTMZLDSMFCVUNX-VMIOUTBZSA-N 0.000 description 4
- OPTASPLRGRRNAP-UHFFFAOYSA-N cytosine Chemical compound NC=1C=CNC(=O)N=1 OPTASPLRGRRNAP-UHFFFAOYSA-N 0.000 description 4
- 230000007423 decrease Effects 0.000 description 4
- 238000010790 dilution Methods 0.000 description 4
- 239000012895 dilution Substances 0.000 description 4
- 239000000839 emulsion Substances 0.000 description 4
- 238000000605 extraction Methods 0.000 description 4
- 238000001914 filtration Methods 0.000 description 4
- 239000000499 gel Substances 0.000 description 4
- 230000001900 immune effect Effects 0.000 description 4
- 230000001976 improved effect Effects 0.000 description 4
- 125000003588 lysine group Chemical group [H]N([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])(N([H])[H])C(*)=O 0.000 description 4
- 238000012423 maintenance Methods 0.000 description 4
- 239000002245 particle Substances 0.000 description 4
- 239000008188 pellet Substances 0.000 description 4
- 239000001397 quillaja saponaria molina bark Substances 0.000 description 4
- 230000010076 replication Effects 0.000 description 4
- 229930182490 saponin Natural products 0.000 description 4
- 150000007949 saponins Chemical class 0.000 description 4
- 235000002639 sodium chloride Nutrition 0.000 description 4
- 229940031439 squalene Drugs 0.000 description 4
- TUHBEKDERLKLEC-UHFFFAOYSA-N squalene Natural products CC(=CCCC(=CCCC(=CCCC=C(/C)CCC=C(/C)CC=C(C)C)C)C)C TUHBEKDERLKLEC-UHFFFAOYSA-N 0.000 description 4
- 239000005720 sucrose Substances 0.000 description 4
- 238000003786 synthesis reaction Methods 0.000 description 4
- XETCRXVKJHBPMK-MJSODCSWSA-N trehalose 6,6'-dimycolate Chemical compound C([C@@H]1[C@H]([C@H](O)[C@@H](O)[C@@H](O[C@@H]2[C@@H]([C@@H](O)[C@H](O)[C@@H](COC(=O)C(CCCCCCCCCCC3C(C3)CCCCCCCCCCCCCCCCCC)C(O)CCCCCCCCCCCCCCCCCCCCCCCCC)O2)O)O1)O)OC(=O)C(C(O)CCCCCCCCCCCCCCCCCCCCCCCCC)CCCCCCCCCCC1CC1CCCCCCCCCCCCCCCCCC XETCRXVKJHBPMK-MJSODCSWSA-N 0.000 description 4
- 241001198387 Escherichia coli BL21(DE3) Species 0.000 description 3
- XUJNEKJLAYXESH-REOHCLBHSA-N L-Cysteine Chemical compound SC[C@H](N)C(O)=O XUJNEKJLAYXESH-REOHCLBHSA-N 0.000 description 3
- ROHFNLRQFUQHCH-YFKPBYRVSA-N L-leucine Chemical compound CC(C)C[C@H](N)C(O)=O ROHFNLRQFUQHCH-YFKPBYRVSA-N 0.000 description 3
- 108700020354 N-acetylmuramyl-threonyl-isoglutamine Proteins 0.000 description 3
- 101100203230 Neisseria meningitidis serogroup B (strain MC58) siaA gene Proteins 0.000 description 3
- 229910019142 PO4 Inorganic materials 0.000 description 3
- 229920003171 Poly (ethylene oxide) Polymers 0.000 description 3
- 108010093965 Polymyxin B Proteins 0.000 description 3
- 101710132190 Porin B Proteins 0.000 description 3
- 240000004808 Saccharomyces cerevisiae Species 0.000 description 3
- 206010040047 Sepsis Diseases 0.000 description 3
- 108060008682 Tumor Necrosis Factor Proteins 0.000 description 3
- 238000004458 analytical method Methods 0.000 description 3
- 239000000872 buffer Substances 0.000 description 3
- 238000005119 centrifugation Methods 0.000 description 3
- 239000003795 chemical substances by application Substances 0.000 description 3
- 230000006957 competitive inhibition Effects 0.000 description 3
- 125000000151 cysteine group Chemical group N[C@@H](CS)C(=O)* 0.000 description 3
- KXGVEGMKQFWNSR-LLQZFEROSA-N deoxycholic acid Chemical compound C([C@H]1CC2)[C@H](O)CC[C@]1(C)[C@@H]1[C@@H]2[C@@H]2CC[C@H]([C@@H](CCC(O)=O)C)[C@@]2(C)[C@@H](O)C1 KXGVEGMKQFWNSR-LLQZFEROSA-N 0.000 description 3
- 238000011161 development Methods 0.000 description 3
- 230000000694 effects Effects 0.000 description 3
- 239000012634 fragment Substances 0.000 description 3
- 125000003630 glycyl group Chemical group [H]N([H])C([H])([H])C(*)=O 0.000 description 3
- 239000003022 immunostimulating agent Substances 0.000 description 3
- 230000003308 immunostimulating effect Effects 0.000 description 3
- 238000011534 incubation Methods 0.000 description 3
- 230000005764 inhibitory process Effects 0.000 description 3
- 230000000670 limiting effect Effects 0.000 description 3
- JMUHBNWAORSSBD-WKYWBUFDSA-N mifamurtide Chemical compound CCCCCCCCCCCCCCCC(=O)OC[C@@H](OC(=O)CCCCCCCCCCCCCCC)COP(O)(=O)OCCNC(=O)[C@H](C)NC(=O)CC[C@H](C(N)=O)NC(=O)[C@H](C)NC(=O)[C@@H](C)O[C@H]1[C@H](O)[C@@H](CO)OC(O)[C@@H]1NC(C)=O JMUHBNWAORSSBD-WKYWBUFDSA-N 0.000 description 3
- 229960005225 mifamurtide Drugs 0.000 description 3
- 239000013642 negative control Substances 0.000 description 3
- 239000010452 phosphate Substances 0.000 description 3
- 229920002401 polyacrylamide Polymers 0.000 description 3
- 229920000024 polymyxin B Polymers 0.000 description 3
- 229960005266 polymyxin b Drugs 0.000 description 3
- 229940023143 protein vaccine Drugs 0.000 description 3
- 230000006798 recombination Effects 0.000 description 3
- 238000005215 recombination Methods 0.000 description 3
- 125000003607 serino group Chemical group [H]N([H])[C@]([H])(C(=O)[*])C(O[H])([H])[H] 0.000 description 3
- 239000011780 sodium chloride Substances 0.000 description 3
- 238000002415 sodium dodecyl sulfate polyacrylamide gel electrophoresis Methods 0.000 description 3
- 230000009870 specific binding Effects 0.000 description 3
- 238000012546 transfer Methods 0.000 description 3
- 102000003390 tumor necrosis factor Human genes 0.000 description 3
- 238000005406 washing Methods 0.000 description 3
- YHQZWWDVLJPRIF-JLHRHDQISA-N (4R)-4-[[(2S,3R)-2-[acetyl-[(3R,4R,5S,6R)-3-amino-4-[(1R)-1-carboxyethoxy]-5-hydroxy-6-(hydroxymethyl)oxan-2-yl]amino]-3-hydroxybutanoyl]amino]-5-amino-5-oxopentanoic acid Chemical compound C(C)(=O)N([C@@H]([C@H](O)C)C(=O)N[C@H](CCC(=O)O)C(N)=O)C1[C@H](N)[C@@H](O[C@@H](C(=O)O)C)[C@H](O)[C@H](O1)CO YHQZWWDVLJPRIF-JLHRHDQISA-N 0.000 description 2
- MSWZFWKMSRAUBD-IVMDWMLBSA-N 2-amino-2-deoxy-D-glucopyranose Chemical group N[C@H]1C(O)O[C@H](CO)[C@@H](O)[C@@H]1O MSWZFWKMSRAUBD-IVMDWMLBSA-N 0.000 description 2
- GOJUJUVQIVIZAV-UHFFFAOYSA-N 2-amino-4,6-dichloropyrimidine-5-carbaldehyde Chemical group NC1=NC(Cl)=C(C=O)C(Cl)=N1 GOJUJUVQIVIZAV-UHFFFAOYSA-N 0.000 description 2
- QFVHZQCOUORWEI-UHFFFAOYSA-N 4-[(4-anilino-5-sulfonaphthalen-1-yl)diazenyl]-5-hydroxynaphthalene-2,7-disulfonic acid Chemical compound C=12C(O)=CC(S(O)(=O)=O)=CC2=CC(S(O)(=O)=O)=CC=1N=NC(C1=CC=CC(=C11)S(O)(=O)=O)=CC=C1NC1=CC=CC=C1 QFVHZQCOUORWEI-UHFFFAOYSA-N 0.000 description 2
- 102000002260 Alkaline Phosphatase Human genes 0.000 description 2
- 108020004774 Alkaline Phosphatase Proteins 0.000 description 2
- 238000009631 Broth culture Methods 0.000 description 2
- UXVMQQNJUSDDNG-UHFFFAOYSA-L Calcium chloride Chemical compound [Cl-].[Cl-].[Ca+2] UXVMQQNJUSDDNG-UHFFFAOYSA-L 0.000 description 2
- 102000009016 Cholera Toxin Human genes 0.000 description 2
- 108010049048 Cholera Toxin Proteins 0.000 description 2
- 108020004705 Codon Proteins 0.000 description 2
- 102000016550 Complement Factor H Human genes 0.000 description 2
- 108010053085 Complement Factor H Proteins 0.000 description 2
- 238000001712 DNA sequencing Methods 0.000 description 2
- ULGZDMOVFRHVEP-RWJQBGPGSA-N Erythromycin Chemical compound O([C@@H]1[C@@H](C)C(=O)O[C@@H]([C@@]([C@H](O)[C@@H](C)C(=O)[C@H](C)C[C@@](C)(O)[C@H](O[C@H]2[C@@H]([C@H](C[C@@H](C)O2)N(C)C)O)[C@H]1C)(C)O)CC)[C@H]1C[C@@](C)(OC)[C@@H](O)[C@H](C)O1 ULGZDMOVFRHVEP-RWJQBGPGSA-N 0.000 description 2
- ZHNUHDYFZUAESO-UHFFFAOYSA-N Formamide Chemical compound NC=O ZHNUHDYFZUAESO-UHFFFAOYSA-N 0.000 description 2
- FZHXIRIBWMQPQF-UHFFFAOYSA-N Glc-NH2 Natural products O=CC(N)C(O)C(O)C(O)CO FZHXIRIBWMQPQF-UHFFFAOYSA-N 0.000 description 2
- WQZGKKKJIJFFOK-GASJEMHNSA-N Glucose Natural products OC[C@H]1OC(O)[C@H](O)[C@@H](O)[C@@H]1O WQZGKKKJIJFFOK-GASJEMHNSA-N 0.000 description 2
- 108010070675 Glutathione transferase Proteins 0.000 description 2
- 102000005720 Glutathione transferase Human genes 0.000 description 2
- 241000238631 Hexapoda Species 0.000 description 2
- 108010063738 Interleukins Proteins 0.000 description 2
- 102000015696 Interleukins Human genes 0.000 description 2
- DCXYFEDJOCDNAF-REOHCLBHSA-N L-asparagine Chemical compound OC(=O)[C@@H](N)CC(N)=O DCXYFEDJOCDNAF-REOHCLBHSA-N 0.000 description 2
- AYFVYJQAPQTCCC-GBXIJSLDSA-N L-threonine Chemical compound C[C@@H](O)[C@H](N)C(O)=O AYFVYJQAPQTCCC-GBXIJSLDSA-N 0.000 description 2
- OUYCCCASQSFEME-QMMMGPOBSA-N L-tyrosine Chemical compound OC(=O)[C@@H](N)CC1=CC=C(O)C=C1 OUYCCCASQSFEME-QMMMGPOBSA-N 0.000 description 2
- 102000007651 Macrophage Colony-Stimulating Factor Human genes 0.000 description 2
- 108010046938 Macrophage Colony-Stimulating Factor Proteins 0.000 description 2
- TWRXJAOTZQYOKJ-UHFFFAOYSA-L Magnesium chloride Chemical compound [Mg+2].[Cl-].[Cl-] TWRXJAOTZQYOKJ-UHFFFAOYSA-L 0.000 description 2
- 101710175625 Maltose/maltodextrin-binding periplasmic protein Proteins 0.000 description 2
- 201000009906 Meningitis Diseases 0.000 description 2
- 102000008300 Mutant Proteins Human genes 0.000 description 2
- 108010021466 Mutant Proteins Proteins 0.000 description 2
- 108700015872 N-acetyl-nor-muramyl-L-alanyl-D-isoglutamine Proteins 0.000 description 2
- PXHVJJICTQNCMI-UHFFFAOYSA-N Nickel Chemical compound [Ni] PXHVJJICTQNCMI-UHFFFAOYSA-N 0.000 description 2
- 108700023315 OspC Proteins 0.000 description 2
- 101710116435 Outer membrane protein Proteins 0.000 description 2
- 238000012408 PCR amplification Methods 0.000 description 2
- 102000004160 Phosphoric Monoester Hydrolases Human genes 0.000 description 2
- 108090000608 Phosphoric Monoester Hydrolases Proteins 0.000 description 2
- 229920001213 Polysorbate 20 Polymers 0.000 description 2
- WCUXLLCKKVVCTQ-UHFFFAOYSA-M Potassium chloride Chemical compound [Cl-].[K+] WCUXLLCKKVVCTQ-UHFFFAOYSA-M 0.000 description 2
- PXIPVTKHYLBLMZ-UHFFFAOYSA-N Sodium azide Chemical compound [Na+].[N-]=[N+]=[N-] PXIPVTKHYLBLMZ-UHFFFAOYSA-N 0.000 description 2
- PRXRUNOAOLTIEF-ADSICKODSA-N Sorbitan trioleate Chemical compound CCCCCCCC\C=C/CCCCCCCC(=O)OC[C@@H](OC(=O)CCCCCCC\C=C/CCCCCCCC)[C@H]1OC[C@H](O)[C@H]1OC(=O)CCCCCCC\C=C/CCCCCCCC PRXRUNOAOLTIEF-ADSICKODSA-N 0.000 description 2
- JLCPHMBAVCMARE-UHFFFAOYSA-N [3-[[3-[[3-[[3-[[3-[[3-[[3-[[3-[[3-[[3-[[3-[[5-(2-amino-6-oxo-1H-purin-9-yl)-3-[[3-[[3-[[3-[[3-[[3-[[5-(2-amino-6-oxo-1H-purin-9-yl)-3-[[5-(2-amino-6-oxo-1H-purin-9-yl)-3-hydroxyoxolan-2-yl]methoxy-hydroxyphosphoryl]oxyoxolan-2-yl]methoxy-hydroxyphosphoryl]oxy-5-(5-methyl-2,4-dioxopyrimidin-1-yl)oxolan-2-yl]methoxy-hydroxyphosphoryl]oxy-5-(6-aminopurin-9-yl)oxolan-2-yl]methoxy-hydroxyphosphoryl]oxy-5-(6-aminopurin-9-yl)oxolan-2-yl]methoxy-hydroxyphosphoryl]oxy-5-(6-aminopurin-9-yl)oxolan-2-yl]methoxy-hydroxyphosphoryl]oxy-5-(6-aminopurin-9-yl)oxolan-2-yl]methoxy-hydroxyphosphoryl]oxyoxolan-2-yl]methoxy-hydroxyphosphoryl]oxy-5-(5-methyl-2,4-dioxopyrimidin-1-yl)oxolan-2-yl]methoxy-hydroxyphosphoryl]oxy-5-(4-amino-2-oxopyrimidin-1-yl)oxolan-2-yl]methoxy-hydroxyphosphoryl]oxy-5-(5-methyl-2,4-dioxopyrimidin-1-yl)oxolan-2-yl]methoxy-hydroxyphosphoryl]oxy-5-(5-methyl-2,4-dioxopyrimidin-1-yl)oxolan-2-yl]methoxy-hydroxyphosphoryl]oxy-5-(6-aminopurin-9-yl)oxolan-2-yl]methoxy-hydroxyphosphoryl]oxy-5-(6-aminopurin-9-yl)oxolan-2-yl]methoxy-hydroxyphosphoryl]oxy-5-(4-amino-2-oxopyrimidin-1-yl)oxolan-2-yl]methoxy-hydroxyphosphoryl]oxy-5-(4-amino-2-oxopyrimidin-1-yl)oxolan-2-yl]methoxy-hydroxyphosphoryl]oxy-5-(4-amino-2-oxopyrimidin-1-yl)oxolan-2-yl]methoxy-hydroxyphosphoryl]oxy-5-(6-aminopurin-9-yl)oxolan-2-yl]methoxy-hydroxyphosphoryl]oxy-5-(4-amino-2-oxopyrimidin-1-yl)oxolan-2-yl]methyl [5-(6-aminopurin-9-yl)-2-(hydroxymethyl)oxolan-3-yl] hydrogen phosphate Polymers Cc1cn(C2CC(OP(O)(=O)OCC3OC(CC3OP(O)(=O)OCC3OC(CC3O)n3cnc4c3nc(N)[nH]c4=O)n3cnc4c3nc(N)[nH]c4=O)C(COP(O)(=O)OC3CC(OC3COP(O)(=O)OC3CC(OC3COP(O)(=O)OC3CC(OC3COP(O)(=O)OC3CC(OC3COP(O)(=O)OC3CC(OC3COP(O)(=O)OC3CC(OC3COP(O)(=O)OC3CC(OC3COP(O)(=O)OC3CC(OC3COP(O)(=O)OC3CC(OC3COP(O)(=O)OC3CC(OC3COP(O)(=O)OC3CC(OC3COP(O)(=O)OC3CC(OC3COP(O)(=O)OC3CC(OC3COP(O)(=O)OC3CC(OC3COP(O)(=O)OC3CC(OC3COP(O)(=O)OC3CC(OC3COP(O)(=O)OC3CC(OC3CO)n3cnc4c(N)ncnc34)n3ccc(N)nc3=O)n3cnc4c(N)ncnc34)n3ccc(N)nc3=O)n3ccc(N)nc3=O)n3ccc(N)nc3=O)n3cnc4c(N)ncnc34)n3cnc4c(N)ncnc34)n3cc(C)c(=O)[nH]c3=O)n3cc(C)c(=O)[nH]c3=O)n3ccc(N)nc3=O)n3cc(C)c(=O)[nH]c3=O)n3cnc4c3nc(N)[nH]c4=O)n3cnc4c(N)ncnc34)n3cnc4c(N)ncnc34)n3cnc4c(N)ncnc34)n3cnc4c(N)ncnc34)O2)c(=O)[nH]c1=O JLCPHMBAVCMARE-UHFFFAOYSA-N 0.000 description 2
- 239000000443 aerosol Substances 0.000 description 2
- 230000002776 aggregation Effects 0.000 description 2
- 238000004220 aggregation Methods 0.000 description 2
- 125000003295 alanine group Chemical group N[C@@H](C)C(=O)* 0.000 description 2
- NWMHDZMRVUOQGL-CZEIJOLGSA-N almurtide Chemical compound OC(=O)CC[C@H](C(N)=O)NC(=O)[C@H](C)NC(=O)CO[C@@H]([C@H](O)[C@H](O)CO)[C@@H](NC(C)=O)C=O NWMHDZMRVUOQGL-CZEIJOLGSA-N 0.000 description 2
- 230000004075 alteration Effects 0.000 description 2
- 229940037003 alum Drugs 0.000 description 2
- 230000003321 amplification Effects 0.000 description 2
- 230000001727 anti-capsular Effects 0.000 description 2
- 239000013602 bacteriophage vector Substances 0.000 description 2
- MSWZFWKMSRAUBD-UHFFFAOYSA-N beta-D-galactosamine Natural products NC1C(O)OC(CO)C(O)C1O MSWZFWKMSRAUBD-UHFFFAOYSA-N 0.000 description 2
- 238000013357 binding ELISA Methods 0.000 description 2
- 229960002685 biotin Drugs 0.000 description 2
- 235000020958 biotin Nutrition 0.000 description 2
- 239000011616 biotin Substances 0.000 description 2
- 239000001110 calcium chloride Substances 0.000 description 2
- 229910001628 calcium chloride Inorganic materials 0.000 description 2
- 210000002421 cell wall Anatomy 0.000 description 2
- 239000003153 chemical reaction reagent Substances 0.000 description 2
- 238000005352 clarification Methods 0.000 description 2
- 230000024203 complement activation Effects 0.000 description 2
- 238000010276 construction Methods 0.000 description 2
- 238000007796 conventional method Methods 0.000 description 2
- 229940104302 cytosine Drugs 0.000 description 2
- 229940009976 deoxycholate Drugs 0.000 description 2
- 238000013461 design Methods 0.000 description 2
- 238000010586 diagram Methods 0.000 description 2
- 230000029087 digestion Effects 0.000 description 2
- 239000002552 dosage form Substances 0.000 description 2
- 230000007893 endotoxin activity Effects 0.000 description 2
- 238000005516 engineering process Methods 0.000 description 2
- 150000002148 esters Chemical class 0.000 description 2
- 239000008103 glucose Substances 0.000 description 2
- 230000036541 health Effects 0.000 description 2
- 238000000703 high-speed centrifugation Methods 0.000 description 2
- 238000002744 homologous recombination Methods 0.000 description 2
- 230000006801 homologous recombination Effects 0.000 description 2
- 230000005847 immunogenicity Effects 0.000 description 2
- 238000001114 immunoprecipitation Methods 0.000 description 2
- 238000000338 in vitro Methods 0.000 description 2
- 238000001727 in vivo Methods 0.000 description 2
- 230000001939 inductive effect Effects 0.000 description 2
- 238000002347 injection Methods 0.000 description 2
- 239000007924 injection Substances 0.000 description 2
- 238000003780 insertion Methods 0.000 description 2
- 230000037431 insertion Effects 0.000 description 2
- 230000003993 interaction Effects 0.000 description 2
- 229940047122 interleukins Drugs 0.000 description 2
- 150000002500 ions Chemical class 0.000 description 2
- 150000002632 lipids Chemical group 0.000 description 2
- 239000002502 liposome Substances 0.000 description 2
- 238000000464 low-speed centrifugation Methods 0.000 description 2
- HQKMJHAJHXVSDF-UHFFFAOYSA-L magnesium stearate Chemical compound [Mg+2].CCCCCCCCCCCCCCCCCC([O-])=O.CCCCCCCCCCCCCCCCCC([O-])=O HQKMJHAJHXVSDF-UHFFFAOYSA-L 0.000 description 2
- 239000002609 medium Substances 0.000 description 2
- 244000005700 microbiome Species 0.000 description 2
- 210000004877 mucosa Anatomy 0.000 description 2
- 125000001446 muramyl group Chemical group N[C@@H](C=O)[C@@H](O[C@@H](C(=O)*)C)[C@H](O)[C@H](O)CO 0.000 description 2
- 238000002703 mutagenesis Methods 0.000 description 2
- 231100000350 mutagenesis Toxicity 0.000 description 2
- 229940105132 myristate Drugs 0.000 description 2
- 238000003199 nucleic acid amplification method Methods 0.000 description 2
- 239000007764 o/w emulsion Substances 0.000 description 2
- 229920002113 octoxynol Polymers 0.000 description 2
- 229940066429 octoxynol Drugs 0.000 description 2
- 230000037361 pathway Effects 0.000 description 2
- 239000000256 polyoxyethylene sorbitan monolaurate Substances 0.000 description 2
- 235000010486 polyoxyethylene sorbitan monolaurate Nutrition 0.000 description 2
- 229920000136 polysorbate Polymers 0.000 description 2
- 229920002981 polyvinylidene fluoride Polymers 0.000 description 2
- 239000013641 positive control Substances 0.000 description 2
- 239000000843 powder Substances 0.000 description 2
- 238000001556 precipitation Methods 0.000 description 2
- 125000002924 primary amino group Chemical group [H]N([H])* 0.000 description 2
- 210000002345 respiratory system Anatomy 0.000 description 2
- 108091008146 restriction endonucleases Proteins 0.000 description 2
- 238000000926 separation method Methods 0.000 description 2
- 208000013223 septicemia Diseases 0.000 description 2
- 239000001509 sodium citrate Substances 0.000 description 2
- 239000007787 solid Substances 0.000 description 2
- 239000000758 substrate Substances 0.000 description 2
- 239000004094 surface-active agent Substances 0.000 description 2
- TUNFSRHWOTWDNC-UHFFFAOYSA-N tetradecanoic acid Chemical compound CCCCCCCCCCCCCC(O)=O TUNFSRHWOTWDNC-UHFFFAOYSA-N 0.000 description 2
- 241001515965 unidentified phage Species 0.000 description 2
- 101150084750 1 gene Proteins 0.000 description 1
- JYZJYKOZGGEXSX-UHFFFAOYSA-N 2-hydroxymyristic acid Chemical compound CCCCCCCCCCCCC(O)C(O)=O JYZJYKOZGGEXSX-UHFFFAOYSA-N 0.000 description 1
- CYDQOEWLBCCFJZ-UHFFFAOYSA-N 4-(4-fluorophenyl)oxane-4-carboxylic acid Chemical compound C=1C=C(F)C=CC=1C1(C(=O)O)CCOCC1 CYDQOEWLBCCFJZ-UHFFFAOYSA-N 0.000 description 1
- ODHCTXKNWHHXJC-VKHMYHEASA-N 5-oxo-L-proline Chemical compound OC(=O)[C@@H]1CCC(=O)N1 ODHCTXKNWHHXJC-VKHMYHEASA-N 0.000 description 1
- XZIIFPSPUDAGJM-UHFFFAOYSA-N 6-chloro-2-n,2-n-diethylpyrimidine-2,4-diamine Chemical compound CCN(CC)C1=NC(N)=CC(Cl)=N1 XZIIFPSPUDAGJM-UHFFFAOYSA-N 0.000 description 1
- 206010001052 Acute respiratory distress syndrome Diseases 0.000 description 1
- 229920000936 Agarose Polymers 0.000 description 1
- GUBGYTABKSRVRQ-XLOQQCSPSA-N Alpha-Lactose Chemical compound O[C@@H]1[C@@H](O)[C@@H](O)[C@@H](CO)O[C@H]1O[C@@H]1[C@@H](CO)O[C@H](O)[C@H](O)[C@H]1O GUBGYTABKSRVRQ-XLOQQCSPSA-N 0.000 description 1
- 101100509461 Arabidopsis thaliana JAR1 gene Proteins 0.000 description 1
- DCXYFEDJOCDNAF-UHFFFAOYSA-N Asparagine Natural products OC(=O)C(N)CC(N)=O DCXYFEDJOCDNAF-UHFFFAOYSA-N 0.000 description 1
- 241000972773 Aulopiformes Species 0.000 description 1
- QYOVMAREBTZLBT-KTKRTIGZSA-N CCCCCCCC\C=C/CCCCCCCCOCCOCCOCCOCCOCCOCCOCCOCCOCCOCCO Chemical compound CCCCCCCC\C=C/CCCCCCCCOCCOCCOCCOCCOCCOCCOCCOCCOCCOCCO QYOVMAREBTZLBT-KTKRTIGZSA-N 0.000 description 1
- TXCIAUNLDRJGJZ-BILDWYJOSA-N CMP-N-acetyl-beta-neuraminic acid Chemical compound O1[C@@H]([C@H](O)[C@H](O)CO)[C@H](NC(=O)C)[C@@H](O)C[C@]1(C(O)=O)OP(O)(=O)OC[C@@H]1[C@@H](O)[C@@H](O)[C@H](N2C(N=C(N)C=C2)=O)O1 TXCIAUNLDRJGJZ-BILDWYJOSA-N 0.000 description 1
- 101100508408 Caenorhabditis elegans ifa-3 gene Proteins 0.000 description 1
- 101100508409 Caenorhabditis elegans ifa-4 gene Proteins 0.000 description 1
- 101100508407 Caenorhabditis elegans mua-6 gene Proteins 0.000 description 1
- 241000283707 Capra Species 0.000 description 1
- BVKZGUZCCUSVTD-UHFFFAOYSA-L Carbonate Chemical compound [O-]C([O-])=O BVKZGUZCCUSVTD-UHFFFAOYSA-L 0.000 description 1
- 102000014914 Carrier Proteins Human genes 0.000 description 1
- 108700010070 Codon Usage Proteins 0.000 description 1
- 102000004127 Cytokines Human genes 0.000 description 1
- 108090000695 Cytokines Proteins 0.000 description 1
- FBPFZTCFMRRESA-KVTDHHQDSA-N D-Mannitol Chemical compound OC[C@@H](O)[C@@H](O)[C@H](O)[C@H](O)CO FBPFZTCFMRRESA-KVTDHHQDSA-N 0.000 description 1
- YVGGHNCTFXOJCH-UHFFFAOYSA-N DDT Chemical compound C1=CC(Cl)=CC=C1C(C(Cl)(Cl)Cl)C1=CC=C(Cl)C=C1 YVGGHNCTFXOJCH-UHFFFAOYSA-N 0.000 description 1
- 102000012410 DNA Ligases Human genes 0.000 description 1
- 108010061982 DNA Ligases Proteins 0.000 description 1
- 229940021995 DNA vaccine Drugs 0.000 description 1
- 102000016911 Deoxyribonucleases Human genes 0.000 description 1
- 108010053770 Deoxyribonucleases Proteins 0.000 description 1
- 240000006497 Dianthus caryophyllus Species 0.000 description 1
- 235000009355 Dianthus caryophyllus Nutrition 0.000 description 1
- 101100245206 Dictyostelium discoideum psmC4 gene Proteins 0.000 description 1
- 206010059866 Drug resistance Diseases 0.000 description 1
- 239000012591 Dulbecco’s Phosphate Buffered Saline Substances 0.000 description 1
- 102000015689 E-Selectin Human genes 0.000 description 1
- 108010024212 E-Selectin Proteins 0.000 description 1
- 101100483656 Escherichia coli (strain K12) ugd gene Proteins 0.000 description 1
- 108700039887 Essential Genes Proteins 0.000 description 1
- 241000206602 Eukaryota Species 0.000 description 1
- 230000010558 Gene Alterations Effects 0.000 description 1
- 108700039691 Genetic Promoter Regions Proteins 0.000 description 1
- 108700007698 Genetic Terminator Regions Proteins 0.000 description 1
- CEAZRRDELHUEMR-URQXQFDESA-N Gentamicin Chemical compound O1[C@H](C(C)NC)CC[C@@H](N)[C@H]1O[C@H]1[C@H](O)[C@@H](O[C@@H]2[C@@H]([C@@H](NC)[C@@](C)(O)CO2)O)[C@H](N)C[C@@H]1N CEAZRRDELHUEMR-URQXQFDESA-N 0.000 description 1
- 229930182566 Gentamicin Natural products 0.000 description 1
- HVLSXIKZNLPZJJ-TXZCQADKSA-N HA peptide Chemical compound C([C@@H](C(=O)N[C@@H](CC(O)=O)C(=O)N[C@@H](C(C)C)C(=O)N1[C@@H](CCC1)C(=O)N[C@@H](CC(O)=O)C(=O)N[C@@H](CC=1C=CC(O)=CC=1)C(=O)N[C@@H](C)C(O)=O)NC(=O)[C@H]1N(CCC1)C(=O)[C@@H](N)CC=1C=CC(O)=CC=1)C1=CC=C(O)C=C1 HVLSXIKZNLPZJJ-TXZCQADKSA-N 0.000 description 1
- 206010019280 Heart failures Diseases 0.000 description 1
- 206010061216 Infarction Diseases 0.000 description 1
- 206010061218 Inflammation Diseases 0.000 description 1
- 102000008070 Interferon-gamma Human genes 0.000 description 1
- 108010074328 Interferon-gamma Proteins 0.000 description 1
- 102000014150 Interferons Human genes 0.000 description 1
- 108010050904 Interferons Proteins 0.000 description 1
- 108010002352 Interleukin-1 Proteins 0.000 description 1
- 108010065805 Interleukin-12 Proteins 0.000 description 1
- 108010002350 Interleukin-2 Proteins 0.000 description 1
- 108090000978 Interleukin-4 Proteins 0.000 description 1
- 108010002616 Interleukin-5 Proteins 0.000 description 1
- 108090001005 Interleukin-6 Proteins 0.000 description 1
- 108010002586 Interleukin-7 Proteins 0.000 description 1
- FFEARJCKVFRZRR-BYPYZUCNSA-N L-methionine Chemical compound CSCC[C@H](N)C(O)=O FFEARJCKVFRZRR-BYPYZUCNSA-N 0.000 description 1
- QIVBCDIJIAJPQS-VIFPVBQESA-N L-tryptophane Chemical compound C1=CC=C2C(C[C@H](N)C(O)=O)=CNC2=C1 QIVBCDIJIAJPQS-VIFPVBQESA-N 0.000 description 1
- GUBGYTABKSRVRQ-QKKXKWKRSA-N Lactose Natural products OC[C@H]1O[C@@H](O[C@H]2[C@H](O)[C@@H](O)C(O)O[C@@H]2CO)[C@H](O)[C@@H](O)[C@H]1O GUBGYTABKSRVRQ-QKKXKWKRSA-N 0.000 description 1
- FYYHWMGAXLPEAU-UHFFFAOYSA-N Magnesium Chemical compound [Mg] FYYHWMGAXLPEAU-UHFFFAOYSA-N 0.000 description 1
- 229930195725 Mannitol Natural products 0.000 description 1
- 206010027202 Meningitis bacterial Diseases 0.000 description 1
- 208000034762 Meningococcal Infections Diseases 0.000 description 1
- MSFSPUZXLOGKHJ-UHFFFAOYSA-N Muraminsaeure Natural products OC(=O)C(C)OC1C(N)C(O)OC(CO)C1O MSFSPUZXLOGKHJ-UHFFFAOYSA-N 0.000 description 1
- 241001529936 Murinae Species 0.000 description 1
- BRGMHAYQAZFZDJ-PVFLNQBWSA-N N-Acetylglucosamine 6-phosphate Chemical compound CC(=O)N[C@H]1[C@@H](O)O[C@H](COP(O)(O)=O)[C@@H](O)[C@@H]1O BRGMHAYQAZFZDJ-PVFLNQBWSA-N 0.000 description 1
- 125000000729 N-terminal amino-acid group Chemical group 0.000 description 1
- 241000588654 Neisseria cinerea Species 0.000 description 1
- 241000588673 Neisseria elongata Species 0.000 description 1
- 241000588651 Neisseria flavescens Species 0.000 description 1
- 241000588652 Neisseria gonorrhoeae Species 0.000 description 1
- 241000588649 Neisseria lactamica Species 0.000 description 1
- 241000287798 Neisseria meningitidis CU385 Species 0.000 description 1
- 241000897304 Neisseria meningitidis H44/76 Species 0.000 description 1
- 241000287773 Neisseria meningitidis M6190 Species 0.000 description 1
- 241000588659 Neisseria mucosa Species 0.000 description 1
- 241000588660 Neisseria polysaccharea Species 0.000 description 1
- 241000588645 Neisseria sicca Species 0.000 description 1
- 241001136170 Neisseria subflava Species 0.000 description 1
- 206010028980 Neoplasm Diseases 0.000 description 1
- 206010030113 Oedema Diseases 0.000 description 1
- 101100504410 Oryza sativa subsp. japonica GH3.5 gene Proteins 0.000 description 1
- 101150093941 PORA gene Proteins 0.000 description 1
- 108010013639 Peptidoglycan Proteins 0.000 description 1
- 102000003992 Peroxidases Human genes 0.000 description 1
- 201000005702 Pertussis Diseases 0.000 description 1
- 241000235648 Pichia Species 0.000 description 1
- 101710094909 Porin PorA Proteins 0.000 description 1
- 101710194807 Protective antigen Proteins 0.000 description 1
- 208000013616 Respiratory Distress Syndrome Diseases 0.000 description 1
- 102000006382 Ribonucleases Human genes 0.000 description 1
- 108010083644 Ribonucleases Proteins 0.000 description 1
- 101001120437 Salmonella typhimurium (strain LT2 / SGSC1412 / ATCC 700720) Lipid A palmitoyltransferase PagP Proteins 0.000 description 1
- 101100155269 Salmonella typhimurium (strain LT2 / SGSC1412 / ATCC 700720) udg gene Proteins 0.000 description 1
- 206010040070 Septic Shock Diseases 0.000 description 1
- 238000012300 Sequence Analysis Methods 0.000 description 1
- VMHLLURERBWHNL-UHFFFAOYSA-M Sodium acetate Chemical compound [Na+].CC([O-])=O VMHLLURERBWHNL-UHFFFAOYSA-M 0.000 description 1
- 241000589970 Spirochaetales Species 0.000 description 1
- 229920002472 Starch Polymers 0.000 description 1
- 229930182558 Sterol Natural products 0.000 description 1
- NINIDFKCEFEMDL-UHFFFAOYSA-N Sulfur Chemical compound [S] NINIDFKCEFEMDL-UHFFFAOYSA-N 0.000 description 1
- 206010043376 Tetanus Diseases 0.000 description 1
- 108010092220 Tetraacyldisaccharide 4'-kinase Proteins 0.000 description 1
- AYFVYJQAPQTCCC-UHFFFAOYSA-N Threonine Natural products CC(O)C(N)C(O)=O AYFVYJQAPQTCCC-UHFFFAOYSA-N 0.000 description 1
- 239000004473 Threonine Substances 0.000 description 1
- 102000004357 Transferases Human genes 0.000 description 1
- 108090000992 Transferases Proteins 0.000 description 1
- 239000013504 Triton X-100 Substances 0.000 description 1
- 229920004890 Triton X-100 Polymers 0.000 description 1
- QIVBCDIJIAJPQS-UHFFFAOYSA-N Tryptophan Natural products C1=CC=C2C(CC(N)C(O)=O)=CNC2=C1 QIVBCDIJIAJPQS-UHFFFAOYSA-N 0.000 description 1
- 102000057144 Uridine Diphosphate Glucose Dehydrogenase Human genes 0.000 description 1
- 108010054269 Uridine Diphosphate Glucose Dehydrogenase Proteins 0.000 description 1
- 241000251539 Vertebrata <Metazoa> Species 0.000 description 1
- UZQJVUCHXGYFLQ-AYDHOLPZSA-N [(2s,3r,4s,5r,6r)-4-[(2s,3r,4s,5r,6r)-4-[(2r,3r,4s,5r,6r)-4-[(2s,3r,4s,5r,6r)-3,5-dihydroxy-6-(hydroxymethyl)-4-[(2s,3r,4s,5s,6r)-3,4,5-trihydroxy-6-(hydroxymethyl)oxan-2-yl]oxyoxan-2-yl]oxy-3,5-dihydroxy-6-(hydroxymethyl)oxan-2-yl]oxy-3,5-dihydroxy-6-(hy Chemical compound O([C@H]1[C@H](O)[C@@H](CO)O[C@H]([C@@H]1O)O[C@H]1[C@H](O)[C@@H](CO)O[C@H]([C@@H]1O)O[C@H]1CC[C@]2(C)[C@H]3CC=C4[C@@]([C@@]3(CC[C@H]2[C@@]1(C=O)C)C)(C)CC(O)[C@]1(CCC(CC14)(C)C)C(=O)O[C@H]1[C@@H]([C@@H](O[C@H]2[C@@H]([C@@H](O[C@H]3[C@@H]([C@@H](O[C@H]4[C@@H]([C@@H](O[C@H]5[C@@H]([C@@H](O)[C@H](O)[C@@H](CO)O5)O)[C@H](O)[C@@H](CO)O4)O)[C@H](O)[C@@H](CO)O3)O)[C@H](O)[C@@H](CO)O2)O)[C@H](O)[C@@H](CO)O1)O)[C@@H]1O[C@H](CO)[C@@H](O)[C@H](O)[C@H]1O UZQJVUCHXGYFLQ-AYDHOLPZSA-N 0.000 description 1
- 238000002835 absorbance Methods 0.000 description 1
- 238000005903 acid hydrolysis reaction Methods 0.000 description 1
- 230000002378 acidificating effect Effects 0.000 description 1
- 239000012190 activator Substances 0.000 description 1
- 230000001919 adrenal effect Effects 0.000 description 1
- 125000001931 aliphatic group Chemical group 0.000 description 1
- 150000005215 alkyl ethers Chemical class 0.000 description 1
- ILRRQNADMUWWFW-UHFFFAOYSA-K aluminium phosphate Chemical compound O1[Al]2OP1(=O)O2 ILRRQNADMUWWFW-UHFFFAOYSA-K 0.000 description 1
- 150000001408 amides Chemical class 0.000 description 1
- BFNBIHQBYMNNAN-UHFFFAOYSA-N ammonium sulfate Chemical class N.N.OS(O)(=O)=O BFNBIHQBYMNNAN-UHFFFAOYSA-N 0.000 description 1
- 238000010171 animal model Methods 0.000 description 1
- 239000003242 anti bacterial agent Substances 0.000 description 1
- 229940088710 antibiotic agent Drugs 0.000 description 1
- 230000027645 antigenic variation Effects 0.000 description 1
- 239000007864 aqueous solution Substances 0.000 description 1
- 125000000637 arginyl group Chemical group N[C@@H](CCCNC(N)=N)C(=O)* 0.000 description 1
- 101150008162 arnC gene Proteins 0.000 description 1
- 238000003491 array Methods 0.000 description 1
- 125000003118 aryl group Chemical group 0.000 description 1
- 235000009582 asparagine Nutrition 0.000 description 1
- 229960001230 asparagine Drugs 0.000 description 1
- 201000009904 bacterial meningitis Diseases 0.000 description 1
- 230000008901 benefit Effects 0.000 description 1
- WQZGKKKJIJFFOK-VFUOTHLCSA-N beta-D-glucose Chemical compound OC[C@H]1O[C@@H](O)[C@H](O)[C@@H](O)[C@@H]1O WQZGKKKJIJFFOK-VFUOTHLCSA-N 0.000 description 1
- 108091008324 binding proteins Proteins 0.000 description 1
- 230000004071 biological effect Effects 0.000 description 1
- 230000033228 biological regulation Effects 0.000 description 1
- 239000012472 biological sample Substances 0.000 description 1
- 230000006696 biosynthetic metabolic pathway Effects 0.000 description 1
- 230000000903 blocking effect Effects 0.000 description 1
- 239000006172 buffering agent Substances 0.000 description 1
- 235000011148 calcium chloride Nutrition 0.000 description 1
- 239000001506 calcium phosphate Substances 0.000 description 1
- 229910000389 calcium phosphate Inorganic materials 0.000 description 1
- 235000011010 calcium phosphates Nutrition 0.000 description 1
- 201000011510 cancer Diseases 0.000 description 1
- 150000001720 carbohydrates Chemical class 0.000 description 1
- 230000015556 catabolic process Effects 0.000 description 1
- 210000000170 cell membrane Anatomy 0.000 description 1
- 210000003850 cellular structure Anatomy 0.000 description 1
- 239000001913 cellulose Substances 0.000 description 1
- 229920002678 cellulose Polymers 0.000 description 1
- 235000010980 cellulose Nutrition 0.000 description 1
- 238000012512 characterization method Methods 0.000 description 1
- 229940096384 chicken egg white lysozyme Drugs 0.000 description 1
- 229960005091 chloramphenicol Drugs 0.000 description 1
- WIIZWVCIJKGZOK-RKDXNWHRSA-N chloramphenicol Chemical compound ClC(Cl)C(=O)N[C@H](CO)[C@H](O)C1=CC=C([N+]([O-])=O)C=C1 WIIZWVCIJKGZOK-RKDXNWHRSA-N 0.000 description 1
- 238000010367 cloning Methods 0.000 description 1
- 239000000084 colloidal system Substances 0.000 description 1
- 230000002860 competitive effect Effects 0.000 description 1
- 238000004590 computer program Methods 0.000 description 1
- 230000021615 conjugation Effects 0.000 description 1
- 238000013270 controlled release Methods 0.000 description 1
- 230000002596 correlated effect Effects 0.000 description 1
- 239000006071 cream Substances 0.000 description 1
- 239000012228 culture supernatant Substances 0.000 description 1
- 238000007822 cytometric assay Methods 0.000 description 1
- 230000001086 cytosolic effect Effects 0.000 description 1
- 238000002784 cytotoxicity assay Methods 0.000 description 1
- 231100000263 cytotoxicity test Toxicity 0.000 description 1
- 230000007547 defect Effects 0.000 description 1
- 238000006731 degradation reaction Methods 0.000 description 1
- 238000012217 deletion Methods 0.000 description 1
- 230000037430 deletion Effects 0.000 description 1
- 229960003964 deoxycholic acid Drugs 0.000 description 1
- 238000001514 detection method Methods 0.000 description 1
- 229960000633 dextran sulfate Drugs 0.000 description 1
- 238000000502 dialysis Methods 0.000 description 1
- 239000003085 diluting agent Substances 0.000 description 1
- 206010013023 diphtheria Diseases 0.000 description 1
- LOKCTEFSRHRXRJ-UHFFFAOYSA-I dipotassium trisodium dihydrogen phosphate hydrogen phosphate dichloride Chemical compound P(=O)(O)(O)[O-].[K+].P(=O)(O)([O-])[O-].[Na+].[Na+].[Cl-].[K+].[Cl-].[Na+] LOKCTEFSRHRXRJ-UHFFFAOYSA-I 0.000 description 1
- 229940042399 direct acting antivirals protease inhibitors Drugs 0.000 description 1
- KAKKHKRHCKCAGH-UHFFFAOYSA-L disodium;(4-nitrophenyl) phosphate;hexahydrate Chemical compound O.O.O.O.O.O.[Na+].[Na+].[O-][N+](=O)C1=CC=C(OP([O-])([O-])=O)C=C1 KAKKHKRHCKCAGH-UHFFFAOYSA-L 0.000 description 1
- 230000003828 downregulation Effects 0.000 description 1
- 238000009510 drug design Methods 0.000 description 1
- 238000001962 electrophoresis Methods 0.000 description 1
- 238000004520 electroporation Methods 0.000 description 1
- 210000002889 endothelial cell Anatomy 0.000 description 1
- 239000003623 enhancer Substances 0.000 description 1
- 230000007613 environmental effect Effects 0.000 description 1
- 230000002255 enzymatic effect Effects 0.000 description 1
- 230000007071 enzymatic hydrolysis Effects 0.000 description 1
- 238000006047 enzymatic hydrolysis reaction Methods 0.000 description 1
- 229960003276 erythromycin Drugs 0.000 description 1
- 210000003527 eukaryotic cell Anatomy 0.000 description 1
- 238000002474 experimental method Methods 0.000 description 1
- 239000000284 extract Substances 0.000 description 1
- 235000013861 fat-free Nutrition 0.000 description 1
- 238000000684 flow cytometry Methods 0.000 description 1
- 239000012530 fluid Substances 0.000 description 1
- 239000007850 fluorescent dye Substances 0.000 description 1
- 229940044627 gamma-interferon Drugs 0.000 description 1
- 238000012215 gene cloning Methods 0.000 description 1
- 230000004077 genetic alteration Effects 0.000 description 1
- 231100000118 genetic alteration Toxicity 0.000 description 1
- 238000010353 genetic engineering Methods 0.000 description 1
- 235000001727 glucose Nutrition 0.000 description 1
- 229930195712 glutamate Natural products 0.000 description 1
- WHUUTDBJXJRKMK-VKHMYHEASA-L glutamate group Chemical group N[C@@H](CCC(=O)[O-])C(=O)[O-] WHUUTDBJXJRKMK-VKHMYHEASA-L 0.000 description 1
- 150000002332 glycine derivatives Chemical class 0.000 description 1
- 238000000265 homogenisation Methods 0.000 description 1
- 230000028996 humoral immune response Effects 0.000 description 1
- 230000033444 hydroxylation Effects 0.000 description 1
- 238000005805 hydroxylation reaction Methods 0.000 description 1
- 210000000987 immune system Anatomy 0.000 description 1
- 238000003018 immunoassay Methods 0.000 description 1
- 230000000951 immunodiffusion Effects 0.000 description 1
- 230000016784 immunoglobulin production Effects 0.000 description 1
- 230000004957 immunoregulator effect Effects 0.000 description 1
- 229960001438 immunostimulant agent Drugs 0.000 description 1
- 230000002779 inactivation Effects 0.000 description 1
- 230000007574 infarction Effects 0.000 description 1
- 230000004054 inflammatory process Effects 0.000 description 1
- 230000000977 initiatory effect Effects 0.000 description 1
- 230000010354 integration Effects 0.000 description 1
- 229940047124 interferons Drugs 0.000 description 1
- 208000028867 ischemia Diseases 0.000 description 1
- BPHPUYQFMNQIOC-NXRLNHOXSA-N isopropyl beta-D-thiogalactopyranoside Chemical compound CC(C)S[C@@H]1O[C@H](CO)[C@H](O)[C@H](O)[C@H]1O BPHPUYQFMNQIOC-NXRLNHOXSA-N 0.000 description 1
- 229960000318 kanamycin Drugs 0.000 description 1
- 229930027917 kanamycin Natural products 0.000 description 1
- SBUJHOSQTJFQJX-NOAMYHISSA-N kanamycin Chemical compound O[C@@H]1[C@@H](O)[C@H](O)[C@@H](CN)O[C@@H]1O[C@H]1[C@H](O)[C@@H](O[C@@H]2[C@@H]([C@@H](N)[C@H](O)[C@@H](CO)O2)O)[C@H](N)C[C@@H]1N SBUJHOSQTJFQJX-NOAMYHISSA-N 0.000 description 1
- 229930182823 kanamycin A Natural products 0.000 description 1
- 210000003734 kidney Anatomy 0.000 description 1
- 239000008101 lactose Substances 0.000 description 1
- 238000011031 large-scale manufacturing process Methods 0.000 description 1
- 231100001231 less toxic Toxicity 0.000 description 1
- 239000003446 ligand Substances 0.000 description 1
- 239000007788 liquid Substances 0.000 description 1
- 239000006210 lotion Substances 0.000 description 1
- 101150070011 lpxK gene Proteins 0.000 description 1
- 210000004072 lung Anatomy 0.000 description 1
- 229940042470 lyme disease vaccine Drugs 0.000 description 1
- 230000002934 lysing effect Effects 0.000 description 1
- 239000011777 magnesium Substances 0.000 description 1
- 229910052749 magnesium Inorganic materials 0.000 description 1
- 229910001629 magnesium chloride Inorganic materials 0.000 description 1
- 235000019359 magnesium stearate Nutrition 0.000 description 1
- 239000000594 mannitol Substances 0.000 description 1
- 235000010355 mannitol Nutrition 0.000 description 1
- 230000007246 mechanism Effects 0.000 description 1
- 208000037941 meningococcal disease Diseases 0.000 description 1
- 239000011859 microparticle Substances 0.000 description 1
- 108700007621 mifamurtide Proteins 0.000 description 1
- 235000013336 milk Nutrition 0.000 description 1
- 239000008267 milk Substances 0.000 description 1
- 210000004080 milk Anatomy 0.000 description 1
- 230000003278 mimic effect Effects 0.000 description 1
- 238000010369 molecular cloning Methods 0.000 description 1
- 238000000329 molecular dynamics simulation Methods 0.000 description 1
- 210000001616 monocyte Anatomy 0.000 description 1
- 230000003387 muscular Effects 0.000 description 1
- JXTPJDDICSTXJX-UHFFFAOYSA-N n-Triacontane Natural products CCCCCCCCCCCCCCCCCCCCCCCCCCCCCC JXTPJDDICSTXJX-UHFFFAOYSA-N 0.000 description 1
- DVEKCXOJTLDBFE-UHFFFAOYSA-N n-dodecyl-n,n-dimethylglycinate Chemical compound CCCCCCCCCCCC[N+](C)(C)CC([O-])=O DVEKCXOJTLDBFE-UHFFFAOYSA-N 0.000 description 1
- 210000004897 n-terminal region Anatomy 0.000 description 1
- 210000001989 nasopharynx Anatomy 0.000 description 1
- 229910052759 nickel Inorganic materials 0.000 description 1
- 239000002736 nonionic surfactant Substances 0.000 description 1
- 239000002674 ointment Substances 0.000 description 1
- 101150047779 ompB gene Proteins 0.000 description 1
- 230000003287 optical effect Effects 0.000 description 1
- 230000004768 organ dysfunction Effects 0.000 description 1
- 230000003204 osmotic effect Effects 0.000 description 1
- 239000003002 pH adjusting agent Substances 0.000 description 1
- 238000004806 packaging method and process Methods 0.000 description 1
- 210000002741 palatine tonsil Anatomy 0.000 description 1
- 230000035515 penetration Effects 0.000 description 1
- 239000000137 peptide hydrolase inhibitor Substances 0.000 description 1
- 208000008494 pericarditis Diseases 0.000 description 1
- 230000002093 peripheral effect Effects 0.000 description 1
- 210000001322 periplasm Anatomy 0.000 description 1
- 108040007629 peroxidase activity proteins Proteins 0.000 description 1
- NBIIXXVUZAFLBC-UHFFFAOYSA-K phosphate Chemical compound [O-]P([O-])([O-])=O NBIIXXVUZAFLBC-UHFFFAOYSA-K 0.000 description 1
- 230000000704 physical effect Effects 0.000 description 1
- 230000004962 physiological condition Effects 0.000 description 1
- 239000006187 pill Substances 0.000 description 1
- 239000013600 plasmid vector Substances 0.000 description 1
- 229920000642 polymer Polymers 0.000 description 1
- 238000003752 polymerase chain reaction Methods 0.000 description 1
- 229940051841 polyoxyethylene ether Drugs 0.000 description 1
- 229920000056 polyoxyethylene ether Polymers 0.000 description 1
- 101150031507 porB gene Proteins 0.000 description 1
- 230000020971 positive regulation of blood coagulation Effects 0.000 description 1
- 230000018338 positive regulation of fibrinolysis Effects 0.000 description 1
- 230000004481 post-translational protein modification Effects 0.000 description 1
- 239000001103 potassium chloride Substances 0.000 description 1
- 235000011164 potassium chloride Nutrition 0.000 description 1
- 238000004321 preservation Methods 0.000 description 1
- 230000002265 prevention Effects 0.000 description 1
- 210000001236 prokaryotic cell Anatomy 0.000 description 1
- 230000001902 propagating effect Effects 0.000 description 1
- 238000001742 protein purification Methods 0.000 description 1
- 230000005180 public health Effects 0.000 description 1
- 229940043131 pyroglutamate Drugs 0.000 description 1
- 238000003908 quality control method Methods 0.000 description 1
- 230000002285 radioactive effect Effects 0.000 description 1
- 239000011541 reaction mixture Substances 0.000 description 1
- 238000003259 recombinant expression Methods 0.000 description 1
- 229940126583 recombinant protein vaccine Drugs 0.000 description 1
- 230000009467 reduction Effects 0.000 description 1
- 230000022532 regulation of transcription, DNA-dependent Effects 0.000 description 1
- 238000009877 rendering Methods 0.000 description 1
- 230000003362 replicative effect Effects 0.000 description 1
- 238000011160 research Methods 0.000 description 1
- 210000003705 ribosome Anatomy 0.000 description 1
- CVHZOJJKTDOEJC-UHFFFAOYSA-N saccharin Chemical compound C1=CC=C2C(=O)NS(=O)(=O)C2=C1 CVHZOJJKTDOEJC-UHFFFAOYSA-N 0.000 description 1
- 235000019515 salmon Nutrition 0.000 description 1
- 150000003839 salts Chemical class 0.000 description 1
- 239000012723 sample buffer Substances 0.000 description 1
- 108700004121 sarkosyl Proteins 0.000 description 1
- 230000003248 secreting effect Effects 0.000 description 1
- 230000028327 secretion Effects 0.000 description 1
- 230000036303 septic shock Effects 0.000 description 1
- 238000002864 sequence alignment Methods 0.000 description 1
- 230000035939 shock Effects 0.000 description 1
- 239000013605 shuttle vector Substances 0.000 description 1
- 206010040882 skin lesion Diseases 0.000 description 1
- 231100000444 skin lesion Toxicity 0.000 description 1
- 239000001632 sodium acetate Substances 0.000 description 1
- 235000017281 sodium acetate Nutrition 0.000 description 1
- NLJMYIDDQXHKNR-UHFFFAOYSA-K sodium citrate Chemical compound O.O.[Na+].[Na+].[Na+].[O-]C(=O)CC(O)(CC([O-])=O)C([O-])=O NLJMYIDDQXHKNR-UHFFFAOYSA-K 0.000 description 1
- 239000001540 sodium lactate Substances 0.000 description 1
- 229940005581 sodium lactate Drugs 0.000 description 1
- 235000011088 sodium lactate Nutrition 0.000 description 1
- KSAVQLQVUXSOCR-UHFFFAOYSA-M sodium lauroyl sarcosinate Chemical compound [Na+].CCCCCCCCCCCC(=O)N(C)CC([O-])=O KSAVQLQVUXSOCR-UHFFFAOYSA-M 0.000 description 1
- 229940045885 sodium lauroyl sarcosinate Drugs 0.000 description 1
- 239000001488 sodium phosphate Substances 0.000 description 1
- 229910000162 sodium phosphate Inorganic materials 0.000 description 1
- 238000000527 sonication Methods 0.000 description 1
- 229940035044 sorbitan monolaurate Drugs 0.000 description 1
- 241000894007 species Species 0.000 description 1
- 210000000952 spleen Anatomy 0.000 description 1
- 229940032094 squalane Drugs 0.000 description 1
- YYGNTYWPHWGJRM-AAJYLUCBSA-N squalene Chemical compound CC(C)=CCC\C(C)=C\CC\C(C)=C\CC\C=C(/C)CC\C=C(/C)CCC=C(C)C YYGNTYWPHWGJRM-AAJYLUCBSA-N 0.000 description 1
- 230000010473 stable expression Effects 0.000 description 1
- 238000010561 standard procedure Methods 0.000 description 1
- 239000008107 starch Substances 0.000 description 1
- 235000019698 starch Nutrition 0.000 description 1
- 150000003432 sterols Chemical class 0.000 description 1
- 235000003702 sterols Nutrition 0.000 description 1
- 239000011593 sulfur Substances 0.000 description 1
- 229910052717 sulfur Inorganic materials 0.000 description 1
- 230000008093 supporting effect Effects 0.000 description 1
- 239000000725 suspension Substances 0.000 description 1
- 230000002195 synergetic effect Effects 0.000 description 1
- 239000003826 tablet Substances 0.000 description 1
- 239000000454 talc Substances 0.000 description 1
- 235000012222 talc Nutrition 0.000 description 1
- 229910052623 talc Inorganic materials 0.000 description 1
- 101150095556 tbpB gene Proteins 0.000 description 1
- 230000001225 therapeutic effect Effects 0.000 description 1
- 210000001519 tissue Anatomy 0.000 description 1
- 238000011200 topical administration Methods 0.000 description 1
- 230000009466 transformation Effects 0.000 description 1
- QORWJWZARLRLPR-UHFFFAOYSA-H tricalcium bis(phosphate) Chemical compound [Ca+2].[Ca+2].[Ca+2].[O-]P([O-])([O-])=O.[O-]P([O-])([O-])=O QORWJWZARLRLPR-UHFFFAOYSA-H 0.000 description 1
- HRXKRNGNAMMEHJ-UHFFFAOYSA-K trisodium citrate Chemical compound [Na+].[Na+].[Na+].[O-]C(=O)CC(O)(CC([O-])=O)C([O-])=O HRXKRNGNAMMEHJ-UHFFFAOYSA-K 0.000 description 1
- 229940038773 trisodium citrate Drugs 0.000 description 1
- RYFMWSXOAZQYPI-UHFFFAOYSA-K trisodium phosphate Chemical compound [Na+].[Na+].[Na+].[O-]P([O-])([O-])=O RYFMWSXOAZQYPI-UHFFFAOYSA-K 0.000 description 1
- OUYCCCASQSFEME-UHFFFAOYSA-N tyrosine Natural products OC(=O)C(N)CC1=CC=C(O)C=C1 OUYCCCASQSFEME-UHFFFAOYSA-N 0.000 description 1
- 230000002792 vascular Effects 0.000 description 1
- 239000003981 vehicle Substances 0.000 description 1
- 230000001018 virulence Effects 0.000 description 1
- XLYOFNOQVPJJNP-UHFFFAOYSA-N water Substances O XLYOFNOQVPJJNP-UHFFFAOYSA-N 0.000 description 1
Images
Classifications
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K39/00—Medicinal preparations containing antigens or antibodies
- A61K39/02—Bacterial antigens
- A61K39/095—Neisseria
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61P—SPECIFIC THERAPEUTIC ACTIVITY OF CHEMICAL COMPOUNDS OR MEDICINAL PREPARATIONS
- A61P31/00—Antiinfectives, i.e. antibiotics, antiseptics, chemotherapeutics
- A61P31/04—Antibacterial agents
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61P—SPECIFIC THERAPEUTIC ACTIVITY OF CHEMICAL COMPOUNDS OR MEDICINAL PREPARATIONS
- A61P37/00—Drugs for immunological or allergic disorders
- A61P37/02—Immunomodulators
- A61P37/04—Immunostimulants
-
- C—CHEMISTRY; METALLURGY
- C07—ORGANIC CHEMISTRY
- C07K—PEPTIDES
- C07K16/00—Immunoglobulins [IGs], e.g. monoclonal or polyclonal antibodies
- C07K16/12—Immunoglobulins [IGs], e.g. monoclonal or polyclonal antibodies against material from bacteria
- C07K16/1203—Immunoglobulins [IGs], e.g. monoclonal or polyclonal antibodies against material from bacteria from Gram-negative bacteria
- C07K16/1217—Immunoglobulins [IGs], e.g. monoclonal or polyclonal antibodies against material from bacteria from Gram-negative bacteria from Neisseriaceae (F)
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K39/00—Medicinal preparations containing antigens or antibodies
- A61K2039/555—Medicinal preparations containing antigens or antibodies characterised by a specific combination antigen/adjuvant
- A61K2039/55505—Inorganic adjuvants
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61K—PREPARATIONS FOR MEDICAL, DENTAL OR TOILETRY PURPOSES
- A61K39/00—Medicinal preparations containing antigens or antibodies
- A61K2039/555—Medicinal preparations containing antigens or antibodies characterised by a specific combination antigen/adjuvant
- A61K2039/55511—Organic adjuvants
- A61K2039/55566—Emulsions, e.g. Freund's adjuvant, MF59
-
- C—CHEMISTRY; METALLURGY
- C07—ORGANIC CHEMISTRY
- C07K—PEPTIDES
- C07K14/00—Peptides having more than 20 amino acids; Gastrins; Somatostatins; Melanotropins; Derivatives thereof
- C07K14/195—Peptides having more than 20 amino acids; Gastrins; Somatostatins; Melanotropins; Derivatives thereof from bacteria
- C07K14/22—Peptides having more than 20 amino acids; Gastrins; Somatostatins; Melanotropins; Derivatives thereof from bacteria from Neisseriaceae (F)
-
- C—CHEMISTRY; METALLURGY
- C07—ORGANIC CHEMISTRY
- C07K—PEPTIDES
- C07K2317/00—Immunoglobulins specific features
- C07K2317/30—Immunoglobulins specific features characterized by aspects of specificity or valency
- C07K2317/34—Identification of a linear epitope shorter than 20 amino acid residues or of a conformational epitope defined by amino acid residues
-
- C—CHEMISTRY; METALLURGY
- C07—ORGANIC CHEMISTRY
- C07K—PEPTIDES
- C07K2319/00—Fusion polypeptide
Definitions
- This invention relates to vaccines for diseases caused by Neisseria meningitidis.
- Neisseria meningitidis is a Gram-negative bacterium which colonizes the human upper respiratory tract and is responsible for worldwide sporadic and cyclical epidemic outbreaks of, most notably, meningitis and sepsis. The attack and morbidity rates are highest in children under 2 years of age. Like other Gram-negative bacteria, Neisseria meningitidis typically possess a cytoplasmic membrane, a peptidoglycan layer, an outer membrane which together with the capsular polysaccharide constitute the bacterial wall, and pili, which project into the outside environment. Encapsulated strains of Neisseria meningitidis are a major cause of bacterial meningitis and septicemia in children and young adults. The prevalence and economic importance of invasive Neisseria meningitidis infections have driven the search for effective vaccines that can confer immunity across different strains, and particularly across genetically diverse group B strains with different serotypes or serosubtypes.
- N. meningitidis protein which is expressed in the bacterium as a surface-exposed lipoprotein. Based on sequence analysis of 71 N. meningitidis strains representative of its genetic and geographic diversity, N.
- variant 1 meningitidis strains have been sub-divided into three fHBP variant groups (referred to as variant 1 (v.1), variant 2 (v.2), and variant 3 (v.3)) based on amino acid sequence variability and immunologic cross-reactivity ( Masignani et al. J Exp Med 2003; 197:789-99 ).
- Other workers (Fletcher et al, 2004) have subdivided the protein into two sub-families designated A (which includes v.2 and v.3 of Masignani) and B (v.1).
- Variant 1 strains account for about 60% of disease-producing group B isolates (Masignani et al. 2003, supra). Within each variant group, there is on the order of about 92% or greater conservation of amino acid sequence.
- each variant group ranges between 89 and 100%, while between the variant groups (e.g., between v.1 and v.2) the conservation can be as low as 59%.
- the protein is expressed by all known strains of N. meningitidis.
- mice immunized with recombinant fHBP developed high serum bactericidal antibody responses against strains expressing fHBP proteins of the homologous variant group (Masignani et al. 2003, supra; Welsch et al. 2004, J Immunol. 172(9):5606-15 .).
- antiserum prepared against fHBP v.1 confers protection against N. meningitidis strains expressing fHBP v.1, but not against strains expressing fHBP v.2 or v.3.
- antiserum prepared against fHBP v.2 protects against strains expressing v.2 (or v.3) but not v.1 ( Masignani et al.
- Chimeric proteins have been used for vaccine development in a variety of ways.
- a first strategy employs a genetic or chemical linkage of an antigen to a known, but unrelated, immunogenic protein, such as the diphtheria, tetanus or pertussis toxoid proteins, or the cholera toxin B (CTB) domain, in order to enhance the magnitude of the antibody responses to the antigen of interest.
- CTB cholera toxin B
- a second strategy uses a genetic fusion of two antigens from the same organism, to enhance cross-protection against strains with antigenic diversity ( Giuliani et al. Infect Immun 2005 73:1151-60 ).
- An example is the multivalent group B meningococcal recombinant protein vaccine, which contains a mixture of two fusion proteins: a first fusion protein of a GNA2091 protein and a GNA1870 (or "fHBP") protein, and a second fusion protein of a GNA2132 protein and a GNA1030 protein ( Giuliani et al. Proc Natl Acad Sci U S A 2006, 103:10834-9 ).
- a third strategy has been to construct a fusion of different serologic variants ("serovars") of one antigen to induce cross-protection against a strains with antigenic diversity.
- An example is a tetravalent OspC chimeric Lyme disease vaccine, which induced bactericidal antibody responses against spirochete strains expressing each of the OspC types that were incorporated into the construct ( Earnhart et al. Vaccine 2007;25:466-80 ).
- the vaccines were composed of repeats of an individual domain with antigenic variability.
- the respective variants of the domain were expressed in tandem in one protein (i.e., the same domain from different strains, A 1 -A 2 -A 3 -A 4 , etc).
- these recombinant tandem proteins can be convenient for manufacturing and quality control. However they also can be very large and subject to improper folding or degradation.
- One approach to avoiding the problem of large tandem fusion proteins is to design a single polypeptide that is composed of different domains of two antigenic variants e.g., by "swapping" different individual domains of an antigen, or even smaller regions such as individual epitopes from two different proteins, to form a chimeric protein that expresses antigenically unrelated epitopes specific for more than one strain (i.e., different domains from two different strains, A 1 -B 2 or A 2 -B 1 , etc.).
- a chimeric protein containing the B domain from a variant 3 strain (B 3 ) fused with the C domain of a variant 1 strain (C 1 ) failed to elicit protective bactericidal responses against strains with either v.1 or v.2 fHBP.
- Vaccines that exploit the ability of fHBP to elicit bactericidal antibody responses and that can elicit such antibodies that are effective against strains expressing different fHBP variants remain of interest.
- Chimeric fHBPs that can elicit antibodies that are bactericidal for different fHBP variant strains of N. meningitidis, and methods of use, are provided.
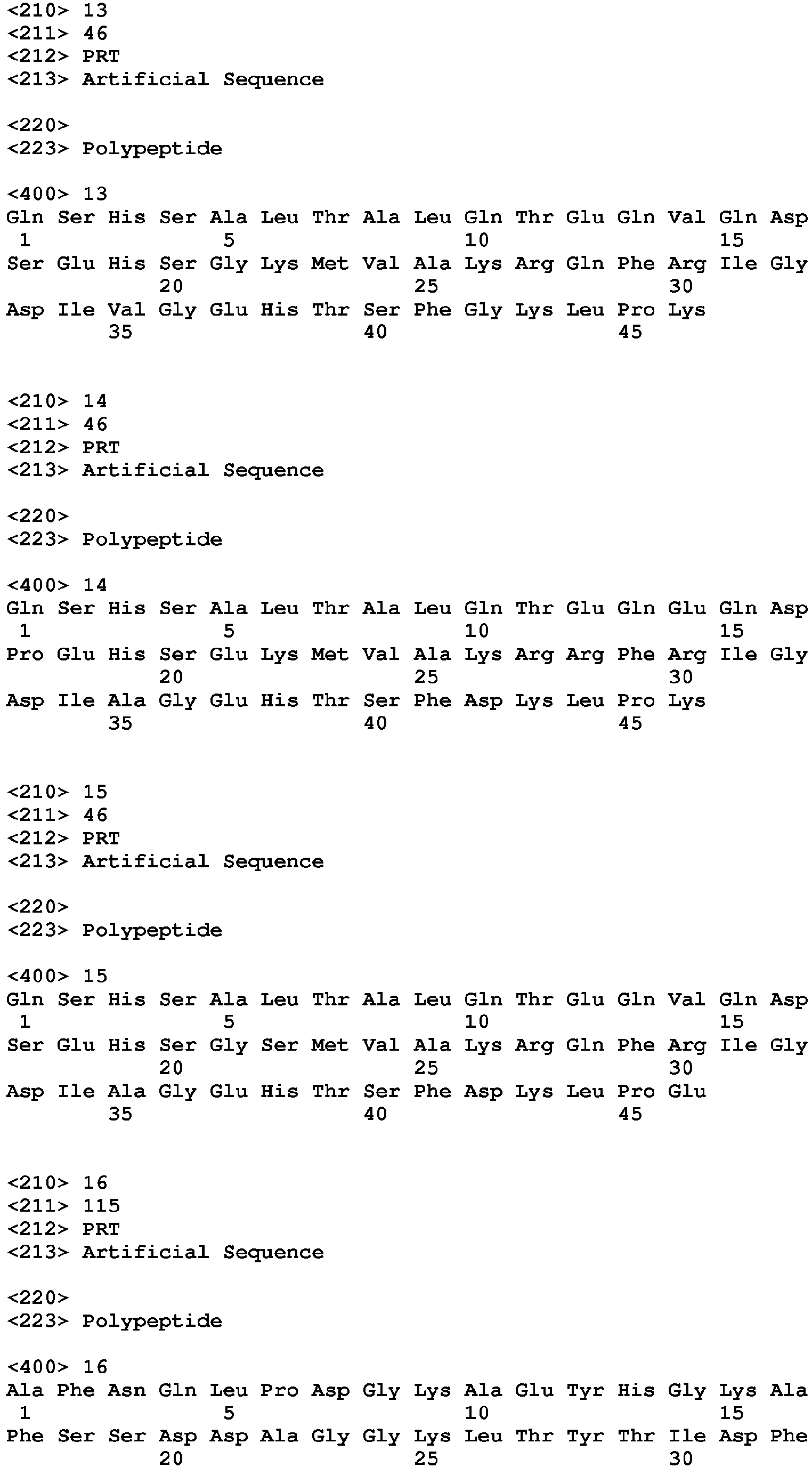
- Figure 1 is a collection of results of Western blot analysis illustrating the amino acid residues involved in binding of monoclonal antibodies (mAbs) JAR 3 and JAR 5 to factor H binding protein (fHBP).
- Panel A JAR 5; lane 1, molecular mass standard; lane 2, pET21b; lane 3, pET21-fHBP(MC58 wildtype); lane 4, pET21-fHBP(MC58)G121R; lane 5, pET21-fHBP(M6190 wildtype)R121; lane 6, pET21-fHBP(M6190)R121G.
- Panel B JAR 3.
- C Penta-His mAb. Panels B and C have the same lane assignments as panel A.
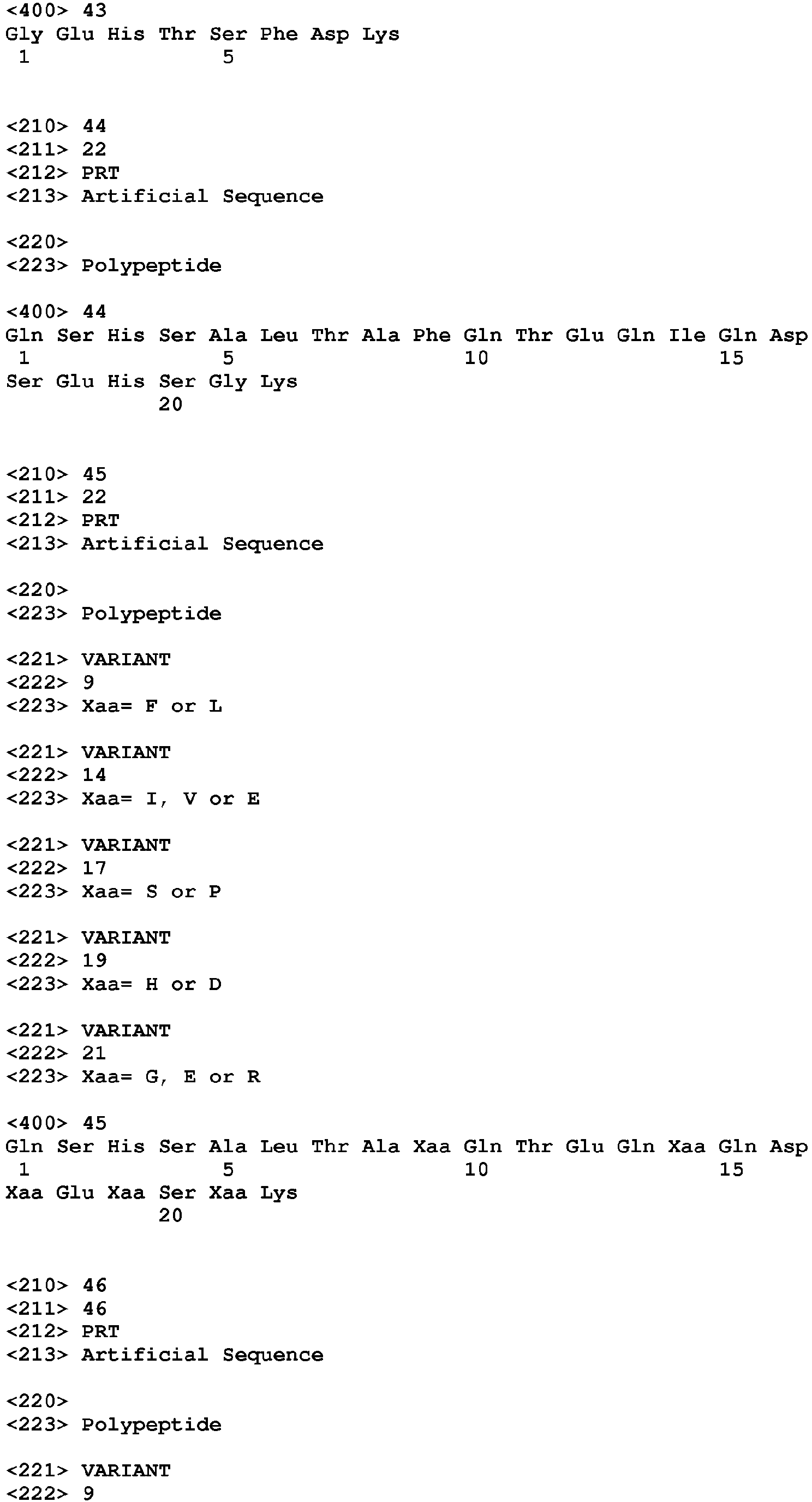
- Figure 2 is a set of graphs illustrating that binding of JAR 3 and JAR 5 mAbs to fHBP is competitive. Percent competitive inhibition of binding of anti-fHBP mAbs to fHBP by a second antibody as measured by ELISA. Each panel includes: rabbit polyclonal anti-fHBP antiserum; rabbit pre-immune serum; and a negative control mAb specific for an irrelevant capsular antigen (JW-C2, -A2 or -A1). Panel A, Inhibition of binding of JAR 3 by JAR 4 or JAR 5. Panel B, Inhibition of binding of JAR 5 by JAR 3 or JAR 4. Panel C, Inhibition of binding of JAR 4 by JAR 3 or JAR 5.
- Figure 3 is a schematic illustrating positions of residues associated with the epitopes of the nine anti-fHBP mAbs ("JAR" mAbs) in the structural model based on previously reported NMR data ( Cantini et al. "Solution structure of the immunodominant domain of protective antigen GNA1870 of Neisseria meningitidis.” J Biol Chem 2006; 281:7220-7 ). Coordinates from the solution structure of the B and C domains of fHBP v.1 from strain MC58 were used to construct the model.
- JAR anti-fHBP mAbs
- variant 2 (v.2) fHBP protein (from strain 8047) and variant 3 (v.3) fHBP (from strain M1239) differ by -1 and +7 amino acid residues, respectively, from that of MC58
- the numbering used to refer to residues for v.2 and v.3 fHBP proteins differs from numbering based on the actual amino acid sequences of these proteins.
- reference to a leucine residue (L) at position 166 of the v.2 or v.3 fHBP sequence in Figure 3 refers to the residue at position 165 of the v.2 protein and at position 173 in the v.3 protein.
- Figure 4 for alignment.
- the residue shown for mAb 502 is from a previously reported study ( Giuliani et al., 2005 Infect Immun 73:1151-60 ). The numbering is based on amino acid sequence of MC58 v.1 fHBP lacking the signal sequence ( Masignani et al., 2003 J Exp Med 197:789-99 ).
- Figure 4 is a schematic providing an alignment of wild-type and chimeric fHBP amino acid sequences (alignment performed using ClustalW).
- the deduced amino acid sequences of fHBP v.1 from strain MC58 (bottom) and v.2 strain 8047 (top) are shown, along with the two chimeric sequences (middle, Chimera I and Chimera II). Numbering for all four proteins is based on the native, mature v.1 protein from MC58 (i.e., without the signal sequence).
- the recombinant fHBP protein as expressed in E. coli lacks both the signal sequence and seven presumably flexible residues (CSSGGGG). An N-terminal methionine was added to each sequence shown to facilitate expression in E.
- Chimera I and Chimera II have identical amino acid sequences. The exception is at residue 174 where alanine in Chimera I has been replaced by lysine in Chimera II. The position of the A174K substitution in Chimera II is shown in bold. Sequence alignment was performed with ClustalW.
- Figure 5 is a schematic representation of chimeric fHBPs.
- the N-terminal portion of the B domain from the v. 1 fHBP is on the right, and the C-terminal portion of the B domain encompassing the ⁇ -helix of the v.2 protein together with the C domain of the v. 2 fHBP is on the left.
- the junction point for these chimeras, exemplified by G136 is indicated with an arrow and accompanying text.
- Both chimeric proteins express the JAR 3 and JAR 5 epitopes expressed on the B domain of fHBP v.1 and the JAR 10 epitope, which is on the C domain of subsets of strains expressing v.1, v.2 or v.3 fHBP.
- Chimera I contains the JAR 11 epitope, including residue A174 (Panel A), which is expressed on the C domains of a subset of strains expressing fHBP v.2 or v.3.
- Chimera II contains the JAR 32 /JAR 35 epitopes, including residue K174, which are expressed on the C domains of subsets of strains expressing fHBP v.2 or v.3. A domains are not shown in these representations.
- the model was constructed based on the NMR structure of Cantini et al. (2006) J Biol Chem 281:7220-7 .
- Figure 6 provides the results of SDS-PAGE analysis of purified wild-type and mutant fHBPs.
- Proteins were expressed from pET21-based plasmids in E. coli BL21(DE3) as C-terminal hexa-histidine fusions and purified by metal chelate chromatography. Proteins were dialyzed against 1x PBS, 5% sucrose, 1 mM DTT and filter sterilized. Proteins (5 ⁇ g each) were separated on a 4-12% polyacrylamide gel and stained with Coomassie blue. Lane 1, mass standard; 2, fHBP v.1 (MC58); 3, fHBP v.2 (8047); 4, fHBP Chimera I; 5, fHBP Chimera II.
- Figure 7 is a set of graphs illustrating binding of individual anti-fHBP mAbs to recombinant proteins.
- Panel A shows mAbs prepared against fHBP v.1;
- Panel B fHBP v.2;
- Panel C fHBP v.3.
- the symbols represent different antigens on the plate: open squares, fHBP v.1; open circles, fHBP v.2; open triangles, Chimera I; asterisks, Chimera II.
- Figure 8A provides a table of strains used in the Examples, including those used to measure serum bactericidal antibody responses and description of the amino acid sequence identity compared with prototype fHBP v.1, v.2 and v.3 and JAR mAb binding of the respective fHBPs.
- Figure 8B shows the amino acid identities of different domains of fHBP. Comparisons are made for the A domain (residues 1-100), the B domain (residues 101-164) and the C domain (residues 165-255). Comparisons also are made for the B domain up to the junction point (101-135) and the B domain starting at the junction point (136-164). Numbering of amino acid residues is based on the mature protein (i.e. lacking the signal sequence) from strain MC58.
- Figure 9 is a graph illustrating serum bactericidal antibody responses of mice immunized with chimeric recombinant proteins given with Freund's adjuvant as measured against N. meningitidis group B strains expressing fHBP in the antigenic v.1 group. Strain H44/76 expresses fHBP v. 1 identical to that of the fHBP v. 1 control vaccine. The remaining strains express subvariants of fHBP v.1 (See Table in Figure 8A , above). Values are presented as 1/GMT (Reciprocal (or inverse) geometric mean titer) with a 95% confidence interval.
- 1/GMT Reciprocal (or inverse) geometric mean titer
- Figure 10 is a graph illustrating serum bactericidal antibody responses of mice immunized with chimeric recombinant proteins given with Freund's adjuvant as measured against N. meningitidis group B expressing fHBP in the v.2 or v.3 antigenic groups.
- Strain 8047 expresses fHBP v.2 identical to that of control rfHBP v.2 vaccine. The remaining strains express subvariants of fHBP v.2 or v.3 (see Table in Figure 8A ). Values are presented as 1/GMT with a 95% confidence interval. The data are stratified based on strains reacting with JAR 11 (left panel) or JAR 32 (right panel).
- Chimera I and II vaccines are identical except that Chimera I has residue A174 and is JAR 11-positive and JAR 32-negative, whereas Chimera II has residue K174 and is JAR 11-negative and JAR 32-positive. See figure for bar symbols.
- Figure 11 is a graph illustrating serum bactericidal antibody responses of mice immunized with chimeric recombinant proteins adsorbed to aluminum hydroxide as measured against N. meningitidis group B strains expressing fHBP in the antigenic v.1 group. Strain H44/76 expresses fHBP v.1 identical to that of the fHBP v.1 control vaccine. The remaining strains express subvariants of fHBP v.1. Values are presented as 1/GMT (i.e., reciprocal (or inverse) geometric mean titer) with a 95% confidence interval. Bar symbols for each vaccine are as shown in Figure 10 .
- 1/GMT i.e., reciprocal (or inverse) geometric mean titer
- Figure 12 is a graph illustrating serum bactericidal antibody responses of mice immunized with chimeric recombinant proteins adsorbed to aluminum hydroxide as measured against N. meningitidis group B expressing fHBP in the v.2 or v.3 antigenic groups.
- Strain 8047 expresses fHBP v.2 identical to that of control rfHBP v.2 vaccine. The remaining strains express subvariants of fHBP v.2 or v.3 (see Table in Figure 8 ). Values are presented as 1/GMT with a 95% confidence interval. The data are stratified based on strains reacting with JAR 11 (left panel) or JAR 32 (right panel).
- the Chimera I and II vaccines are identical except that Chimera I is JAR 11-positive and JAR 32-negative, whereas Chimera II is JAR 11-negative and JAR 32-positive Bar symbols for each vaccine are as shown in Figure 10 .
- Figure 13 is a schematic showing alignment of fHBP v.1 amino acid sequences with natural polymorphisms in the N-terminal portion of the B domain.
- the sequence shown also comprises a C-terminal portion of the fHbpN domain and a small N-terminal portion of the fHbpC domain as indicated above the alignment.
- the sequence conservation is shown below the alignment (code as in Figure 4 ).
- the positions of ⁇ -helices are shown above the alignment.
- the position of the junction point in the chimeric proteins is shown in the box. Numbering is based on the mature protein (i.e. lacking the signal sequence) from strain MC58.
- strains MC48, M4105, 4243, NZ98/254 are positive for JAR3/JAR 5 reactivity; strains M6190 and 03S-0408 are negative for JAR 3/5 reactivity, and strains NM452 and CDC1573 have not been tested.
- the residues G121 and K122, which are associated with JAR 3 and JAR 5 mAb epitopes, are shown in bold and underlined text. Note that although strain 03S-0408 has G121, it is negative for JAR 3/5 reactivity.
- This strain has three amino acid differences between positions 101 and 146 compared with amino acids of MC58: L109, V114 and S122. Since both L109 and V114 are present in reactive sequences, e.g. 4243 and M4105, lack of reactivity of 03S-0408 is likely attributable to the presence of serine at position 122 instead of lysine and, therefore in addition to G121, K122 also is associated with JAR3/5 reactivity.
- Figure 14 is a schematic showing alignment of fHBP v.2 amino acid sequences with natural polymorphisms in the carboxyl-terminal portion of the B domain and the C domain, or alternatively, the complete fHbpC domain based on the three-dimensional structural nomenclature. The sequence conservation is shown below the alignment (code as in legend to Figure 4 ).
- the residues implicated in anti-fHBP mAb epitopes are designated with the number of the JAR mAb above the alignment: JAR 11 (alanine at residue position 174; A174); JAR 10 (lysine at residue position 180 and glutamate at position 192; K180 and E192); JAR 13 (serine residue at position 216; S216). Numbering in this figure is based on fHBP from strain MC58.
- FIG. 15 is a schematic illustrating additional exemplary chimeric vaccines (Chimeras IIb, III, IV, and V).
- Chimera IIb can be made by introducing the K180R substitution into Chimera II.
- Chimeras III and V can be made using portions of the A and B domains of strain NZ98/254 (subvariant v.1) with the distal portion of the B domain and C domain of v.2 strain 8047 (Chimera III) or of subvariant v.2 strain RM1090 (Chimera V).
- Chimera IV uses the A and proximal B domains of MC58 with the distal B and C domains of RM1090.
- Figure 16 is a schematic showing an alignment of amino acid sequences of further exemplary chimeric fHBPs (Chimera III, IV and V) in the region of the crossover position, which is indicated by the box (residues GEHT).
- the residues, G121 and K122, implicated in the JAR 3 and JAR 5 epitopes are shown in bold and underlining.
- Figure 17 provides a table summarizing cross-reactivity of the different JAR mAbs, their respective Ig isotypes and ability to inhibit binding of human fH.
- Figure 18 is a table listing human complement-mediated bactericidal activity of each of the JAR mAbs when tested individually or in combination with a second anti-fHBP mAb.
- Figure 19 is a series of graphs showing the ability of representative JAR mAbs prepared against fHBP v.2 or v.3 proteins to give concentration-dependent inhibition of binding of fH to rfHBP in an ELISA.
- Panel A Inhibition of binding of fH to rfHBP v.2.
- Panel B Inhibition of binding of fH to rfHBP v.3.
- Respective v.2 and v.3 recombinant proteins are those encoded by the fHBP genes of strains 8047 and M1239.
- Panel C Inhibition of binding of fH to rfHBP v.1.
- Figure 20 is a table listing certain properties of respective pairs of JAR mAbs with or without synergistic complement-mediated bactericidal antibody, including the positions of amino acid residues involved in the epitopes, distances between them, inhibition of fH binding and isotype of each mAb.
- Figure 21 provides the amino acid sequence of variant 1 (v.1) factor H binding protein (fHBP) of MC58, with the A, B and C domains indicated. Positions of the structural domains, fHbpN and fHbpC, are also shown.
- Glutamine 101 (Q) and glycine 164 (G) indicated by upward arrows define the A/B and B/C domain borders, respectively, as defined by Giuliani et al., Infect. Immun, 2005 73:1151-60 .
- the upward arrow at glycine 136 designates the boundary between the fHbpN and the fHbpC domains, as defined by Cantini et al., J. Biol. Chem. 2009 .
- Figure 22 shows the amino- (N-) and carboxyl- (C-) terminal portions of the B and C domains, which are defined with respect to the conserved amino acid sequence of GEHT.
- the amino acid sequences that can define a JAR 3/5 epitope are positioned N-terminal to the second alpha helix; the amino acid sequence that can define the JAR 11/32/35 epitopes are positioned C-terminal to the second alpha helix.
- Alpha-helix (AH) 2 is indicated.
- Figure 23 is a schematic showing Chimera I (MC58/8047) nucleotide and protein sequences. The sequence before the junction (cross-over) point is shown in lower case and the sequence following the junction point is shown in upper case. Lines of fifty residues are shown. Only the Neisserial sequences are shown; E. coli expression constructs contained an N-terminal Methionine and C-terminal hexa-histidine tag (LEHHHHHH).
- Figure 24 is a schematic showing Chimera II (MC58/8047 A174K) nucleotide and protein sequences. The sequence before the junction (cross-over) point is shown in lower case and the sequence following the junction point is shown in upper case. Lines of fifty residues are shown. Only the Neisserial sequences are shown; E. coli expression constructs contained an N-terminal Methionine and C-terminal hexa-histidine tag (LEHHHHHH). The A174K substitution is shown in bold and underlined text.
- Figure 25 is a schematic showing Chimera IIb (MC58/8047 A174K/K180R) nucleotide and protein sequences. The sequence before the junction (cross-over) point is shown in lower case and the sequence following the junction point shown in upper case. Lines of fifty residues are shown. Only the Neisserial sequences are shown; E. coli expression constructs contain an N-terminal Methionine and C-terminal hexa-histidine tag (LEHHHHHH). The A174K and K180R substitutions are shown in bold text.
- Figure 26 is a schematic showing Chimera III (NZ98254/8047) nucleotide and protein sequences. The sequence before the junction (cross-over) point is shown in lower case and the sequence following the junction point is shown in upper case. Lines of fifty residues are shown. Only the Neisserial sequences are shown; E. coli expression constructs contain an N-terminal Methionine and C-terminal hexa-histidine tag (LEHHHHHH).
- Figure 27 is a schematic showing Chimera IV (MC58/RM1090) nucleotide and protein sequences. The sequence before the junction (cross-over) point is shown in lower case and the sequence following the junction point is shown in upper case. Lines of fifty residues are shown. Only the Neisserial sequences are shown; E. coli expression constructs contain an N-terminal methionine and C-terminal hexa-histidine tag (LEHHHHHH).
- Figure 28 is a schematic showing Chimera V (NZ98254/RM1090) nucleotide and protein sequences. The sequence before the junction (cross-over) point is shown in lower case and the sequence following the junction point is shown in upper case. Lines of fifty residues are shown. Only the Neisserial sequences are shown; E. coli expression constructs contain an N-terminal methionine and C-terminal hexa-histidine tag (LEHHHHHH).
- Figure 29 provides a table showing positions of residues associated with JAR mAb binding.
- the reactive residue in fHBP was from the strain used as the source for immunization.
- the reactive strain is 8047, whose fHBP sequence is 99.6% identical to that from strain 2996.
- the non-reactive residue is that present in the non-reactive strain. Loss of reactivity associated with a change from the reactive to the non-reactive residue is indicated as knock-out (KO) and the converse change is indicated as knock-in (KI).
- Figure 30 provides an image of a Western blot indicating residues involved in the JAR 10 and JAR 33 epitopes.
- E. coli lysates containing plasmids expressing the respective wild-type and mutant fHBPs were analyzed by Western blot with JAR 10 (Panel A), Penta-His mAb (Panel B), or JAR 33 (Panel C).
- Figure 31 provides an image of a Western blot indicating a residue involved in the JAR 11, JAR 32 and JAR 35 epitopes.
- E. coli lysates containing plasmids expressing the respective wild-type and mutant fHBPs were analyzed by Western blot with JAR 32 (Panel A), JAR 35 (Panel B), JAR 11 (Panel C) or Penta-His mAb (Panel D).
- Figure 32 provides an image of a Western blot indicating residue involved in the JAR 13 epitope.
- E. coli lysates containing plasmids expressing wild-type and mutant fHBPs: lane 1, molecular weight marker; lane 2, pET21 (empty plasmid); lane 3, fHBP(8047)wt; lane 4, fHBP(8047)S216G; lane 5, fHBP(RM1090)wt; lane 6, fHBP(RM1090)G216S.
- Blots were probed with JAR 13 (Panel A) or Penta-His mAb (Panel B) and anti-mouse IgG-HRP secondary antibody.
- Figure 33 provides an image of a Western blot of wildtype (WT) or Chimeric fHBP expressed in N. meningitidis.
- Lane 1 H44/76 KO fHBP transformed with pCom-fHBP v.2 WT plasmid; 2, H44/76 KO fHbp transformed with pCom-Chimera I plasmid; 3, Kaleidoscope marker; 4, Magic Mark marker; 5, H44/76 (v.1) WT cells; 6, 8047 (v.2) WT cells; 7, 8047 KO fHBP cells; 8, recombinant (r) fHBP v.1 protein (gene from strain MC58); 9, rfHBP v.2 protein (gene from strain 8047).
- Upper panel blot probed with anti-fHBP mAb JAR 3 (v.1); lower panel, blot probed with anti-fHBP mAb JAR 13 (v.2 or v.3).
- Figure 34 shows ribbon diagrams of full length v. 1 fHBPs.
- Panel A, fHBP is partitioned into three domains indicated by various shades of gray.
- the A domain and the N-terminal portion of the B domain are on the left and the boundary between the A and B domains is indicated by an arrow at lysine 100.
- the C-terminal portion of the B domain together with the C domain is on the right, where the boundary between the two is designated by an arrow at glycine 164.
- Panel B an alternative nomenclature describes the fHBP as having two structural domains.
- the N-terminal domain containing a mix of ⁇ helices and ⁇ strands is named the fHbpN domain (left) and the C-terminal domain consisting of ⁇ strands is labeled as the fHbpC domain (right).
- the fHbpN and the fHbpC are connected by a linker at or proximal to glycine 136.
- the junction point relevant for the chimeric fHBP described herein is at or proximal to G136, indicated by an arrow in both panels.
- the models shown in both panels are constructed based on the NMR structure of Cantini et al. J Biol Chem 2009 .
- the present disclosure provides chimeric fHBPs that can elicit antibodies that are bactericidal for different fHBP variant strains of N. meningitidis, and methods of use.
- fHBP Vector H Binding Protein
- GNA1870 GNA 1870
- ORF2086 LP2086 (lipoprotein 2086)
- 741 refers to a polypeptide of N. meningitidis that is a lipoprotein presented on the surface of the bacterium.
- N. meningitidis strains have been sub-divided into three fHBP variant groups (referred to as variant 1 (v.1), variant 2 (v.2), and variant 3 (v.3) in some reports (Masignani et al. 2003, supra ) and Family A and B in other reports (see, e.g., Fletcher et al.
- a leucine residue (L) at position 166 of the v.2 or v.3 fHBP sequence in Figure 3 refers to the residue at position 165 of the v.2 protein and at position 173 in the v.3 protein.
- Figure 4 see Figure 4 for alignment.
- heterologous refers to two components that are defined by structures derived from different sources.
- the chimeric polypeptide includes operably linked amino acid sequences that can be derived from different polypeptides (e.g., a first component from a fHBP v.1 polypeptide and a second component from a fHBP v.2 polypeptide).
- heterologous in the context of a polynucleotide encoding a chimeric polypeptide includes operably linked nucleic acid sequence that can be derived from different genes (e.g., a first component from a nucleic acid encoding a fHBP v.1 polypeptide and a second component from a nucleic acid encoding a fHBP v.2 polypeptide).
- Such chimeric polypeptides as described herein provide for presentation of epitopes in a single polypeptide that are normally found in different polypeptides.
- heterologous nucleic acids include expression constructs in which a nucleic acid comprising a coding sequence is operably linked to a regulatory element (e.g., a promoter) that is from a genetic origin different from that of the coding sequence (e.g., to provide for expression in a host cell of interest, which may be of different genetic origin relative to the promoter, the coding sequence or both).
- a regulatory element e.g., a promoter
- a T7 promoter operably linked to a polynucleotide encoding a fHBP polypeptide or domain thereof is said to be a heterologous nucleic acid.
- Heterologous in the context of recombinant cells can refer to the presence of a nucleic acid (or gene product, such as a polypeptide) that is of a different genetic origin than the host cell in which it is present.
- a Neisserial amino acid or nucleic acid sequence of one strain is heterologous to a Neisserial host of another strain.
- Heterologous as used herein in the context of a chimeric fHBP (e.g., “heterologous fHBP domain”, e.g., a “heterologous B domain", “heterologous C domain”) indicates that the chimeric fHBP protein contains operably linked and contiguous amino acid sequences of structural elements of at least two different fHBP variants (e.g., so as to provide for presentation of epitopes of a v. 1 fHBP, and presentation of a v.2 fHBP and/or a v.3 fHBP in a single fHBP polypeptide).
- a heterologous B domain refers to a polypeptide which comprises a B domain that contains a first portion having a contiguous amino acid sequence of a B domain of a first fHBP variant operably linked to a second portion having a contiguous amino acid sequence of a B domain of a second fHBP variant.
- “Derived from” in the context of an amino acid sequence or polynucleotide sequence is meant to indicate that the polypeptide or nucleic acid has a sequence that is based on that of a reference polypeptide or nucleic acid (e.g., a naturally occurring fHBP protein or encoding nucleic acid), and is not meant to be limiting as to the source or method in which the protein or nucleic acid is made.
- a reference polypeptide or nucleic acid e.g., a naturally occurring fHBP protein or encoding nucleic acid
- “Derived from” in the context of bacterial strains is meant to indicate that a strain was obtained through passage in vivo, or in in vitro culture, of a parental strain and/or is a recombinant cell obtained by modification of a parental strain.
- Constant amino acid substitution refers to a substitution of one amino acid residue for another sharing chemical and physical properties of the amino acid side chain (e.g., charge, size, hydrophobicity/hydrophilicity). "Conservative substitutions” are intended to include substitution within the following groups of amino acid residues: gly, ala; val, ile, leu; asp, glu; asn, gln; ser, thr; lys, arg; and phe, tyr. Conservative amino acid substitutions in the context of a chimeric fHBP disclosed herein are selected so as to preserve presentation of an epitope of interest. Guidance for such substitutions can be drawn from alignments of amino acid sequences of polypeptides presenting the epitope of interest.
- protective immunity means that a vaccine or immunization schedule that is administered to a mammal induces an immune response that prevents, retards the development of, or reduces the severity of a disease that is caused by Neisseria meningitidis, or diminishes or altogether eliminates the symptoms of the disease.
- Protective immunity can be accompanied by production of bactericidal antibodies. It should be noted that production of bactericidal antibodies against Neisseria meningitidis is accepted in the field as predictive of a vaccine's protective effect in humans. ( Goldschneider et al., 1969, J. Exp. Med. 129:1307 ; Borrow et al. 2001 Infect Immun. 69:1568 ).
- a disease caused by a strain of capsular group B of Neisseria meningitidis encompasses any clinical symptom or combination of clinical symptoms that are present in an infection of a human with a member of capsular group B of Neisseria meningitidis. These symptoms include but are not limited to: colonization of the upper respiratory tract ( e.g.
- mucosa of the nasopharynx and tonsils by a pathogenic strain of capsular group B of Neisseria meningitidis, penetration of the bacteria into the mucosa and the submucosal vascular bed, septicemia, septic shock, inflammation, haemmorrhagic skin lesions, activation of fibrinolysis and of blood coagulation, organ dysfunction such as kidney, lung, and cardiac failure, adrenal hemorrhaging and muscular infarction, capillary leakage, edema, peripheral limb ischaemia, respiratory distress syndrome, pericarditis and meningitis.
- broad spectrum protective immunity means that a vaccine or immunization schedule elicits "protective immunity” against at least more than one strain (and can be against at least two, at least three, at least four, at least five, against at least eight, or more strains) of Neisseria meningitidis, wherein each of the strains expresses a different fHBP subvariant or fHBP variant.
- the present disclosure specifically contemplates and encompasses a vaccine or vaccination regimen that confers protection against a disease caused by a member of any capsular group (e.g., A, B, or C), with protection against disease caused by a capsular group B strain of Neisseria meningitidis being of interest due to the epidemiological prevalence of strains causing disease with this capsular group and lack of broadly effective group B vaccines.
- a member of any capsular group e.g., A, B, or C
- an antibody or “specifically immunoreactive with”, in the context of an antigen (e.g., a polypeptide antigen) refers to a binding reaction which is based on and/or is probative of the presence of the antigen in a sample which may also include a heterogeneous population of other molecules.
- an antigen e.g., a polypeptide antigen
- the specified antibody or antibodies bind(s) to a particular antigen or antigens in a sample and do not bind in a significant amount to other molecules present in the sample.
- an antibody or “specifically immunoreactive with” in the context of an epitope of an antigen (e.g., an epitope of a polypeptide) refers to a binding reaction which is based on and/or is probative of the presence of the epitope in an antigen (e.g., polypeptide) which may also include a heterogeneous population of other epitopes, as well as a heterogeneous population of antigens.
- the specified antibody or antibodies bind(s) to a particular epitope of an antigen and do not bind in a significant amount to other epitopes present in the antigen and/or in the sample.
- Immune response indicators include but are not limited to: antibody titer or specificity, as detected by an assay such as enzyme-linked immunoassay (ELISA), bactericidal assay, flow cytometry, immunoprecipitation, Ouchter-Lowny immunodiffusion; binding detection assays of, for example, spot, Western blot or antigen arrays; cytotoxicity assays, etc.
- an assay such as enzyme-linked immunoassay (ELISA), bactericidal assay, flow cytometry, immunoprecipitation, Ouchter-Lowny immunodiffusion
- binding detection assays of, for example, spot, Western blot or antigen arrays
- cytotoxicity assays etc.
- a "surface antigen” is an antigen that is present in a surface structure of Neisseria meningitidis (e.g. the outer membrane, inner membrane, periplasmic space, capsule, pili, etc.).
- isolated refers to an entity of interest that is in an environment different from that in which the compound may naturally occur. "Isolated” is meant to include compounds that are within samples that are substantially enriched for the compound of interest and/or in which the compound of interest is partially or substantially purified.”
- Enriched means that a sample is non-naturally manipulated (e.g., by an experimentalist or a clinician) so that a compound of interest is present in a greater concentration (e.g., at least a three-fold greater, at least 4-fold greater, at least 8-fold greater, at least 64-fold greater, or more) than the concentration of the compound in the starting sample, such as a biological sample (e.g., a sample in which the compound naturally occurs or in which it is present after administration), or in which the compound was made (e.g., as in a bacterial polypeptide, antibody, chimeric polypeptide, and the like)
- a biological sample e.g., a sample in which the compound naturally occurs or in which it is present after administration
- the compound was made e.g., as in a bacterial polypeptide, antibody, chimeric polypeptide, and the like
- a “knock-out” or “knockout” of a target gene refers to an alteration in the sequence of the gene that results in a decrease of function of the target gene, e.g., such that target gene expression is undetectable or insignificant, and/or the gene product is not functional or not significantly functional.
- a “knockout” of a gene involved in LPS synthesis indicates means that function of the gene has been substantially decreased so that the expression of the gene is not detectable or only present at insignificant levels and/or a biological activity of the gene product (e.g., an enzymatic activity) is significantly reduced relative to prior to the modification or is not detectable.
- “Knock-outs” encompass conditional knock-outs, where alteration of the target gene can occur upon, for example, exposure to a predefined set of conditions (e.g., temperature, osmolarity, exposure to substance that promotes target gene alteration, and the like.
- a “knock-in” or “knockin” of a target gene refers to a genetic alteration in a host cell genome that that results in an increase in a function provided by the target gene,
- fHBP Two nomenclature systems have been adopted to describe fHBP: one, which for convenience divided the protein into three domains, designated A, B and C ( Giuliani et al., Infect Immun 2005; 73:1151-60 ), and the other based on three-dimensional structural data.
- A, B and C the protein into three domains
- fHBP is divided into two domains: the fHbpN and the fHbpC. Details of each of these domains with reference to the amino acid sequence of v.1 fHBP of MC58 strain is described below.
- fHBP as having an "A domain", a "B domain", and a "C domain”.
- the amino acid sequence of the v.1 fHBP of the MC58 strain along with the boundaries of the A, B and C domains is shown in Fig. 21 .
- the Q101 and G164 residues indicated by the upward arrows denote the A/B and B/C domain boundaries, respectively.
- the " ⁇ " symbols indicate the position of the first and second ⁇ helices of the fHBP (referred to as AH1 and AH2).
- Residues GEHT are underlined followed by the second ⁇ helix (AH2) of fHBP.
- Panel A in Fig. 34 also shows a ribbon diagram of the full length fHBP with the A, B, and C domains indicated as various shades of gray.
- Fig. 3 provides a schematic of a truncated structural model of fHBP having operably linked B and C domains (the A domain and a portion of the N-terminal portion of the B domain are not shown).
- the native v.1 fHBP of MC58 was again used as a reference sequence for purposes of residue numbering. Amino acid residues identified by site-directed mutagenesis of fHBP that contribute to binding of nine anti-fHBP mAbs (referred to as "JAR" mAbs) are noted. Coordinates from the solution structure of the B and C domains of fHBP from strain MC58 were used to construct the model.
- the ⁇ helix of the B domain is illustrated, as are the loops and ⁇ strands of the C domain.
- fHBP is described as having two structural domains as opposed to the three domains described above.
- the two-domain nomenclature system is based on structural information of a full-length fHBP from which three-dimensional models may be constructed, such as the ones shown in Fig. 34 .
- Structural modeling reveals that full-length fHBP is found to exist in solution as two separate domains connected by a linker.
- the amino acid sequence of the v.1 fHBP of the MC58 strain is shown in Fig. 21 with end of the fHbpN domain indicated with an arrow at glycine 136.
- the N-terminal domain is named fHbpN (residues 8-136) and the C-terminal domain fHbpC (residues 141-255), each comprising at least 8 antiparallel ⁇ strands and joined by a native linker (residues 137-140).
- the linker also comprises ⁇ -helix AH2 as " ⁇ " below the sequence in Fig. 21 marks the positions of ⁇ helices that reside in fHBP.
- the fHbpC domain is considered to include the linker that connects the N-terminal and C-terminal domains based on the convention of this nomenclature.
- fHBP has been divided into three variant groups (referred to as variant 1 (v.1), variant 2 (v.2), and variant 3 (v.3)) based on amino acid sequence variability and immunologic cross-reactivity ( Masignani et al. 2003 J Exp Med 197:789-99 ).
- fHBP has also been subdivided into two sub-families designated sub-family A (which includes v.2 and v.3 of Masignani et al., 2003 J Exp Med 197:789-99 ) and sub-family B (v.1) ( Fletcher et al., 2004, Infect Immun. 72: 2088-100 ).
- Variant as used in the context of an "fHBP variant” refers to an fHBP that share at least 89% amino acid sequence identity with the prototype strain of that variant group (strain MC58 for v.1; strain 2996 for v.2; and strain M1239 for v.3). These were the original prototype sequences described by Masignani et al., J. Exp. Med., 2003 . Strains within a variant group encode fHBPs with greater than 88% amino acid identity, whereas strains of different fHBP variant groups range from approximately 60-88% identical.
- fHBPs in the same "variant" group possess greater than 88% identity to the respective prototype sequence (v.1, strain MC58; v.2, strain 2996; v.3, strain M1239).
- a "subvariant" as used in the context of an "fHBP subvariant” refers to fHBP polypeptides that differ from the prototype sequence.
- strain NZ98/254 is referred to as an fHBP v. 1 subvariant, with 91% identity to the prototype sequence from strain MC58; strain RM1090 is referred to as an fHBP v.2 subvariant, with a sequence that is 94% identical to the v.2 prototype strain 2996. Examples of subvariants, and their relative amino acid sequence identities, are provided in Figures 8A and 8B .
- fHBP polypeptides, and encoding nucleic acids, from which portions of the chimeric fHBPs of the present disclosure can be derived may be from any suitable N. meningitidis strain.
- N. meningitidis strains are divided into serologic groups (capsular groups), serotypes (PorB phenotypes) and subtypes (PorA phenotypes) on the basis of reactions with polyclonal ( Frasch, C. E. and Chapman, 1973, J. Infect. Dis. 127: 149-154 ) or monoclonal antibodies that interact with different surface antigens.
- Capsular grouping traditionally has been based on immunologically detectable variations in the capsular polysaccharide but is being replaced by PCR of genes encoding specific enzymes responsible for the biosynthesis of the structurally different capsular polysaccharides.
- About 12 capsular groups (including A, B, C, X, Y, Z, 29-E, and W-135) are known. Strains of the capsular groups A, B, C, Y and W-135 account for nearly all meningococcal disease.
- Serotyping traditionally has been based on monoclonal antibody defined antigenic differences in an outer membrane protein called Porin B (PorB). Antibodies defining about 21 serotypes are currently known ( Sacchi et al., 1998, Clin. Diag. Lab. Immunol.
- Serosubtyping has been based on antibody defined antigenic variations on an outer membrane protein called Porin A (PorA). Both serotyping and serosubtyping are being replaced by PCR and/or DNA sequencing for identification of genes encoding the variable regions of PorB and PorA, respectively that are associated with mAb reactivity (e.g. Sacchi, Lemos et al., supra; Urwin et al., 1998, Epidem. and Infect. 120:257 ).
- N. meningitidis also may be divided into clonal groups or subgroups, using various techniques that directly or indirectly characterize the bacterial genome. These techniques include multilocus enzyme electrophoresis (MLEE), based on electrophoretic mobility variation of an enzyme, which reflects the underlying polymorphisms at a particular genetic locus. By characterizing the variants of a number of such proteins, genetic "distance" between two strains can be inferred from the proportion of mismatches. Similarly, clonality between two isolates can be inferred if the two have identical patterns of electrophoretic variants at number of loci.
- MLEE multilocus enzyme electrophoresis
- MLST multilocus sequence typing
- N. meningitidis strains of any capsular group may be used, N . meningitidis strains of capsular group B are of particular interest as sources from which nucleic acid encoding fHBP and domains thereof are derived.
- the chimeric fHBP can contain amino acid sequences that are at least 80%, at least 85%, at least 90%, or at least 95% identical to an amino acid sequence of a naturally-occurring fHBP.
- Nucleic acids encoding fHBP polypeptides for use in construction of chimeric fHBPs contemplated herein are known in the art. Exemplary fHBP polypeptides are described in, for example, WO 2004/048404 ; Masignani et al. 2003 J Exp Med 197:789-799 ; Fletcher et al. Infect Immun 2004 2088-2100 ; Welsch et al. J Immunol 2004 172:5606-5615 ; and WO 99/57280 . Nucleic acid (and amino acid sequences) for fHBP variants and subvariants are also provided in GenBank as accession nos.: NC_003112, GeneID: 904318 (NCBI Ref.
- NP_274866 (from N. meningitidis strain MC58); AY548371 (AAT01290.1) (from N. meningitidis strain CU385); AY548370 (AAT01289.1) (from N. meningitidis strain H44/76); AY548377 (AAS56920.1) (from N. meningitidis strain M4105); AY548376 (AAS56919.1) (from N. meningitidis strain M1390); AY548375 (AAS56918.1) (from N . meningitidis strain N98/254); AY548374 (AAS56917.1) (from N.
- the immature fHBP protein includes a leader sequence of about 19 residues.
- the ordinarily skilled person can readily envision the sequences of nucleic that can encode for, and provide for expression of, a polypeptide having such an amino acid sequence.
- polypeptides and nucleic acids having sequences that are at least 80%, at least 85%, at least 90%, or at least 95% identical in sequence to such exemplary amino acid and nucleic acids.
- nucleic acid sequences refers to two or more sequences or subsequences that are the same or have a specified percentage of amino acid residues or nucleotides that are the same (e.g., at least 80%, at least 85%, at least 90%, or at least 95% identical over a specified region), when compared and aligned for maximum correspondence over a designated region, e.g., a B domain or portion thereof, e.g., a region at least about 30, 35, 40, 45, 50, 55, 60, 65 or more amino acids or nucleotides in length, and can be up to the full-length of the reference amino acid or nucleotide sequence (e.g., a full-length fHBP).
- the disclosure specifically contemplates both naturally-occurring polymorphisms and synthetically produced amino acid sequences and their encoding nucleic acids.
- sequence comparison typically one sequence acts as a reference sequence (e.g., a naturally-occurring fHBP polypeptide sequence), to which test sequences are compared.
- a reference sequence e.g., a naturally-occurring fHBP polypeptide sequence
- test and reference sequences are input into a computer program, subsequence coordinates are designated, if necessary, and sequence algorithm program parameters are designated.
- sequence comparison algorithm then calculates the percent sequence identity for the test sequence(s) relative to the reference sequence, based on the designated program parameters.
- BLAST and BLAST 2.0 algorithms are described in Altschul et al. (1990) J. Mol. Biol. 215: 403-410 and Altschul et al. (1977) Nucleic Acids Res. 25: 3389-3402 , respectively.
- Software for performing BLAST analyses is publicly available through the National Center for Biotechnology Information (www.ncbi.nlm.nih.gov).
- Further exemplary algorithms include ClustalW ( Higgins D., et al. (1994) Nucleic Acids Res 22: 4673-4680 ), available at www.ebi.ac.uk/Tools/clustalw/index.html.
- residue positions which are not identical differ by conservative amino acid substitutions.
- Conservative amino acid substitutions refer to the interchangeability of residues having similar side chains.
- a group of amino acids having aliphatic side chains is glycine, alanine, valine, leucine, and isoleucine
- a group of amino acids having aliphatic-hydroxyl side chains is serine and threonine
- a group of amino acids having amide-containing side chains is asparagine and glutamine
- a group of amino acids having aromatic side chains is phenylalanine, tyrosine, and tryptophan
- a group of amino acids having basic side chains is lysine, arginine, and histidine
- a group of amino acids having sulfur-containing side chains is cysteine and methionine.
- Sequence identity between two nucleic acids can also be described in terms of hybridization of two molecules to each other under stringent conditions.
- the hybridization conditions are selected following standard methods in the art (see, for example, Sambrook, et al., Molecular Cloning: A Laboratory Manual, Second Edition, (1989) Cold Spring Harbor, N.Y .).
- An example of stringent hybridization conditions is hybridization at 50°C or higher and 0.1 ⁇ SSC (15 mM sodium chloride/1.5 mM sodium citrate).
- Stringent hybridization conditions are hybridization conditions that are at least as stringent as the above representative conditions, where conditions are considered to be at least as stringent if they are at least about 80% as stringent, typically at least 90% as stringent as the above specific stringent conditions.
- the chimeric fHBP of the present disclosure is described in more detail below in the context of both the nomenclature dividing the protein into three domains used by Giuliani et al. (Infect Immun 2005; 73:1151-60 ) and the three-dimensional structural nomenclature.
- fHBP may be described as having the following three domains to facilitate analysis: A domain, B domain, and C domain.
- a domain As shown in Fig. 21 , the upward arrows at Q101 and G164 demarcate the boundaries between A/B domains and B/C domains, respectively.
- the chimeric fHBPs of the present disclosure optionally include an A domain.
- the A domain can be structurally defined as those residues corresponding to residues 1-100 of v.1 fHBP of MC58, where the numbering is based on amino acid sequence of MC58 v.1 fHBP lacking the signal sequence ( Masignani et al., 2003 J Exp Med 197:789-99 ) (see Figure 21 ).
- Chimeric fHBPs which contain an A domain can contain a contiguous A domain amino acid sequence that is at least 85%, at least 90%, or at least 95% identical to an amino acid sequence of an A domain of a naturally occurring fHBP.
- the A domain may be derived from the same variant group (and may be derived from the same fHBP) as the N-terminal portion of the B domain, such that the amino acid sequence at the A/B junction is one that may be found in nature.
- the A domain amino acid sequence may be derived from a fHBP variant group different from the fHBP variant group from which the N-terminal amino acid sequence of the B domain is derived (e.g., the A domain may be derived from a v.2 fHBP and the N-terminal amino acid sequence of the B domain derived from a v.1 fHBP).
- the chimeric fHBPs of the present disclosure contain amino acid sequence of a v.1 fHBP B domain.
- Amino acid sequences of v.1 fHBP, including v.1 fHBP B domains, are well known in the art and can be used to derive the desired amino acid sequence of a chimeric fHBP disclosed herein.
- Fig. 13 provides the amino acid sequences of an N-terminal portion of the B domain of selected v. 1 fHBPs. The alignment illustrates the position and identity of naturally occurring polymorphisms among v.1 fHBPs.
- Figure 8A illustrates the amino acid sequence identity between full length fHBPs of exemplary v.1, v.2 and v.3 strains, and further illustrates the presence or absence of epitopes defined by the indicated JAR mAbs.
- Figure 8B illustrates the amino acid sequence identity between the A, B, and C domains of exemplary v.1, v.2 and v.3 fHBPs, as well as amino acid sequence identity within the N-terminal (101-135) and C-terminal (136-164) portions of B domains.
- Fig. 21 shows the amino acid sequence of the fHBP of the v.1 strain MC58, and illustrates the position and of a full-length B domain (defined by residues 101-164 and encompassing the amino acid sequence of GEHT followed by ⁇ -helix AH2).
- Fig. 22 Panel A illustrates that an N-terminal portion of the B domain of the v.1 fHBP of the MC58 strain, can encompass an amino acid sequence defined by residues corresponding to residues N-terminal of the GEHT residues and extending to the N-terminus of the B domain at a residue corresponding to residue 101.
- 1 fHBP of the MC58 strain can encompass an amino acid sequence defined by those residues corresponding to an amino acid sequence extending N-terminally from residue 164 of the B domain, and encompassing up to and including the amino acid sequence of GEHT.
- a full-length B domain is structurally defined by the residues corresponding to residues 101-164 of the v.1 of fHBP of MC58, where residues 101-135 can define an exemplary N-terminal portion of the B domain and residues 136-164 can define an exemplary C-terminal portion of the B domain, where the numbering is based on amino acid sequence of MC58 v.1 fHBP lacking the signal sequence ( Masignani et al., 2003 J Exp Med 197:789-99 ).
- the C-terminus of the N-terminal portion of the B domain (and thus the N-terminus of the C-terminal portion of the heterologous B domain) is defined by the position of the junction point, which can be present N-terminal or C-terminal to the amino acid sequence of GEHT, as discussed below in more detail.
- the junction point of a heterologous B domain of a chimeric fHBP can be positioned C-terminal to a sequence corresponding to the GEHT, and thus can extend beyond a residue corresponding to residue 135.
- Exemplary chimeric fHBP include those comprising a B domain having a contiguous amino acid sequence that is at least 80%, at least 85%, at least 90%, or at least 95% identical to an N-terminal B domain amino acid sequence of a v.1 fHBP, e.g., at least 80%, at least 85%, at least 90%, or at least 95% identical to a contiguous amino acid sequence of the N-terminal B domain amino acid sequence exemplified in Fig. 13 .
- Exemplary chimeric fHBP having a heterologous B domain contain at least 35, at least 40, at least 45, at least 50 residues (and in some embodiments no more than 50 residues) of a contiguous N-terminal amino acid sequence of a B domain of a v.1 fHBP.
- Exemplary chimeric fHBPs of the present disclosure contain a heterologous B domain containing an N-terminal amino acid sequence derived from an N-terminal portion of a v. 1 fHBP B domain and the remaining C-terminal portion derived from the corresponding C-terminal portion of a v.2 (or v.3) fHBP B domain, followed by the contiguous amino acid sequence of a v.2 (or v.3) C domain.
- the C domain can be structurally defined as those residues corresponding to residues 165-255 of v.1 fHBP of MC58, where the numbering is based on amino acid sequence of MC58 v.1 fHBP lacking the signal sequence ( Masignani et al., 2003 J Exp Med 197:789-99 ) (see Figure 21 ).
- Amino acid sequences of v.2 and v.3 fHBP are well known in the art and can be used to derive the desired amino acid sequence of a chimeric fHBP disclosed herein.
- Fig. 14 provides the amino acid sequences of a C-terminal portion of the B domain (as exemplified by the C-terminal 25 amino acids of v.2 fHBP B domain) and the full-length C domains of selected v.2 fHBPs.
- the alignment illustrates the position and identity of naturally occurring polymorphisms among v.2 fHBPs.
- Exemplary chimeric fHBP include those comprising a B domain containing a C-terminal amino acid sequence derived from a v.2 or v.3 B domain, usually having a contiguous amino acid sequence that is greater than or at least 85%, at least 90%, or at least 95% identical to an C-terminal B domain amino acid sequence of a v.2 or v.3 fHBP, e.g., at least 80%, at least 85%, at least 90%, or at least 95% identical to a contiguous amino acid sequence of the N-terminal B domain amino acid sequence, such as those v.2 sequences exemplified in Fig. 14 .
- the B domain can be at least 80%, at least 85%, at least 90%, or at least 95% identical to a contiguous amino acid sequence of a full-length B domain amino acid sequence of a v. 1 fHBP.
- a full-length B domain of a v.1 fHBP generally is about 64 residues in length.
- fHBP may also be described has having two structural domains: fHbpN and fHbpC, based on an alternative nomenclature that is derived from the structure of the full-length fHBP.
- glycine 136 marks approximately the beginning of a linker between the N-terminal and the C-terminal domains, named the fHbpN and fHbpC domains, respectively.
- the chimeric fHBP of the present disclosure may include a full-length fHbpN domain or a partial fHbpN domain.
- the fHbpN domain can be structurally defined as those residues corresponding to residues 1-136 of v.1 fHBP of MC58, where the numbering is based on amino acid sequence of MC58 v.1 fHBP lacking the signal sequence ( Masignani et al., 2003 J Exp Med 197:789-99 ) (see Fig. 21 ).
- the respective amino acid sequences of the first 100 residues of the fHbpN domain normally share significant amino acid sequence identity ( Fig. 8B ).
- Chimeric fHBP which contains an fHbpN domain can contain a contiguous fHbpN domain amino acid sequence that is at least 85%, at least 90%, or at least 95% identical to an amino acid sequence of an fHbpN domain of a naturally occurring fHBP.
- the chimeric fHBP may include a partial fHbpN domain, such that an N-terminal portion of the fHbpN is truncated.
- the partial fHbpN domain may comprise at least 30, 40, or 50 of a contiguous C-terminal amino acid sequence of the full length fHbpN domain.
- Exemplary chimeric fHBPs include those comprising a full or partial fHbpN domain having a contiguous amino acid sequence that is at least 80%, at least 85%, at least 90%, or at least 95% identical to at least a C-terminal portion of the fHbpN amino acid sequence of a v.1 fHBP, e.g., at least 80%, at least 85%, at least 90%, or at least 95% identical to a contiguous amino acid sequence of the C-terminal fHbpN amino acid sequence exemplified in Fig. 13 .
- An exemplary chimeric fHBP having heterologous domains contains at least 35, at least 40, at least 45, at least 50 residues (and in some embodiments no more than 50 residues) of a contiguous C-terminal amino acid sequence of an fHbpN domain of a v.1 fHBP.
- the full or partial fHbpN domain may be derived from the same variant group (and may be derived from the same fHBP) as certain portions of the fHbpC domain.
- the fHbpN amino acid sequence may be derived from a fHBP variant group different from the fHBP variant group from which the N-terminal amino acid sequence of the fHbpC domain is derived (e.g., the fHbpC domain may be derived from a v.2 fHBP and the C-terminal amino acid sequence of the fHbpN domain derived from a v.1 fHBP).
- the chimeric fHBPs of the present disclosure contain amino acid sequence of a v.1 fHbpN domain.
- Amino acid sequences of v.1 fHBP, including v.1 fHbpN domains, are well known in the art and can be used to derive the desired amino acid sequence of a chimeric fHBP disclosed herein.
- Fig. 13 provides the C-terminal amino acid sequences of the fHbpN domain of selected v.1 fHBPs. The alignment illustrates the position and identity of naturally occurring polymorphisms among v.1 fHBPs.
- Figure 8A illustrates the amino acid sequence identity between full length fHBPs of exemplary v.1, v.2 and v.3 strains, and further illustrates the presence or absence of epitopes defined by the indicated JAR mAbs.
- Figure 8B illustrates the amino acid sequence identity between exemplary v.1, v.2 and v.3 fHBPs, as well as amino acid sequence identity within the C-terminal portion of the fHbpN (101-135) and N-terminal (136-164) portion of the fHbpC domains.
- the position of the junction point between heterologous domains can be present within or proximal to the linker that connects the fHbpN and the fHbpC domains.
- Glycine 136 defines the boundary between fHbpN and fHbpC and also marks the beginning of the linker sequence.
- the linker sequence corresponds approximately to residues 136 to 149 and includes ⁇ -helix AH2.
- the junction point between heterologous domains of a chimeric fHBP can be positioned C-terminal to a sequence corresponding to the GEHT sequence underlined in Fig.
- the junction may be no more than 20, no more than 15, no more than 5 or less amino acid residues away from the amino acid sequence of GEHT or the linker sequence.
- the junction between the heterologous domains may be positioned C-terminal to glycine 164.
- Glycine 164 is also indicated by an arrow in Fig. 21 .
- Exemplary chimeric fHBPs of the present disclosure contain heterologous domains comprising a full or partial fHbpN domain of a v.1 fHBP fHbpN domain and a fHbpC domain derived from the fHbpC of a v.2 (or v.3) fHBP.
- the fHbpC domain can be structurally defined as those residues corresponding to residues 141-255 of v.1 fHBP of MC58, where the numbering is based on amino acid sequence of MC58 v.1 fHBP lacking the signal sequence ( Masignani et al., 2003 J Exp Med 197:789-99 ) ( Fig. 21 ).
- Amino acid sequences of v.2 and v.3 fHBP including v.2 and v.3 fHBP fHbpN and fHbpC domains, are well known in the art and can be used to derive the desired amino acid sequence of a chimeric fHBP disclosed herein.
- Fig. 14 provides the amino acid sequences of the full-length fHbpC domains of selected v.2 fHBPs. The alignment illustrates the position and identity of naturally occurring polymorphisms among v.2 fHBPs.
- Exemplary chimeric fHBPs include those comprising an fHbpC amino acid sequence derived from a v.2 or v.3 fHbpC domain, usually having a contiguous amino acid sequence that is greater than or at least 85%, at least 90%, or at least 95% identical to the amino acid sequence of the fHbpC domain of a v.2 or v.3 fHBP, e.g., at least 80%, at least 85%, at least 90%, or at least 95% identical to a contiguous amino acid sequence of the fHbpC domain amino acid sequence, such as those v.2 sequences exemplified in Fig. 14 .
- fHbpC domain may contain two contiguous amino acid sequences derived from different variants.
- a contiguous N-terminal amino acid sequence of fHbpC can be at least 80%, at least 85%, at least 90%, or at least 95% identical to a contiguous amino acid sequence of the corresponding amino acid sequence of a v.1 fHBP.
- fHBP may be described in the context of the three domains assigned by Giuliani et al (Infect Immun 2005; 73:1151-60 ) or in the context of two three-dimensional structural domains.
- the disclosure will adopt the nomenclature of the three domains, designated A, B, and C domains.
- all discussion in the context of the three functional domains can be readily understood in the context of the two structural domains based on what has been detailed above.
- the chimeric fHBPs of the present disclosure generally include either a heterologous B domain and a C domain; or a B domain and a heterologous C domain.
- Such chimeric fHBPs are constructed so as to contain epitopes that elicit bactericidal antibodies effective against N. meningitidis strains producing more than one fHBP variant.
- chimeric factor H binding protein or "chimeric fHBP” refers to a polypeptide comprising, from N-terminus to C-terminus, an amino acid sequence of a B domain and of a C domain, wherein at least one of the B domain and the C domain contains a heterologous amino acid sequence characterized as having an N-terminal portion derived from a contiguous amino acid sequence of a v.1 fHBP with the remaining B and C-terminal portion (or C terminal portion) being derived from a contiguous amino acid sequence of a v.2 or v.3 fHBP.
- the B domain and/or C domain amino acid sequences are generally derived from a contiguous amino acid sequence of a naturally-occurring fHBP and mutants thereof that maintain or introduce desired epitopes.
- Chimeric fHBP can optionally include an amino acid sequence of an fHBP A domain operably linked and N-terminal to the B domain.
- Chimeric fHBP can further optionally include a leader sequence, e.g., to provide for expression of the chimeric fHBP on a cell surface of a bacterial host cell.
- the heterologous B domain generally comprises at least an N-terminal portion derived from a contiguous amino acid sequence of a v.1 fHBP B domain and a C-terminal portion derived from a contiguous amino acid sequence of a v.2 or v.3 B domain, with the heterologous B domain being operably linked to a C domain derived from a contiguous amino acid sequence of a v.2 or v.3 fHBP C domain.
- such chimeric fHBP can be described as having a heterologous B domain composed of an N-terminal portion for which a corresponding contiguous amino acid sequence of a v.1 fHBP B domain sequence serves as a scaffold, and a C-terminal portion for which a corresponding contiguous amino acid sequence of a v.2 or v.3 fHBP B domain sequence serves as a scaffold.
- exemplary chimeric fHBP having a heterologous B domain contain at least 35, at least 40, at least 45, at least 50 residues (and in some embodiments no more than 50 residues) of a contiguous N-terminal amino acid sequence of a B domain of a v.1 fHBP.
- the B domain of the chimeric fHBP comprises a contiguous amino acid sequence of a v.1 fHBP B domain operably linked to heterologous C domain comprising at least an N-terminal portion of a v. 1 fHBP C domain and a C-terminal portion of a v.2 or v.3 C domain.
- Exemplary chimeric fHBP of this embodiment contain 2, 4, 6, 8 residues of an N-terminal sequence of a v.1 C domain, with the remainder of the C domain being derived from a v.2 or v.3 C domain amino acid sequence.
- Chimeric fHBP contemplated by the present disclosure include those having an amino acid sequence corresponding to a full-length B domain and a full-length C domain, and, optionally, a full-length A domain wherein the chimeric fHBP includes at least a heterologous B domain or a heterologous C domain.
- Other embodiments include chimeric fHBP having an amino acid sequence corresponding to a fragment of an A domain composed of a contiguous amino acid sequence encompassing amino acid defining an epitope bound by the JAR 4 mAb.
- chimeric fHBP in which the C domain is truncated at the C-terminus, with the proviso that epitopes of interest (e.g., one or more of the epitopes bound by mAbs JAR 10, JAR 11, JAR 33, JAR 32/35, and JAR 13) are preserved so as to retain the ability to elicit antibodies that bind these epitopes.
- Chimeric fHBP also include those that lack an A domain, and have an N-terminally truncated B domain, with the proviso that the truncated B domain maintains expression of an epitope(s) of interest.
- Chimeric fHBP include those having a B domain that expresses an epitope bound by the JAR 5 mAb.
- Chimeric polypeptides described herein can include additional heterologous amino acid sequences, e.g., to provide an N-terminal methionine or derivative thereof (e.g., pyroglutamate) as a result of expression in a bacterial host cell (e.g., E. coli ) and/or to provide a chimeric polypeptide having a fusion partner at its N-terminus or C-terminus.
- Fusion partners of interest include, for example, glutathione-S-transferase (GST), maltose binding protein (MBP), His 6 -tag, and the like, as well as leader peptides from other proteins, particularly lipoproteins. Fusion partners can provide for additional features, such as in facilitating isolation and purification of the chimeric polypeptide.
- Native fHBP usually contains an N-terminal cysteine to which a lipid moiety can be covalently attached.
- This cysteine residue is usually lipidated in the naturally-occurring protein, and can be lipidated in the chimeric fHBPs disclosed herein.
- reference to "cysteine” or "C” at this position specifically includes reference to both an unmodified cysteine as well as to a cysteine that is lipidated (e.g., due to post-translational modification).
- the chimeric fHBP can be lipidated or non-lipidated.
- lipidated proteins in vitro, (see, e.g., Andersson et al., 2001 J. Immunological Methods 255(1-2):135-48 ) or in vivo are known in the art.
- lipidated fHBP previously has been purified from the membrane fraction of E. coli protein by detergent extraction ( Fletcher et al., 2004 Infection and Immunity 72(4):2088-100 ), which method may be adapted for the production of lipidated chimeric fHBP.
- Lipidated proteins may be of interest as such can be more immunogenic than soluble protein (see, e.g., Fletcher et al., 2004 Infection and Immunity 72(4):2088-100 ).
- chimeric fHBPs of the present disclosure encompass those that can be described in terms of one or more of, for example, the site at which heterologous sequences are joined within the chimeric fHBP (i.e., the "junction point"), the presence of epitopes specifically bound by a mAb, amino acid sequence, or any combination of such features that may be present in exemplary fHBPs.
- the junction point of the chimeric fHBP is the point at which amino acid sequence of the chimeric fHBP shifts from being derived from a contiguous amino acid sequence of a v.1 fHBP to being derived from contiguous amino acid sequence of a v.2 or v.3 fHBP.
- the junction point thus provides for an amino acid sequence that is heterologous, i.e., derived from different fHBPs.
- heterologous domain i.e., heterologous B domain or heterologous C domain
- junction point thus defining the length of the N-terminal and C-terminal portions of the chimeric domain that are derived from a v. 1 or v.2/v.3 amino acid sequence.
- a B domain amino acid sequence comprising an amino acid sequence N-terminal to the second ⁇ helix of fHBP, which includes residues corresponding to those implicated in defining the JAR 5 mAb epitope (i.e., residues at positions 121 and 122 of a B domain v.1 fHBP MC58, which are glycine and lysine, respectively) is denoted as the "N-terminal portion of the B domain" (see, e.g., Fig. 13 , Fig. 21 and Fig. 22 , Panel A).
- the amino acid sequence flanking and C-terminal to the N-terminal portion of the B domain is the "C-terminal (or distal) portion of the B domain" and is derived from a contiguous amino acid sequence of a v.2 or v.3 fHBP ( Fig. 14 and Fig. 22 ). Together, the N-terminal and C-terminal portions of the B domain compose a heterologous B domain of a chimeric fHBP of the present disclosure.
- the junction point may be positioned at a residue adjacent to the second ⁇ helix (AH2) (e.g., adjacent and C-terminal to a residue corresponding to residue 121 or 122 of Figure 21 , e.g., adjacent and C-terminal to one of the residues of GEHTSFDK, e.g., adjacent and C-terminal to one of the residues of GEHT, N-terminal to AH2), or at a position C-terminal to AH2.
- AH2 residue adjacent to the second ⁇ helix
- the junction point of the heterologous B domain can be positioned at any site corresponding to a site after the glycine residue or after the lysine residue, that define a JAR 5 monoclonal antibody (mAb) epitope of a v. 1 fHBP (which residue is positioned within the B domain, i.e., at G121 or K122 of v.1 fHBP strain MC58 reference sequence) but before a residue corresponding to a residue defining a JAR 11 mAb epitope of a v.2 fHBP (which residue is positioned in the C domain, i.e., A174 of v.2 fHBP strain 8047 reference sequence).
- mAb monoclonal antibody
- the heterologous B domain is provided such that the JAR 5 mAb epitope, the JAR 11 epitope, or both the JAR 5 and JAR 11 epitopes are maintained such that the chimeric fHBP is specifically bound by the respective mAb.
- the junction point is positioned so that the chimeric fHBP contains a heterologous B domain, which has an N-terminal portion composed of a contiguous amino acid sequence of an N-terminal portion of a B domain of a v. 1 fHBP containing a JAR 5 epitope (defined in part by G121 of v.1 fHBP strain MC58) with the remaining portion (i.e., the C-terminal portion) of the B domain derived from a contiguous amino acid sequence of the corresponding C-terminal portion of a v.2 or v.3 fHBP B domain.
- a heterologous B domain which has an N-terminal portion composed of a contiguous amino acid sequence of an N-terminal portion of a B domain of a v. 1 fHBP containing a JAR 5 epitope (defined in part by G121 of v.1 fHBP strain MC58) with the remaining portion (i.e., the C-terminal portion
- the heterologous B domain is operably linked to a C domain derived from a contiguous amino acid sequence of a v.2 or v.3 fHBP, which can be the same or different v.2 or v.3 fHBP as that from which the C-terminal portion of the B domain is derived.
- Exemplary heterologous B domains include those at least 80% identical, at least 85% identical, at least 90% identical, at least 99% identical or more to a contiguous amino acid sequence of a v.1 fHBP corresponding to residues 101-121, 101-122, 101-123, 101-124, 101-125, 101-126, 101-127, 101-128, 101-129, 101-130, 101-131, 101-132, 101-133, 101-134, 101-134, 101-136, 101-137, 101-138, or 101-139 of a v.1 fHBP amino acid sequence, where the numbering is based on MC58 fHBP as a reference.
- Such heterologous B domains include those having an amino acid sequence that is at least 80% identical, at least 85% identical, at least 90% identical, at least 99% identical or more to a contiguous amino acid sequence of a v.2 or v.3 fHBP so as to provide the remainder of the heterologous B domain having a C-terminus corresponding to residue 164 (again, using MC58 fHBP as a reference sequence of purposes of numbering).
- the C-terminal portion of the heterologous B domain includes residues 123-164 of a v.2 or v.3 fHBP.
- the C-terminal portion of the heterologous B domain can include an amino acid sequence at least 80% identical, at least 85% identical, at least 90% identical, at least 99% identical or more to a contiguous amino acid sequence of a v.2 or v.3 fHBP corresponding to residues 122-164, 123-164, 124-164, 125-164, 126-164,127-164, 128-164, 129-164, 130-164, 131-164, 132-164, 133-164, 134-164, 135-164, 136-164, 137-164, 139-164, or 140-164, where the N-terminal portion of the heterologous B domain is provided by the v.1 sequences exemplified above.
- the junction point is positioned N-terminal to the second ⁇ helix (AH2), which are denoted in Figure 22 by " ⁇ ".
- AH2 second ⁇ helix
- the residues GEHT are highly conserved across v.1, v.2, and v.3 fHBP variants, and thus can serve as convenient junction point residues, as well as a convenient reference for the position of a junction point in a chimeric fHBP.
- the junction point can be positioned within 14, 13, 12, 11, 10, 9, 8, 7, 6, 5, 4, 3, 2, or 1 residue(s) N-terminal to GEHT to provide a heterologous B domain (e.g., positioned at a site not more than 14, 13, 12, 11, 10, 9, 8, 7, 6, 5, 4, 3, 2, or 1 residue N-terminal of GEHT); or is positioned within 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33 or 34 residues C-terminal to GEHT (e.g., positioned at a site not more than 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33 or 34 residues C-terminal of GEHT), where a junction point at a site less than or equal to 26 residues C-terminal to GEHT provides a heterologous B domain and a junction point positioned at more than 26 residues C-terminal to GEHT produces
- the junction point of the heterologous B domain can be selected such that the heterologous B domain amino acid sequence positioned N-terminal and flanking the amino acid sequence GEHT is derived from a v.1 fHBP B domain amino acid sequence and the heterologous B domain amino acid sequence positioned C-terminal and flanking the GEHT is derived from a v.2 or v.3 fHBP B amino acid sequence.
- the junction point is positioned so as to provide a heterologous B domain comprising an amino acid sequence that is greater than 80% (e.g., at least 81%), at least 85%, at least 90%, at least 95% or identical to an amino acid sequence of
- QSHSALTAFQ TEQIQDSEHS GK (SEQ ID NO: 1) where the amino acid sequence optionally provides for an epitope that mediates specific binding of a JAR 5 mAb.
- Exemplary amino acid substitutions of the above sequence are as follows: QSHSALTA(F/L)Q TEQ(I/V/E)QD(S/P)E(H/D)S (G/E/R)K.
- amino acid sequences of the heterologous B domain as set out above include, for example, one or more of the following substitutions of SEQ ID NO: 1 as follows:
- heterologous B domain comprises an amino acid sequence represented by the formula:
- the junction point is positioned so as to provide a heterologous B domain comprising an amino acid sequence that is at least 80%, at least 85%, at least 90%, at least 95% or identical to an amino acid sequence of TEQIQDSEHS GKMVAKRQFR IGDIAGEHTA FNQLPD, where the amino acid sequence optionally provides for an epitope that mediates specific binding of a JAR 5 mAb.
- the heterologous B domain comprises an amino acid sequence that is at least 80%, at least 85%, at least 90%, at least 95% or identical to an amino acid sequence of QSHSALTA F Q TEQIQDSEHS GKMVAKRQFR IGDIAGEHTA FNQLPD where the amino acid sequence optionally provides for an epitope specifically bound by JAR 5 MAB.
- the heterologous B domain comprises a sequence at least 80%, at least 85%, at least 90%, at least 95% or identical to an amino acid sequence set out in Fig. 13 , which provides an alignment of exemplary chimeric fHBPs III, IV and V sequences in the region of the junction point, which is indicated by the box.
- the residue, G121, implicated in the JAR 5 epitope is shown in bold and underlined.
- the junction point is positioned so as to provide a heterologous B domain comprising an amino acid sequence that is at least 80%, at least 85%, at least 90%, at least 95% or identical to an amino acid sequence of: LTAFQ TEQIQDSEHS GKMVAKRQFR IGDIA where the amino acid sequence optionally provides for an epitope that mediates specific binding of a JAR 5 mAb.
- the junction point of the chimeric fHBP is positioned so that the chimeric fHBP contains a heterologous C domain composed of a contiguous amino acid sequence of an N-terminal portion of a C domain of a v. 1 fHBP and a contiguous amino acid sequence of a C-terminal portion of a C domain of a v.2 or v.3 fHBP.
- junction point of a chimeric fHBP having a heterologous C domain can be in the loop regions of the ⁇ -barrel of the C domain, or in any highly conserved segment, for example at residues D160 or I170.
- the heterologous C domain includes an N-terminal sequence of KLTYTIDFA.
- Exemplary chimeric fHBP are provided in the Examples below.
- the present disclosure contemplates these exemplary chimeric fHBP, as well as chimeric fHBP having at least 85%, at least 90%, at least 95% or greater amino acid sequence identity to the amino acid sequences of these exemplary chimeric fHBP (e.g., Chimera I, Chimera II, Chimera IIb, Chimera III, Chimera IV, and Chimera V).
- the amino acid and nucleic acid sequences encoding Chimera I, Chimera II, Chimera IIb, Chimera III, Chimera IV, and Chimera V are provided in Figures 23, 24 , 25, 26 , 27, and 28 , respectively.
- the asterisk denotes the C-terminus of the amino acid sequence (corresponding to the stop codon of the encoding nucleic acid).
- Chimeric fHBP encompass chimeric fHBP that contain pairs of epitopes that elicit antibodies that, when both are bound to their respective epitopes, exhibit enhanced bactericidal activity against N. meningitidis than when either one is bound alone.
- Chimeric fHBP can be designed so as to ensure that such epitopes are maintained or to introduce such epitopes (e.g., by modification of an fHBP amino acid sequence to include a pair of epitopes heterologous to that fHBP amino acid sequence).
- the distance between epitopes of such epitope pairs is selected so as to be less than 27 ⁇ but more than 14 ⁇ , and are usually located within a distance of about 18 ⁇ - 20 ⁇ .
- a greater bactericidal effect was observed when two antibodies bound epitopes located at distances within these parameters.
- the distance between the epitopes is sufficient to facilitate interaction of the antibodies with factors of the complement cascade, but not so close as to result in inhibition of binding due to steric hindrance.
- Chimeric fHBP containing such epitopes for v.2 and v.3 strains can thus provide for production of antibodies having greater bactericidal activity against such strains.
- epitope pairs are those epitopes bound by JAR 10 and JAR 11 (fHBP v.2); and by JAR 33 and JAR 32/ 35 (JAR 32 and JAR 35 bind to the same or overlapping epitopes) (fHBP v.3).
- Chimeric fHBPs can also include epitope pairs where one epitope of the pair is defined by binding by the mAb JAR 4 and the second epitope is bound by an antibody that inhibits fH binding.
- Such an epitope pair is not necessarily subject to the constraints on distance between the epitopes as discussed above, with the proviso that the epitopes are not so close as to inhibit binding of their respective antibodies.
- binding of an antibody that inhibits fH binding can be bactericidal along with another mAb that does not inhibit fH binding.
- a mAb pair such as JAR 4 along with any anti-v.1 or v.2 mAb that blocks fH binding can provide for production of antibodies that have enhanced bactericidal activity.
- Chimeric fHBPs can be designed so as to include an epitope(s) that elicits antibodies that, when bound to fHBP, inhibit fH binding.
- an epitope(s) that elicits antibodies that, when bound to fHBP, inhibit fH binding.
- JAR 13 v.2 epitope
- JAR 11 v.2 epitope
- JAR 32/35 v.3 epitope
- the chimeric fHBP can be generated using recombinant techniques to manipulate nucleic acids of different fHBPs known in the art to provide constructs encoding a chimeric fHBP of interest.
- nucleic acids encoding a variety of different v.1, v.2, and v.3 fHBPs of N. meningitidis are available in the art, and their nucleotide sequences are known.
- Amino acid and nucleic acid sequences of exemplary chimeric fHBPs are provided in Figures 23-28 . It will be appreciated that the nucleotide sequences encoding the chimeric fHBPs can be modified so as to optimize the codon usage to facilitate expression in a host cell of interest (e.g., E. coli, N. meningitidis, human (as in the case of a DNA-based vaccine), and the like). Methods for production of codon optimized sequences are known in the art.
- Chimeric fHBPs can be produced by any suitable method, including recombinant and non-recombinant methods (e.g., chemical synthesis). Where the chimeric fHBP is produced using recombinant techniques, the methods can involve any suitable construct and any suitable host cell, which can be a prokaryotic or eukaryotic cell, usually a bacterial or yeast host cell, more usually a bacterial cell. Methods for introduction of genetic material into host cells include, for example, transformation, electroporation, conjugation, calcium phosphate methods and the like. The method for transfer can be selected so as to provide for stable expression of the introduced chimeric fHBP -encoding nucleic acid.
- the chimeric fHBP -encoding nucleic acid can be provided as an inheritable episomal element (e.g., plasmid) or can be genomically integrated.
- Suitable vectors for transferring chimeric fHBP-encoding nucleic acid can vary in composition.
- Integrative vectors can be conditionally replicative or suicide plasmids, bacteriophages, and the like.
- the constructs can include various elements, including for example, promoters, selectable genetic markers (e.g., genes conferring resistance to antibiotics (for instance kanamycin, erythromycin, chloramphenicol, or gentamycin)), origin of replication (to promote replication in a host cell, e.g., a bacterial host cell), and the like.
- selectable genetic markers e.g., genes conferring resistance to antibiotics (for instance kanamycin, erythromycin, chloramphenicol, or gentamycin)
- origin of replication to promote replication in a host cell, e.g., a bacterial host cell
- the choice of vector will depend upon a variety of factors such as the type of cell in which propagation is desired and the purpose of propagation.
- vectors are useful for amplifying and making large amounts of the desired DNA sequence.
- Other vectors are suitable for expression in cells in culture.
- Still other vectors are suitable for transfer and expression in cells in a whole animal.
- the choice of appropriate vector is well within the skill of the art. Many such vectors are available commercially.
- the vector is an expression vector based on episomal plasmids containing selectable drug resistance markers and elements that provide for autonomous replication in different host cells (e.g., in both E. coli and N. meningitidis ) .
- episomal plasmids containing selectable drug resistance markers and elements that provide for autonomous replication in different host cells (e.g., in both E. coli and N. meningitidis ) .
- a "shuttle vector” is the plasmid pFP10 ( Pagotto et al. Gene 2000 244:13-19 ).
- Constructs can be prepared by, for example, inserting a polynucleotide of interest into a construct backbone, typically by means of DNA ligase attachment to a cleaved restriction enzyme site in the vector.
- the desired nucleotide sequence can be inserted by homologous recombination or site-specific recombination.
- homologous recombination is accomplished by attaching regions of homology to the vector on the flanks of the desired nucleotide sequence, while site-specific recombination can be accomplished through use of sequences that facilitate site-specific recombination (e.g., cre-lox, att sites, etc.).
- Nucleic acid containing such sequences can be added by, for example, ligation of oligonucleotides, or by polymerase chain reaction using primers comprising both the region of homology and a portion of the desired nucleotide sequence.
- Vectors can provide for extrachromosomal maintenance in a host cell or can provide for integration into the host cell genome. Vectors are amply described in numerous publications well known to those in the art, including, e.g., Short Protocols in Molecular Biology, (1999) F. Ausubel, et al., eds., Wiley & Sons . Vectors may provide for expression of the nucleic acids encoding a chimeric fHBP, may provide for propagating the subject nucleic acids, or both.
- Exemplary vectors that may be used include but are not limited to those derived from recombinant bacteriophage DNA, plasmid DNA or cosmid DNA.
- plasmid vectors such as pBR322, pUC 19/18, pUC 118, 119 and the M13 mp series of vectors may be used.
- pET21 is also an expression vector that may be used.
- Bacteriophage vectors may include ⁇ gt10, ⁇ gt11, ⁇ gt18-23, ⁇ ZAP/R and the EMBL series of bacteriophage vectors.
- vectors that may be utilized include, but are not limited to, pJB8, pCV 103, pCV 107, pCV 108, pTM, pMCS, pNNL, pHSG274, COS202, COS203, pWE15, pWE16 and the charomid 9 series of vectors.
- an expression cassette may be employed for expression of a chimeric fHBP of interest.
- the expression vector provides transcriptional and translational regulatory sequences, and may provide for inducible or constitutive expression, where the coding region is operably linked under the transcriptional control of the transcriptional initiation region, and a transcriptional and translational termination region. These control regions may be native to an fHBP from which the chimeric fHBP is derived, or may be derived from exogenous sources.
- transcriptional and translational regulatory sequences may include, but are not limited to, promoter sequences, ribosomal binding sites, transcriptional start and stop sequences, translational start and stop sequences, and enhancer or activator sequences.
- Promoters can be either constitutive or inducible, and can be a strong constitutive promoter (e.g., T7, and the like).
- Expression vectors generally have convenient restriction sites located near the promoter sequence to provide for the insertion of nucleic acid sequences encoding proteins of interest.
- a selectable marker operative in the expression host may be present to facilitate selection of cells containing the vector.
- the expression construct may include additional elements.
- the expression vector may have one or two replication systems, thus allowing it to be maintained in organisms, for example in mammalian or insect cells for expression and in a procaryotic host for cloning and amplification.
- the expression construct may contain a selectable marker gene to allow the selection of transformed host cells. Selection genes are well known in the art and will vary with the host cell used.
- chimeric fHBP of the present disclosure may comprise additional elements, such as a detectable label, e.g., a radioactive label, a fluorescent label, a biotin label, an immunologically detectable label (e.g., an HA tag, a poly-Histidine tag) and the like. Additional elements of chimeric fHBP can be provided to facilitate isolation (e.g., biotin tag, immunologically detectable tag) through various methods (e.g., affinity capture, etc.). Chimeric fHBP can optionally be immobilized on a support through covalent or noncovalent attachment.
- a detectable label e.g., a radioactive label, a fluorescent label, a biotin label, an immunologically detectable label (e.g., an HA tag, a poly-Histidine tag) and the like.
- Additional elements of chimeric fHBP can be provided to facilitate isolation (e.g., biotin tag, immunologically detectable tag) through various
- chimeric fHBP can be isolated from a lysate of cells genetically modified to express a chimeric fHBP, or from a synthetic reaction mix, by immunoaffinity purification, which generally involves contacting the sample with an anti-chimeric fHBP antibody (e.g., an anti-chimeric fHBP mAb, such as a JAR 5 mAb or other appropriate JAR mAb described herein), washing to remove non-specifically bound material, and eluting specifically bound chimeric fHBP.
- Isolated chimeric fHBP can be further purified by dialysis and other methods normally employed in protein purification methods.
- the chimeric fHBP can be isolated using metal chelate chromatography methods.
- chimeric fHBP Any of a number of suitable host cells can be used in the production of chimeric fHBP.
- the chimeric fHBP described herein may be expressed in prokaryotes or eukaryotes, usually bacteria, more usually E. coli or Neisseria (e.g., N. meningitidis) in accordance with conventional techniques.
- the present disclosure further provides a genetically modified host cell, which contains a nucleic acid encoding a chimeric fHBP.
- Host cells for production (including large scale production) of a chimeric fHBP can be selected from any of a variety of available host cells.
- Exemplary host cells for expression include those of a prokaryotic or eukaryotic unicellular organism, such as bacteria (e.g., Escherichia coli strains), yeast (e.g., S. cerevisiae, Pichia spp., and the like)., and may include host cells originally derived from a higher organism such as insects, vertebrates, particularly mammals, (e.g. CHO, HEK, and the like). Generally bacterial host cells and yeast are of particular interest for chimeric fHBP production.
- bacteria e.g., Escherichia coli strains
- yeast e.g., S. cerevisiae, Pichia spp., and the like
- host cells originally derived from a higher organism such as insects, vertebrates, particularly mammals, (e.g. CHO, HEK, and the like).
- Generally bacterial host cells and yeast are of particular interest for chimeric fHBP production.
- Chimeric fHBPs can be prepared in substantially pure or substantially isolated form (i.e., substantially free from other Neisserial or host cell polypeptides) or substantially isolated form.
- the chimeric fHBP is present in a composition that is enriched for the polypeptide relative to other components that may be present (e.g., other polypeptides or other host cell components).
- Purified chimeric fHBP can be provided such that the polypeptide is present in a composition that is substantially free of other expressed polypeptides, e.g., less than 90%, usually less than 60% and more usually less than 50% of the composition is made up of other expressed polypeptides.
- a Neisserial host cell is genetically modified to express a chimeric fHBP.
- Any of a variety of Neisseria spp. strains can be modified to produce a chimeric fHBP, and, optionally, which produce or can be modified to produce other antigens of interest, such as PorA, can be used in the methods disclosed herein.
- exemplary vectors and methods are provided in WO 02/09746 and O'Dwyer et al. Infect Immun 2004;72:6511-80 .
- Strong promoters, particularly constitutive strong promoters are of particular interest.
- Exemplary promoters include the promoters of porA, porB, lbpB, tbpB, p110, hpuAB, lgtF, opa, p110, lst, hpuAB. and rmp.
- Pathogenic Neisseria spp. or strains derived from pathogenic Neisseria spp., particularly strains pathogenic for humans or derived from strains pathogenic or commensal for humans, are of particular interest for use in membrane vesicle production.
- Exemplary Neisserial spp. include N. meningitidis, N. flavescens, N. gonorrhoeae, N. lactamica, N. polysaccharea, N. cinerea, N. mucosa, N. subflava, N. sicca, N. elongata, and the like.
- N. meningitidis strains are of particular interest for genetic modification to express a chimeric fHBP and for use in vesicle production.
- the strain used for vesicle production can be selected according to a number of different characteristics that may be desired.
- the strain may be selected according to: a desired PorA type (a "serosubtype", as described above), capsular group, serotype, and the like; decreased capsular polysaccharide production; and the like.
- the production strain can produce any desired PorA polypeptide, and may express one or more PorA polypeptides (either naturally or due to genetic engineering).
- Exemplary strains includes those that produce a PorA polypeptide which confers a serosubtype of P1.7,16; P1.19,15; P1.7,1; P1.5,2; P1.22a,14; P1.14; P1.5,10; P1.7,4; P1.12,13; as well as variants of such PorA polypeptides which may or may not retain reactivity with conventional serologic reagents used in serosubtyping. Also of interest are PorA polypeptides characterized according to PorA variable region (VR) typing (see, e.g., Russell et al.
- VR PorA variable region
- the production strain can be a capsule deficient strain.
- Capsule deficient strains can provide vesicle-based vaccines that provide for a reduced risk of eliciting a significant autoantibody response in a subject to whom the vaccine is administered (e.g., due to production of antibodies that cross-react with sialic acid on host cell surfaces).
- "Capsule deficient” or “deficient in capsular polysaccharide” as used herein refers to a level of capsular polysaccharide on the bacterial surface that is lower than that of a naturally-occurring strain or, where the strain is genetically modified, is lower than that of a parental strain from which the capsule deficient strain is derived.
- a capsule deficient strain includes strains that are decreased in surface capsular polysaccharide production by at least 10%, 20%, 25%, 30%, 40%, 50%, 60%, 75%, 80%, 85%, 90% or more, and includes strains in which capsular polysaccharide is not detectable on the bacterial surface (e.g., by whole cell ELISA using an anti-capsular polysaccharide antibody).
- Capsule deficient strains include those that are capsule deficient due to a naturally-occurring or recombinantly-generated genetic modification.
- Naturally-occurring capsule deficient strains see, e.g., Dolan-Livengood et al. J. Infect. Dis. (2003) 187(10):1616-28 ), as well as methods of identifying and/or generating capsule-deficient strains (see, e.g., Fisseha et al. (2005) Infect. Immun. 73(7):4070-4080 ; Stephens et al. (1991) Infect Immun 59(11):4097-102 ; Frosch et al. (1990) Mol Microbiol. 1990 4(7):1215-1218 ) are known in the art.
- Modification of a Neisserial host cell to provide for decreased production of capsular polysaccharide may include modification of one or more genes involved in capsule synthesis, where the modification provides for, for example, decreased levels of capsular polysaccharide relative to a parent cell prior to modification.
- Such genetic modifications can include changes in nucleotide and/or amino acid sequences in one or more capsule biosynthesis genes rendering the strain capsule deficient (e.g., due to one or more insertions, deletions, substitutions, and the like in one or more capsule biosynthesis genes).
- Capsule deficient strains can lack or be non-functional for one or more capsule genes.
- strains that are deficient in sialic acid biosynthesis can provide for production of vesicles that have reduced risk of eliciting anti-sialic acid antibodies that cross-react with human sialic acid antigens, and can further provide for improved manufacturing safety.
- Strains having a defect in sialic acid biosynthesis can be defective in any of a number of different genes in the sialic acid biosynthetic pathway.
- strains that are defective in a gene product encoded by the N-acetylglucosamine-6-phosphate 2-epimerase gene (known as synX AAF40537.1 or siaA AAA20475), with strains having this gene inactivated being of especial interest.
- a capsule deficient strain is generated by disrupting production of a functional synX gene product (see, e.g., Swartley et al. (1994) J Bacteriol. 176(5):1530-4 ).
- Capsule-deficient strains can also be generated from naturally-occurring strains using non-recombinant techniques, e.g., by use of bactericidal anti-capsular antibodies to select for strains that reduced in capsular polysaccharide.
- the strains can be selected so as to differ in one or more strain characteristics, e.g., to provide for vesicles that differ in the chimeric fHBP used, PorA, and the like.
- the antigenic compositions contemplated by the present disclosure generally include vesicles prepared from Neisserial cells that express a chimeric fHBP.
- vesicles is meant to encompass outer membrane vesicles as well as microvesicles (which are also referred to as blebs).
- the antigenic composition comprises outer membrane vesicles (OMV) prepared from the outer membrane of a cultured strain of Neisseria meningitidis spp. genetically modified to express a chimeric fHBP.
- OMVs may be obtained from Neisseria meningitidis grown in broth or solid medium culture, preferably by separating the bacterial cells from the culture medium (e.g. by filtration or by a low-speed centrifugation that pellets the cells, or the like), lysing the cells (e.g. by addition of detergent, osmotic shock, sonication, cavitation, homogenization, or the like) and separating an outer membrane fraction from cytoplasmic molecules (e.g.
- outer membrane fractions may be used to produce OMVs.
- the antigenic composition comprises microvesicles (MV) (or "blebs") containing chimeric fHBP, where the MV or blebs are released during culture of a Neisseria meningitidis strain genetically modified to express a chimeric fHBP.
- MVs may be obtained by culturing a strain of Neisseria meningitidis in broth culture medium, separating whole cells from the broth culture medium (e.g. by filtration, or by a low-speed centrifugation that pellets only the cells and not the smaller blebs, or the like), and then collecting the MVs that are present in the cell-free culture medium (e.g.
- Strains for use in production of MVs can generally be selected on the basis of the amount of blebs produced in culture (e.g., bacteria can be cultured in a reasonable number to provide for production of blebs suitable for isolation and administration in the methods described herein).
- An exemplary strain that produces high levels of blebs is described in PCT Publication No. WO 01/34642 .
- strains for use in MV production may also be selected on the basis of NspA production, where strains that produce higher levels of NspA may be of particular interest (for examples of N.
- meningitidis strains having different NspA production levels see, e.g., Moe et al. (1999 Infect. Immun. 67: 5664 ).
- Other strains of interest for use in production of blebs include strains having an inactivated GN33 gene, which encodes a lipoprotein required for cell separation, membrane architecture and virulence (see, e.g., Adu-Bobie et al. Infect Immun. 2004;72:1914-1919 ).
- the antigenic compositions of the present disclosure can comprise vesicles from one strain, or from 2, 3, 4, 5 or more strains, which strains may be homologous or heterologous, usually heterologous, to one another.
- the strains may be homologous or heterologous with respect to PorA.
- the vesicles can be prepared from strains that express more than one chimeric fHBP (e.g., 1, 2, 3, or more chimeric fHBP) which may be composed of fHBP amino acid sequences from different variants (v.1, v.2, or v.3) or subvariants (e.g., a subvariant of v.1, v.2, or v.3).
- the antigenic compositions can comprise a mixture of OMVs and MVs presenting the same or different chimeric fHBPs, where the chimeric fHBPs may optionally present epitopes from different combinations of fHBP variants and/or subvariants and where the OMVs and/or MVs may be from the same or different strains.
- Vesicles from different strains can be administered as a mixture, or can be administered serially.
- the vesicles are optionally treated to reduce endotoxin, e.g., to reduce toxicity following administration.
- reduction of endotoxin can be accomplished by extraction with a suitable detergent (for example, BRIJ-96, sodium deoxycholate, sodium lauroylsarcosinate, Empigen BB, Triton X-100, TWEEN 20 (sorbitan monolaurate polyoxyethylene), TWEEN 80, at a concentration of 0.1-10%, preferably 0.5-2%, and SDS).
- a suitable detergent for example, BRIJ-96, sodium deoxycholate, sodium lauroylsarcosinate, Empigen BB, Triton X-100, TWEEN 20 (sorbitan monolaurate polyoxyethylene), TWEEN 80, at a concentration of 0.1-10%, preferably 0.5-2%, and SDS.
- a detergent other than deoxycholate it is preferable to use a detergent other than deoxycholate.
- the vesicles of the antigenic compositions are prepared without detergent, e.g., without use of deoxycholate.
- detergent treatment is useful to remove endotoxin activity, it may deplete the native fHBP lipoprotein and/or chimeric fHBP (including lipidated chimeric fHBP) by extraction during vesicle production. Thus it may be particularly desirable to decrease endotoxin activity using technology that does not require a detergent.
- strains that are relatively low producers of endotoxin lipopolysaccharide, LPS
- the vesicles can be prepared from Neisseria mutants in which lipooligosaccharide or other antigens that may be undesirable in a vaccine (e.g. Rmp) is reduced or eliminated.
- Vesicles can be prepared from N. meningitidis strains that contain genetic modifications that result in decreased or no detectable toxic activity of lipid A.
- such strain can be genetically modified in lipid A biosynthesis ( Steeghs et al. Infect Immun 1999;67:4988-93 ; van der Ley et al. Infect Immun 2001;69:5981-90 ; Steeghs et al. J Endotoxin Res 2004;10:113-9 ; Fissha et al, Infect Immun 73:4070,.2005 ).
- the immunogenic compositions may be detoxified by modification of LPS, such as downregulation and/or inactivation of the enzymes encoded by lpxL1 or lpxL2, respectively.
- LPS low-power polypeptide
- Production of a penta-acylated lipid A made in lpxL1 mutants indicates that the enzyme encoded by lpxL1 adds the C12 to the N-linked 3-OH C14 at the 2' position of GlcN II.
- the major lipid A species found in lpxL2 mutants is tetra-acylated, indicating the enzyme encoded by lpxL2 adds the other C12, i.e., to the N-linked 3-OH C14 at the 2 position of GlcN I.
- meningitidis strains genetically modified so as to provide for decreased or no detectable functional LpxL1-encoded protein.
- Such vesicles provide for reduced toxicity as compared to N. meningitidis strains that are wild-type for LPS production, while retaining immunogenicity of chimeric fHBP.
- LPS toxic activity can also be altered by introducing mutations in genes/loci involved in polymyxin B resistance (such resistance has been correlated with addition of aminoarabinose on the 4' phosphate of lipid A).
- genes/loci could be pmrE that encodes a UDP-glucose dehydrogenase, or a region of antimicrobial peptide-resistance genes common to many enterobacteriaciae which could be involved in aminoarabinose synthesis and transfer.
- the gene pmrF that is present in this region encodes a dolicol-phosphate manosyl transferase ( Gunn J. S., Kheng, B. L., Krueger J., Kim K., Guo L., hackett M., Miller S. I. 1998. Mol. Microbiol. 27: 1171-1182 ).
- PhoP-PhoQ regulatory system which is a phospho-relay two component regulatory system (e.g., PhoP constitutive phenotype, PhoPc), or low Mg++ environmental or culture conditions (that activate the PhoP-PhoQ regulatory system) lead to the addition of aminoarabinose on the 4'-phosphate and 2-hydroxymyristate replacing myristate (hydroxylation of myristate).
- This modified lipid A displays reduced ability to stimulate E-selectin expression by human endothelial cells and TNF secretion from human monocytes.
- Polymyxin B resistant strains are also suitable for use, as such strains have been shown to have reduced LPS toxicity (see, e.g., van der Ley et al. 1994. In: Proceedings of the ninth international pathogenic Neisseria conference. The Guildhall, Winchester, England).
- synthetic peptides that mimic the binding activity of polymyxin B may be added to the antigenic compositions to reduce LPS toxic activity (see, e.g., Rustici et al. 1993, Science 259:361-365 ; Porro et al. Prog Clin Biol Res. 1998;397:315-25 ).
- Endotoxin can also be reduced through selection of culture conditions. For example, culturing the strain in a growth medium containing 0.1 mg-100 mg of aminoarabinose per liter medium provides for reduced lipid toxicity (see, e.g., WO 02/097646 ).
- Antigen composition is used herein as a matter of convenience to refer generically to compositions comprising a chimeric fHBP as disclosed herein, which chimeric fHBP may be optionally conjugated to further enhance immunogenicity.
- Compositions useful for eliciting antibodies, particularly antibodies against Neisseria meningitidis group B (NmB), in a human are specifically contemplated by the present disclosure.
- Antigenic compositions can contain 2 or more different chimeric fHBPs, where the chimeric fHBPs may present epitopes from different combinations of fHBP variants and/or subvariants.
- Antigenic compositions generally comprise an immunologically effective amount of chimeric fHBP, and may further include other compatible components, as needed.
- immunologically effective amount is meant that the administration of that amount to an individual, either in a single dose, as part of a series of the same or different antigenic compositions, is effective to elicit an antibody response effective for treatment or prevention of a symptom of, or disease caused by, for example, infection by Neisseria, particularly N. meningitidis, more particularly Group B N. meningitidis.
- This amount varies depending upon the health and physical condition of the individual to be treated, age, the capacity of the individual's immune system to produce antibodies, the degree of protection desired, the formulation of the vaccine, the treating clinician's assessment of the medical situation, and other relevant factors. It is expected that the amount will fall in a relatively broad range that can be determined through routine trials.
- Dosage regimen may be a single dose schedule or a multiple dose schedule (e.g., including booster doses) with a unit dosage form of the antigenic composition administered at different times.
- unit dosage form refers to physically discrete units suitable as unitary dosages for human and animal subjects, each unit containing a predetermined quantity of the antigenic compositions of the present invention in an amount sufficient to produce the desired effect, which compositions are provided in association with a pharmaceutically acceptable excipient (e.g., pharmaceutically acceptable diluent, carrier or vehicle).
- the antigenic composition may be administered in conjunction with other immunoregulatory agents.
- Antigenic compositions can be provided in a pharmaceutically acceptable excipient, which can be a solution such as a sterile aqueous solution, often a saline solution, or they can be provided in powder form. Such excipients can be substantially inert, if desired.
- the antigenic compositions can further comprise an adjuvant.
- suitable adjuvants that can be used in humans include, but are not necessarily limited to, alum, aluminum phosphate, aluminum hydroxide, MF59 (4.3% w/v squalene, 0.5% w/v Tween 80TM, 0.5% w/v Span 85), CpG-containing nucleic acid (where the cytosine is unmethylated), QS21, MPL, 3DMPL, extracts from Aquilla, ISCOMS, LT/CT mutants, poly(D,L-lactide-co-glycolide) (PLG) microparticles, Quil A, interleukins, and the like.
- thr-MDP N-acetyl-muramyl-L-threonyl-D-isoglutamine
- CGP 11637 N-acetyl-nor-muramyl-L-alanyl-D-isoglutamine
- nor-MDP N-acetylmuramyl-L-alanyl-D-isoglutaminyl-L-alanine-2-(1'-2'-dip- almitoyl-sn-glycero-3-hydroxyphosphoryloxy)-ethylamine
- CGP 19835A referred to as MTP-PE
- RIBI which contains three components extracted from bacteria, monophosphoryl lipid A, trehalose dimycolate and cell wall skeleton (MPL+TDM+CWS) in a 2% squalene/Tween 80 emulsion.
- the effectiveness of an adjuvant may be determined by measuring the amount of antibodies directed against
- adjuvants to enhance effectiveness of the composition include, but are not limited to: (1) oil-in-water emulsion formulations (with or without other specific immunostimulating agents such as muramyl peptides (see below) or bacterial cell wall components), such as for example (a) MF59TM ( WO 90/14837 ; Chapter 10 in Vaccine design: the subunit and adjuvant approach, eds.
- Span 85 (optionally containing MTP-PE) formulated into submicron particles using a microfluidizer, (b) SAF, containing 10% Squalane, 0.4% Tween 80, 5% pluronic-blocked polymer L121, and thr-MDP either microfluidized into a submicron emulsion or vortexed to generate a larger particle size emulsion, and (c) RIBITM adjuvant system (RAS), (Ribi Immunochem, Hamilton, Mont.) containing 2% Squalene, 0.2% Tween 80, and one or more bacterial cell wall components such as monophosphorylipid A (MPL), trehalose dimycolate (TDM), and cell wall skeleton (CWS), preferably MPL+CWS (Detox TM); (2) saponin adjuvants, such as QS21 or Stimulon TM(
- RAS RIBITM adjuvant system
- MPL monophosphorylipid A
- TDM trehalose dim
- interferons e.g. gamma interferon
- M-CSF macrophage colony stimulating factor
- TNF tumor necrosis factor
- MPL monophosphoryl lipid A
- 3dMPL 3-O-deacylated MPL
- WO 00/56358 combinations of 3dMPL with, for example, QS21 and/or oil-in-water emulsions e.g. EP-A-0835318 , EP-A-0735898 , EP-A-0761231 ; (7) oligonucleotides comprising CpG motifs ( Krieg Vaccine 2000, 19, 618-622 ; Krieg Curr opin Mol Ther2001 3:15-24 ; Roman et al., Nat. Med, 1997, 3, 849-854 ; Weiner et al., PNAS USA, 1997, 94, 10833-10837 ; Davis et al, J.
- a polyoxyethylene ether or a polyoxyethylene ester e.g WO 99/52549
- a polyoxyethylene sorbitan ester surfactant in combination with an octoxynol WO 01/21207
- a polyoxyethylene alkyl ether or ester surfactant in combination with at least one additional non-ionic surfactant such as an octoxynol ( WO 01/21152 );
- a saponin and an immunostimulatory oligonucleotide e.g.
- a CpG oligonucleotide ( WO 00/62800 ); (11) an immunostimulant and a particle of metal salt e.g WO 00/23105 ; (12) a saponin and an oil-in-water emulsion e.g. WO 99/11241 ; (13) a saponin (e.g QS21)+3dMPL+IM2 (optionally+a sterol) e.g WO 98/57659 ; (14) other substances that act as immunostimulating agents to enhance the efficacy of the composition.
- Muramyl peptides include N-acetyl-muramyl-L-threonyl-D-isoglutamine (thr-MDP), N-25 acetyl-normuramyl-L-alanyl-D-isoglutamine (nor-MDP), N-acetylmuramyl-L-alanyl-D-isoglutarninyl-L-alanine-2-(1'-2'-dipalmitoyl-- sn-glycero-3-hydroxyphosphoryloxy)-ethylamine MTP-PE), etc.
- Adjuvants suitable for administration to a human are of particular interest.
- the antigen compositions may comprise other components, such as pharmaceutical grades of mannitol, lactose, starch, magnesium stearate, sodium saccharin, talcum, cellulose, glucose, sucrose, magnesium, carbonate, and the like.
- the compositions may contain pharmaceutically acceptable auxiliary substances as required to approximate physiological conditions such as pH adjusting and buffering agents, toxicity adjusting agents and the like, for example, sodium acetate, sodium chloride, potassium chloride, calcium chloride, sodium lactate and the like.
- the concentration of chimeric fHBP in a formulation can vary widely (e.g., from less than about 0.1%, usually at or at least about 2% to as much as 20% to 50% or more by weight) and will usually be selected primarily based on fluid volumes, viscosities, and patient-based factors in accordance with the particular mode of administration selected and the patient's needs.
- Chimeric fHBP-containing formulations can be provided in the form of a solution, suspension, tablet, pill, capsule, powder, gel, cream, lotion, ointment, aerosol or the like. It is recognized that oral administration can require protection of the compositions from digestion. This is typically accomplished either by association of the composition with an agent that renders it resistant to acidic and enzymatic hydrolysis or by packaging the composition in an appropriately resistant carrier. Means of protecting from digestion are well known in the art.
- Chimeric fHBP-containing formulations can also provided so as to enhance serum half-life of chimeric fHBP following administration.
- the chimeric fHBP may be provided in a liposome formulation, prepared as a colloid, or other conventional techniques for extending serum half-life.
- a variety of methods are available for preparing liposomes, as described in, e.g., Szoka et al., Ann. Rev. Biophys. Bioeng. 9:467 (1980 ), U.S. Pat. Nos. 4,235,871 , 4,501,728 and 4,837,028 .
- the preparations may also be provided in controlled release or slow-release forms.
- the chimeric fHBP-containing antigenic compositions are generally administered to a human subject that is at risk of acquiring a Neisserial disease so as to prevent or at least partially arrest the development of disease and its complications.
- An amount adequate to accomplish this is defined as a "therapeutically effective dose.” Amounts effective for therapeutic use will depend on, e.g., the antigenic composition, the manner of administration, the weight and general state of health of the patient, and the judgment of the prescribing physician.
- Single or multiple doses of the antigenic compositions may be administered depending on the dosage and frequency required and tolerated by the patient, and route of administration.
- the chimeric fHBP-containing antigenic compositions are generally administered in an amount effective to elicit an immune response, particularly a humoral immune response, in the host.
- amounts for immunization will vary, and can generally range from about 1 ⁇ g to 100 ⁇ g per 70 kg patient, usually 5 ⁇ g to 50 ⁇ g/70 kg.
- Substantially higher dosages e.g. 10 mg to 100 mg or more
- the initial administration can be followed by booster immunization of the same of different chimeric fHBP-containing antigenic composition.
- vaccination involves at least one booster, more usually two boosters.
- immunization can be accomplished by administration by any suitable route, including administration of the composition orally, nasally, nasopharyngeally, parenterally, enterically, gastrically, topically, transdermally, subcutaneously, intramuscularly, in tablet, solid, powdered, liquid, aerosol form, locally or systemically, with or without added excipients.
- parenterally administrable compositions will be known or apparent to those skilled in the art and are described in more detail in such publications as Remington's Pharmaceutical Science, 15th ed., Mack Publishing Company, Easton, Pa. (1980 ).
- An anti-chimeric fHBP immune response can be assessed by known methods (e.g. by obtaining serum from the individual before and after the initial immunization, and demonstrating a change in the individual's immune status, for example an immunoprecipitation assay, or an ELISA, or a bactericidal assay, or a Western blot, or flow cytometric assay, or the like).
- known methods e.g. by obtaining serum from the individual before and after the initial immunization, and demonstrating a change in the individual's immune status, for example an immunoprecipitation assay, or an ELISA, or a bactericidal assay, or a Western blot, or flow cytometric assay, or the like).
- the antigenic compositions can be administered to a human subject that is immunologically naive with respect to Neisseria meningitidis.
- the subject is a human child about five years or younger, and preferably about two years old or younger, and the antigenic compositions are administered at any one or more of the following times: two weeks, one month, 2, 3, 4, 5, 6, 7, 8, 9, 10, or 11 months, or one year or 15, 18, or 21 months after birth, or at 2, 3, 4, or 5 years of age.
- Wild-type fHBP genes were amplified from genomic DNA by PCR and cloned into pGEM-T-Easy (Promega). The resulting plasmids were treated with the restriction enzymes Nde I and Xho I and the approximately 800 base-pair fragments containing the fHBP coding sequences were ligated into pET21b (Novagen) cut with the same two enzymes. The plasmid clones were confirmed by DNA sequence determination of PCR products obtained by the amplification of the plasmid with primers specific for the T7 promotor and terminator regions.
- the plasmids encoded the full-length fHBP proteins except for the amino-terminal 19 amino acid signal sequence and 7 presumably flexible N-terminal residues, and included a C-terminal hexa-histidine (His 6 ) tag originating from the pET21b plasmid.
- fHBP Chimera I lacking a signal sequence was constructed by PCR amplification of the region encoding residues 8-135 from genomic DNA from strain MC58 (fHBP v.1) and that encoding residues 136-255 from strain 8047 (v.2).
- the two fragments, including an overlapping region of 48 base pairs centered around amino acids 136-139, were assembled by PCR amplification using external, gene-specific primers containing the Nde I and Xho I restriction sites.
- the chimeric gene was cloned into pET21b as described for wild-type genes above.
- Site-specific mutagenesis was used to test predictions of amino acid residues involved in anti-fHBP mAb epitopes and to create Chimera II. Mutagenesis was performed using the QuikChange II kit (Stratagene) using 10 ng of plasmid template and the manufacturer's protocols. For testing residues putatively involved in mAb epitopes, mutagenesis reactions were performed on pET21-based plasmids encoding wild-type fHBP genes from various strains. A residue in a reactive sequence was changed to that naturally present in a non-reactive sequence or vice versa.
- Chimera II site-specific mutagenesis was used to introduce the A174K substitution into the pET21 plasmid encoding Chimera I. Mutant fHBP genes were confirmed by DNA sequencing as described for the wild-type plasmids, above.
- fHBP expression and purification Wild-type, mutant and chimeric fHBPs were expressed in Escherichia coli BL21(DE3) (Novagen). fHBP purifications were performed from 1 L cultures. Mid-exponential cultures (optical density at 600 nm of 0.5-0.6) were grown at 37 °C, induced with 0.5 mM isopropylthiogalactoside for 3-4 h and the bacteria harvested by centrifugation. The cells were lysed by incubation with chicken egg white lysozyme (Sigma) and two freeze/thaw cycles.
- Bacterial lysates were treated with DNase and RNase (Sigma) and protease inhibitors (Complete EDTA-free, Roche) and clarified by centrifugation at 13,000 x g.
- Recombinant fHBPs were purified by nickel chelate chromatography using Ni-NTA agarose (Qiagen) and buffers recommended by the supplier. Fractions containing purified fHBP were pooled and dialyzed against PBS (Roche) containing 5% (w/v) sucrose and 0.01% NaN 3 , filter sterilized and stored at 4 °C.
- mAb preparation We generated hybridoma cell lines from spleens from CD-1 mice immunized with recombinant fHBP variant group 2 (gene from strain 2996) or variant group 3 (gene from strain M1239) using methods previously described for preparation of hybridoma cell lines secreting mAbs against fHBP v.1 protein ( Welsch et al., J. Immunol. 2004 ). mAbs were precipitated from tissue culture supernatants with 50% saturated (NH 4 ) 2 SO 4 and dialyzed against phosphate-buffered saline (PBS; Roche). IgG isotypes were determined using Clonotyping-AP reagents (Southern Biotech).
- Binding of the mAbs to recombinant fHBP was measured by ELISA.
- the wells of a microtiter plate (Immulon 2B; Thermo Electron Corp.) were coated with 1 ⁇ g/ml of recombinant fHBP in PBS and incubated overnight at 4 °C.
- the plates were blocked with PBS containing 0.1% Tween-20 (Sigma) (PBST) and 1% BSA (Sigma).
- the primary antibodies were anti-fHBP mAbs (0.016 to 5 ⁇ g/ml) and the secondary antibody was rabbit anti-mouse IgG-alkaline phosphatase (Zymed; 1:5,000), each diluted in PBST. After 1 h at room temperature, alkaline phosphatase substrate (Sigma) was added and the absorbance at 405 nm was measured after 30 min.
- one mAb was held at a fixed concentration sufficient to obtain an OD at 405 nm of 1.0 determined by direct binding ELISA, as described above.
- a second mAb of a different isotype was added together with the first mAb to the wells of a microtiter plate coated with the antigen as described above, at concentrations ranging from 0.4 to 50 ⁇ g/ml.
- the secondary mAb was an isotype specific mouse anti-IgG-alkaline phosphatase conjugate.
- the ELISA was developed as described above.
- the membranes were washed, incubated with the different anti-fHBP mAbs (1 to 5 ⁇ g/ml) or, as a control for protein expression by the different clones, 0.02 ⁇ g/ml of Penta-His mAb (Qiagen).
- the membranes were washed in PBST and incubated with a 1:10,000 dilution of a rabbit anti-mouse IgG-horseradish peroxidase conjugate (Zymed) and washed again.
- the membranes were developed with a chemiluminescent substrate (ECL + ; GE Healthcare) and visualized on a Storm 840 imager (Molecular Dynamics).
- mice mice each of five-week old CD-1 mice (Charles River) were immunized with four doses containing 20 ⁇ g of wild-type or chimeric fHBP vaccines or adjuvant alone at two-week intervals.
- Each experimental or control vaccine was administered with aluminum hydroxide or Freund's adjuvant (FA) (complete FA for the first dose and incomplete FA for subsequent doses).
- FA Freund's adjuvant
- Complement-mediated bactericidal activity was measured as described previously using washed, log-phase bacteria grown in Mueller-Hinton broth supplemented with 0.25 % glucose and 0.02 mM CMP-NANA to an OD 620 of 0.6.
- the buffer was Dulbecco's phosphate buffered saline (Mediatech, Inc.) containing 0.9 mM CaCl 2 x 2 H 2 O, 0.5 mM MgCl 2 x 6 H 2 O and 1% (w/v) BSA.
- the complement source was human serum from a healthy adult with no detectable intrinsic bactericidal activity.
- bactericidal activity For synergism of mAb bactericidal activity, equal quantities of two mAbs ranging from 0.4 to 50 ug/ml (final concentration) were used.
- the bactericidal activity (BC 50 ) of the mouse antiserum (or mAb combination) was defined by the dilution (or mAb concentration) that gave a 50% decrease in the number of CFU after 60 min incubation at 37 °C as compared with the CFU at time 0 in the negative control reactions.
- JAR mAbs were used as tools to determine amino acid residues in fHBP that contribute to the epitopes for binding of these mAbs so as to provide for structural predictions on the locations of epitopes of fHBP from different variant groups that interact with bactericidal antibodies. This information could then be used to construct chimeric fHBP vaccines that express epitopes from more than one variant group and that are capable of eliciting antibodies that confer protection against strains expressing different fHBP variants.
- the protein was divided into three domains, designated A, B and C ( Giuliani et all. Infect Immun 2005;73:1151-60 ).
- a domain is highly conserved across v.1 and v.2 variant groups, whereas the B and C domains contain sequences that diverge among strains.
- B and C domains contain sequences that diverge among strains.
- the only known fHBP epitope interacting with a bactericidal mAb was located in the C domain at R204 (Giuliani et al. supra ). (Note that the convention of numbering amino acid residues beginning with the first residue after the signal sequence is adopted herein).
- a chimeric protein vaccine composed of the B domain from a variant 3 strain (B 3 ) fused with the C domain of a variant 1 strain (C 1 ) failed to elicit protective bactericidal responses against strains with either variant 1 or 3 fHBP.
- JAR3/5" epitope an epitope defined by two anti-fHBP mAbs, JAR 3 and 5 (referred to herein as the "JAR3/5" epitope), in the B 1 domain around residue G121.
- JAR 3 individually was known to be bactericidal with human complement against strains from sequence type (ST) complex 32 ( Welsch et al. J Immunol 2004;172:5606-15 ) and, both JAR 3 and JAR 5 when combined with other mAbs were broadly bactericidal against strains expressing subvariants of variant 1 fHBP (Welsch et al., supra ).
- JAR 3 Madico et al.
- the chimeric fHBP provided for a polypeptide that elicited broadly protective antibodies against v.2 or v.3 strains.
- the animals developed serum bactericidal antibody responses against strains expressing fHBP v.1, v.2 or v.3 whereas as expected the serum bactericidal antibody responses of the control mice immunized with the wild-type recombinant fHBP v.1 were nearly entirely restricted to strains expressing fHBP v.1, and those of the control mice immunized with the wild-type recombinant fHBP v.2 were restricted to v.2 or v.3 (which from previous studies were known to cross-react ( Masignani 2007 J Exp Med , supra and Beernink 2007 J. Infect Dis supra ).
- the results provide proof of concept that an individual chimeric
- a chimeric protein vaccine composed of the A 1 domain (which is highly conserved across variant 1 and 2), the N-terminal portion of the B 1 domain expressing the JAR 3/5 epitope fused with the distal terminal portion of the B 1 domain and C 1 domain elicited cross-protective bactericidal antibodies in immunized mice.
- the JAR 11 epitope is expressed by about one-third of disease-producing N. meningitidis strains in the U.S. that express fHBP v.2 or v.3 ( Beernink 2007 J. Infect Dis, supra ). Approximately 50 percent of the JAR 11-negative strains with v.2 or v.3 fHBP express the JAR 32/35 epitope. Therefore, to increase coverage against these strains, the Chimera II vaccine was prepared, in which a single amino acid change, A174K, was introduced into the C domain that inactivated the epitope recognized by JAR 11 and introduced the epitope recognized by JAR 32/35.
- JAR 32 is often associated with expression of JAR 33 (for example, strains 03S-0658, M1239 and SK104, Table in Figure 8A ), while expression of JAR 11 is usually associated with expression of JAR 10 (see for example our strains 8047, MD1435 and MD1321, Figure 8A ).
- JAR 33 for example, strains 03S-0658, M1239 and SK104, Table in Figure 8A
- JAR 11 is usually associated with expression of JAR 10 (see for example our strains 8047, MD1435 and MD1321, Figure 8A ).
- bactericidal activity of antibodies is enhanced when two antibodies bind their respective epitopes located at a distance of about 18 - 20 ⁇ . Stated differently, a greater bactericidal effect was observed when two antibodies bound epitopes located about 18-20 ⁇ apart on the chimeric fHBP compared to the bactericidal effect of these antibodies alone. In contrast, binding of two antibodies to epitopes positioned at a greater distance apart (e.g., ⁇ about 27 ⁇ ) did not enhance bactericidal activity, which may be due to the reduced ability of these bound antibodies to provide for enhanced interaction with C1q of the complement cascade.
- chimeric fHBP which contain epitopes that elicit antibodies that bind to epitopes within about 18 - 20 ⁇ apart can provide for further enhanced bactericidal antibody production.
- epitope pairs are those epitopes bound by JAR 10 and JAR 11; and by JAR 33 and JAR 32/ 35 (JAR 32 and JAR 35 bind to the same (or overlapping) epitopes).
- chimeric fHBP polypeptides as vaccines can be further enhanced by including epitopes that elicit antibodies that block fH binding.
- epitopes that elicit antibodies that block fH binding.
- JAR 13 v.2 epitope
- JAR 11 v.2 epitope
- JAR 32/35 v.3 epitope
- EXAMPLE 1 IDENTIFICATION OF AMINO ACID RESIDUES OF FHBP EPITOPES IMPORTANT FOR JAR 3/5 MAB BINDING
- JAR 3 and JAR 5 were known to bind to v.1 or subvariants of v.1 fHBP expressed by strains MC58, 4243, M1390, and NZ98/254 but not to strain M6190 ( Welsch et al. J Immunol 2004;172:5606-15 ).
- fHBP expressed by M6190 had an arginine at position 121 (R121) whereas the fHBPs from the four reactive strains had glycine at position 121 (G121) ( Welsch et al. J Immunol 2004;172:5606-15 ).
- site-specific mutagenesis was used to change the glycine residue at position 121 in the fHBP sequence of strain MC58 to arginine.
- EXAMPLE 2 IDENTIFICATION OF AMINO ACID RESIDUES OF FHBP EPITOPES IMPLICATED IN JAR MAB BINDING
- Figures 30-32 provide supporting data for identification of residues involved in JAR mAb binding.
- E. coli lysates containing plasmids expressing the respective wild-type and mutant fHBPs were analyzed by Western blot using the appropriate JAR mAb, as well as a control antibody to detect an epitope tag present on the fHBP (penta-His).
- Figure 30 is a Western blot indicating residues involved in the JAR 10 and JAR 33 epitopes, in which E. coli lysates containing plasmids expressing the respective wild-type and mutant fHBPs were analyzed by Western blot with JAR 10 (Panel A) or Penta-His mAb (Panel B).
- Figure 31 is a Western blot indicating a residue involved in the JAR 11, JAR 32 and JAR 35 epitopes, in which E.
- Figure 32 is a Western blot indicating residue involved in the JAR 13 epitope, in which E. coli lysates containing plasmids expressing wild-type and mutant fHBPs were were probed with JAR 13 (Panel A) or Penta-His mAb (Panel B) and anti-mouse IgG-HRP secondary antibody.
- the amino acid sequences of the v.2 protein (with fHBP from strain 8047 used as the reference v.2 amino acid sequence) and v.3 fHBP (with fHBP from strain M1239 used as the reference v.3 amino acid sequence) differ by -1 and +7 amino acid residues, respectively, from that of MC58.
- a leucine residue (L) referred to using the numbering system herein as being at position 166 of the v.2 or v.3 fHBP sequence is actually at position 165 of the v.2 protein and at position 173 in the v.3 protein based on the actual amino acid sequence of these proteins, rather than on the numbering used herein based on the alignment of these sequences with v. 1 fHBP of MC58.
- FIG. 19 is a series of graphs showing the ability of representative JAR mAbs prepared against fHBP v.2 (8047), v.3 (MI239), or v.1 (MC58) recombinant proteins to give concentration-dependent inhibition of binding of fH to rfHBP v.2 (Panel A), rfHBP v.3 (Panel B), or rfHBP v.1 (Panel C) in an ELISA.
- These data show that some of the contact residues defined by the JAR mAb epitopes are involved in binding to fH.
- the epitopes defined by JAR 3 and JAR 5 are located within the B domain of variant 1 fHBP beginning approximately 19 amino acid residues N-terminal to the start of ⁇ -helix AH2, or approximately 15 amino acid residues N-terminal to the amino acid sequence of GEHT,.
- a first chimeric fHBP (referred to herein as "Chimera I") was constructed by combining a portion of the gene encoding the A domain and the N-terminal portion of the B domain up to residue G136 from v.1 fHBP of MC58 with the distal portion of the gene encoding the alpha-helix of the B domain and C domain of v.2 fHBP from strain 8047.
- the residue at position G136 was used as a convenient crossover position (the point at which the chimeric sequence "shifted" from that of the v.1 fHBP to that of the v.2 fHBP).
- G136 is N-terminal the ⁇ -helix AH2 and begins a sequence of four highly conserved residues, GEHT, which are shown in a box in Figure 4 .
- the outer brackets show the region of the protein previously defined as the B domain ( Giuliani et al. Infect Immun 2005;73:1151-60 ).
- Chimera II A second chimeric fHBP, referred to herein as Chimera II, was generated.
- Chimera II was identical in amino acid sequence to Chimera I except for the introduction the A174K substitution (Bold and underlined K, Chimera II, Figure 4 ). It should be noted that the A domain is not shown in Figure 4 , or in the NMR-based structure of Figure 5 , but would be attached at the N-terminus labeled "N" in Figure 5 .
- Chimera I contains the JAR 11 epitope, including residue A174 ( Figure 5 , Panel A).
- Chimera II contains the JAR 32 and JAR 35 epitopes, including residue K174 ( Figure 5 , Panel B).
- the model of the fHBP chimeras was constructed based on the NMR structure of Cantini et al. J Biol Chem 2006;281:7220-7 .
- Recombinant proteins were expressed in E. coli as C-terminal hexahistidine (His 6 ) fusions, which were purified by metal chelate chromatography. Specifically, Proteins were expressed from pET21-based plasmids in E. coli BL21(DE3) as C-terminal hexa-histidine fusions. Fusion proteins were then isolated by metal chelate chromatography according to methods known in the art. Isolated proteins were dialyzed against 1x PBS, 5% sucrose, 1 mM DTT and filter sterilized. Proteins (5 ⁇ g each) were separated on a 4-12% polyacrylamide gel and stained with Coomassie blue.
- Lane 1 mass standard; 2, fHBP v.1 (MC58); 3, fHBP v.2 (8047); 4, fHBP Chimera I; 5, fHBP Chimera II.
- EXAMPLE 5 EPITOPE EXPRESSION BY CHIMERIC ANTIGENS.
- JAR 1 which binds to a v.1 epitope in the C domain (R204), did not bind to either of the chimeric proteins ( Fig. 7 , Panel A).
- Figure 7 Panel B, provides binding data for mAbs JAR 10, 11 and 13, which were from a mouse immunized with v.2 or fHBP. All three mAbs recognize epitopes on the C domain of fHBP v.2 of strain 8047 ( Figure 20 ), and they showed similar respective concentration-dependent binding with the Chimera I protein as they did with the wild-type rfHBP v.2 control protein expressed from the gene of strain 8047 ( Fig. 7 , Panel B).
- JAR 11 did not bind to Chimera II, since this protein had lysine substituted for alanine at position 174 (A174K), which eliminated the JAR 11 epitope and introduced the JAR 32 epitope (Panel C).
- JAR 36 which cross-reacts with an epitope not yet defined but present on fHBP v.2 and v.3 fHBP bound to both of the chimeric proteins, and to the wild-type rfHBP v.2 control but not with the fHBP v.1 control ( Fig. 7 , Panel C).
- the proteins shown in Figure 6 were used to immunize mice according to the schedule in Table 1, below.
- Four doses of vaccine (20 ⁇ g of protein) were administered IP with intervals of 2 weeks between doses. Mice were bled 2.5 weeks after dose 4.
- CFA complete Freund's adjuvant
- IFA incomplete Freund's adjuvant
- Al(OH) 3 aluminum hydroxide.
- CFA/IFA below indicates that the mice received an initial dose with CFA, then subsequent booster doses with IFA. Where Al(OH) 3 was used as the adjuvant, all doses were administered with aluminum hydroxide as the adjuvant. Table 1.
- Figure 9 summarizes the serum antibody responses of the mice that received the chimeric vaccines administered with FA when measured against strain H44/76 (variant 1) and four additional strains that express subvariants of v.1 fHBP (i.e., fHBP proteins with relatively small amino acid differences (e.g., with greater than about 88%, and less than 97% amino acid sequence identity) between the sequence of the respective protein and that of v.1.1 fHBP of H44/76).
- variant 1 strain 1
- fHBP proteins with relatively small amino acid differences e.g., with greater than about 88%, and less than 97% amino acid sequence identity
- mice immunized with the wild-type rfHBP v.1 control protein had high responses to H44/76 (reciprocal GMT of nearly 10,000) and lower and variable responses against the other four test strains (ranging from a GMT of ⁇ 1:10 against strain NZ98/254 to a GMT of >1:1,000 against SK084).
- the sera from the mice immunized with the rfHBP v.2 control protein were either negative for bactericidal activity (bactericidal titers ⁇ 1:10, four strains) or weakly positive (reciprocal GMT of 1:10; strain SK141).
- mice immunized with either chimeric protein vaccine developed serum bactericidal antibodies against all four strains that were susceptible to bactericidal activity of sera from the control mice immunized with rfHBP v.1.
- the respective reciprocal GMTs of the chimeric vaccine groups where ⁇ 1 log lower than those of mice given the control rfHBP v.1 vaccine whereas the responses to the fifth strain, SK141, were as high or higher than those of the mice given the control rfHBP v.1 vaccine.
- Figure 10 summarizes the serum bactericidal antibody responses as measured against the six strains expressing fHBPs in the v.2 or v.3 variant groups. Three of the strains were JAR 11 positive (left panel) and three were JAR 32 positive (right panel). Sera from control mice immunized with rfHBP v.2 were bactericidal against all six strains whereas, with one exception (strain 03S-0658), the serum bactericidal titers of control mice immunized with rfHBP v.1 were ⁇ 1:10. The sera from the mice immunized with either chimeric vaccine were bactericidal against all six strains.
- the respective titers were ⁇ 1 log lower than those of the control mice immunized with rfHBP v.2.
- the titers elicited by one or both chimeric vaccines were similar to those of the mice given the positive control rfHBP v.2 vaccine.
- the chimeric vaccines elicited bactericidal antibody responses against strains expressing fHBP from each of the three antigenic variant groups.
- the Chimera I vaccine expressed the JAR 11 epitope while the Chimera II vaccine expressed the JAR 32 epitope ( Fig. 1 ).
- the respective responses of mice immunized with either chimeric vaccine when measured against strains expressing JAR 11- or JAR 32-positive fHBP were not significantly different from each other ( Fig. 5 ).
- Figure 11 summarizes the serum bactericidal antibody responses of mice immunized with the chimeric vaccines when absorbed with aluminum hydroxide as measured against the panel of test strains with v.1 fHBP.
- the corresponding data for responses to test strains expressing v.2 or v.3 fHBP are shown in Figure 12 .
- the respective responses to the different vaccines absorbed with aluminum hydroxide paralleled those observed to the vaccines given with Freund's adjuvant although as expected the titers were somewhat lower with the aluminum hydroxide adjuvant.
- JAR3/5 epitope which is common to virtually all v.1 proteins but is not present in fHBP from v.2 or v.3 strains, is important for eliciting high bactericidal antibody titers to the variant 1 fHBP protein.
- This discovery that the epitope recognized by JAR 3/5 plays an important role in eliciting v.1 fHBP bactericidal antibodies provides the basis for the rational design of further chimeric fHBP vaccines that can elicit bactericidal antibodies across strains expressing different fHBP protein variants, particularly against both v.1 and v.2 fHBP-expressing strains.
- the two chimeric vaccines described above included, from N-terminus to C-terminus:
- EXAMPLE 8 NATURAL OR SYNTHETIC POLYMORPHISMS OF V.1 FHBP B DOMAINS
- Figure 13 provides an alignment of fHBP v.1 sequences with natural polymorphisms in the N-terminal portion of the B domain.
- sequence conservation is shown below the alignment, with "*” denoting residues that are identical, “:”denoting residues that are conserved, and “.”denoting residues that are semi-conserved across the aligned sequences.
- the positions of alpha-helices are shown above the alignment, with the residues implicated in the alpha helices indicated by italics.
- the residue, G121 which is implicated in the JAR 3 and JAR 5 epitope, is shown in bold and underlining.
- a lysine at position 122 also appears to be important in the JAR 3/5 epitope, since one strain that is negative for JAR 3 and JAR 5 binding, 03S-0408, has G121 but differs from JAR 3/5 reactive strains in having serine at position 122 (S122). (data not shown)
- the amino acid sequence of GEHT that provides the point at which the B domain sequence of the chimera "switches” or "crosses over" to the amino acid sequence of a v.2 B domain in Chimera I and Chimera II (referred to herein as the "junction point" is shown in the box.
- the alignment thus provides guidance as to the types of amino acid substitutions that can be introduced while maintaining JAR 3/5 epitope expression.
- amino acid substitutions can be either naturally-occurring (i.e., natural polymorphisms) or can be introduced by synthetic means (e.g., recombinant polymorphisms).
- the heterologous B domains of the chimeric fHBP polypeptides contemplated herein include those containing v. 1 B domain sequences with natural and synthetic polymorphisms in the proximal B domain, including both natural and synthetic variants.
- chimeric fHBPs contemplated herein generally include one or more epitopes of v.2 fHBP B and C domains, where the v.2 fHBP B domain epitopes are present at a location C-terminal to (i.e., distal to) the location of the JAR 3/5 epitope of v.1 fHBPs, which is generally C-terminal to the alpha helix that follows the sequence of GEHT, which is shared between v.1 and v.2 fHBPs.
- Figure 14 provides an alignment of exemplary v.2 fHBP sequences of the distal portion of the B domain, and further provides exemplary v.2 fHBP sequences of the C domain, where the B domain is generally defined as residues 101 to 164, with numbering based on MC58 fHBP as a reference.
- Figures 13 and 14 provide 7 exemplary amino acid sequences of the N-terminal region of the v.1 B domain ( Figure 10) and 9 exemplary amino acid sequences for the distal portion of the B domain of v.2 fHBP and for the C domain of v.2 fHBP ( Figure 11 ).
- the sequences in Figures 13 and 14 provide for a least 63 different fHBP chimeras, simply by combining the amino acid sequences as provided. Further, the alignments provide guidance as to the amino acid residues that can be substituted.
- these exemplary sequences provide guidance for use of amino acid sequences containing naturally-occurring polymorphisms, they also provide guidance for production of synthetically-generated variants (e.g., using recombinant methods).
- additional point mutations may be introduced into the coding nucleic acid to provide for fHBP chimeras that express other desirable epitopes, such as the v.1 epitope recognized by JAR 1/mAb 502 that is in the portion of the C domain (R204), or the JAR 11 epitope in Chimeras IV and V.
- JAR1/mAb 502 epitope can provide for improved cross-reactivity against v.1 strains from the ST-32 lineage that nearly always express the JAR 1 epitope, while eliciting antibodies to the JAR 11 epitope can provide for improved titers against v.2 strains (see Koeberling et al., J Infect Dis 2008, 198:262-270 , for a description of v.1.1).
- JAR 32 is often associated with expression of JAR 33
- JAR 11 is usually associated with expression of JAR 10 (see, for example, strain panel, Figure 8 ).
- Table 2 and Figures 15 and 16 provide for additional hypothetical chimeric vaccines, designated Chimera III, Chimera IV and Chimera V.
- Each of these chimeric fHBPs are generated using a strategy similar to that used to generate Chimera I to provide for a chimeric fHBP that elicits bactericidal anti-v.1 and v.2 antibodies.
- Chimera III contains the A domain and proximal B domain of subvariant v.1.10 encoded by the fHBP from NZ98/254, and uses the same distal B domain and C domain of Chimera I and Chimera II.
- Chimera IV illustrated in Figure 15 , includes the A and proximal B domains of Chimera I and Chimera II, but substitutes the distal B and C domains of v.2 from strain 8047 (v.2.1) of these chimera with those from RM1090 (v.2 subvariant).
- Chimera V fuses the A and proximal B domains of a v. 1 subvariant (strain NZ98/254) with that distal B and C domains of v.2 subvariant (strain RM1090).
- Chimeras III and V can provide for increased breadth of protection against certain strains expressing subvariants of v.1, such as NZ98/254, which is not covered by the Chimera I or II vaccines.
- Chimeras IV and V can provide for extended protection against v.3 strains, which are poorly covered by Chimera I or Chimera II.
- Table 2 provides a summary of the observed epitope expression for Chimera I and Chimera II, and further sets out the predicted epitope expression for proposed Chimeras III, IV, and V.
- Table 2 Predicted (or observed) epitope expression by chimeric proteins Variant 1 Variant 1/2/3 Variant 2/3 mAb mAb 502/J AR1 JAR 3/5 JAR 10 JAR 11 JAR 13 JAR 32/35 JAR 33 Domain C B C C C C C C Epitope R204 G121 K180 and E192 A174 S216 K174 R180, E192 Wild-type proteins MC58 (v.1) 1 1 0 0 0 0 0 NZ98/254 (v.1, sv) 0 1 1 0 0 0 0 8047 (v.2) 0 0 1 1 1 0 0 RM1090 (v.2, sv) 0 0 0 0 0 1 1 Chimeric proteins Chimera I 0 1 1 1 1 1 0 0 Chimera II
- mAb 502 was described by Giuliani et al (Infect Immun 2005; 73:1151-60 ). JAR 3 and 5, were prepared against a v.1 fHBP (gene from strain MC58) ( Welsch et al. J Immunol 2004; 172:5606-15 ). JAR 10, 11 and 13, were prepared against a v.2 protein (gene from strain 2996) ( Beernink et al. J Infect Dis 2007; 195:1472-9 ), and JAR 32, 33 and 35 were prepared against a v.3 protein (gene from strain M1239). Each of the mAbs reacts with the variant protein, which was used to immunize the mouse.
- Chimeras I and II were constructed to contain amino acid residues 1 to 135 encoded by fHBP gene v.1.1 (MC58) fused with residues 136 to 255 of v.2.1 gene from 8047. Chimera II also contains a point mutation A174K introduced into the C domain that inactivates the epitope recognized by JAR 11 and introduces the epitope recognized by JAR 32/35. Proposed Chimeras III, IV and V are examples of additional chimeric fHBPs, with predicted epitope expression as defined by binding of the respective JAR mAbs shown.
- chimeric fHBP include varying the residue within the heterologous B domain at which the v.1 fHBP B domain sequence ends and the v.2 (or v.2) fHBP B domain sequence ends.
- residue G136 was used as the position of the "crossover" between fHBP variants, the "crossover" residue can be any residue C-terminal of the amino acid sequence defining the JAR 3/JAR 5 epitope and a residue within M123-S136 can also be selected.
- residue positions C-terminal to G136 (E137-D142), or residue positions adjacent or within ⁇ -helix AH2 (K143-A150, preceding the first beta-strand) can be suitable crossover residue positions.
- crossover residue positions are contemplated herein, where the crossover residue may be positioned after G121 of the JAR 3/5 epitope (G121) through and including A174 of the JAR 11 epitope, where the presence of the JAR 3/5 epitope can be assessed using immunoassay methods known in the art, (Note that numbering above is based on the amino acid sequence number of the fHBP reference sequence of MC58.)
- Figure 33 shows a Western blot of samples of N. meningitidis expressing either wildtype (WT) or a chimeric fHBP (Chimera I (see Fig. 23 )).
- the Chimera I corresponded to a full-length fHBP and further included the signal sequence (but lacked any epitope tags, such as a Penta-His tag)
- bacterial cells transformed with the plasmid containing the gene encoding Chimera I were positive for both anti-fHbp mAbs, whereas the cells from H44/76 transformed with the plasmid containing the gene encoding fHbp v.2 or WT H44/76 react only with JAR 3 (v.1) and the cells from 8047 react only with JAR 13 (v.2).
- Hybridomas producing the JAR 4, JAR 5, JAR 11, and JAR 32 monoclonal antibodies were deposited under the terms of the Budapest Treaty with the American Type Culture Collection, 10801 University Boulevard., Manassas, Va. 20110-2209, USA (ATCC) on the date indicated in the table below, and were assigned the designations set out in the table below. ATCC Deposit No. (Deposit Date) Material Deposited PTA-8943 (Feb. 7, 2008) Hybridoma producing JAR 4 Monoclonal Antibody PTA-8941 (Feb. 7, 2008) Hybridoma producing JAR 5 Monoclonal Antibody PTA-8940 (Feb.
- JAR 5 mAb specifically binds to an epitope that at least overlaps with the epitope specifically bound by JAR 3 mAb
- JAR 32 mAb specifically binds to an epitope that at least overlaps with the epitope specifically bounds by JAR 35 mAb.
Landscapes
- Health & Medical Sciences (AREA)
- Chemical & Material Sciences (AREA)
- Life Sciences & Earth Sciences (AREA)
- Immunology (AREA)
- Medicinal Chemistry (AREA)
- Organic Chemistry (AREA)
- General Health & Medical Sciences (AREA)
- Public Health (AREA)
- Pharmacology & Pharmacy (AREA)
- Veterinary Medicine (AREA)
- Animal Behavior & Ethology (AREA)
- Biochemistry (AREA)
- Microbiology (AREA)
- Proteomics, Peptides & Aminoacids (AREA)
- Molecular Biology (AREA)
- Genetics & Genomics (AREA)
- Epidemiology (AREA)
- Biophysics (AREA)
- Mycology (AREA)
- General Chemical & Material Sciences (AREA)
- Nuclear Medicine, Radiotherapy & Molecular Imaging (AREA)
- Chemical Kinetics & Catalysis (AREA)
- Bioinformatics & Cheminformatics (AREA)
- Engineering & Computer Science (AREA)
- Oncology (AREA)
- Communicable Diseases (AREA)
- Peptides Or Proteins (AREA)
- Medicines Containing Antibodies Or Antigens For Use As Internal Diagnostic Agents (AREA)
Abstract
Chimeric fHBPs that can elicit antibodies that are bactericidal for different fHBP variant strains of N. meningitidis, and methods of use, are provided.
Description
- This application claims priority benefit of
U.S. provisional application serial no. 61/035,329, filed March 10, 2008 U.S. provisional application serial no. 61/037,252, filed March 17, 2008 - This invention was made with government support under Public Health Service grant nos. R01 AI46464 and C06 RR16226. The government has certain rights in this invention.
- This invention relates to vaccines for diseases caused by Neisseria meningitidis.
- Neisseria meningitidis is a Gram-negative bacterium which colonizes the human upper respiratory tract and is responsible for worldwide sporadic and cyclical epidemic outbreaks of, most notably, meningitis and sepsis. The attack and morbidity rates are highest in children under 2 years of age. Like other Gram-negative bacteria, Neisseria meningitidis typically possess a cytoplasmic membrane, a peptidoglycan layer, an outer membrane which together with the capsular polysaccharide constitute the bacterial wall, and pili, which project into the outside environment. Encapsulated strains of Neisseria meningitidis are a major cause of bacterial meningitis and septicemia in children and young adults. The prevalence and economic importance of invasive Neisseria meningitidis infections have driven the search for effective vaccines that can confer immunity across different strains, and particularly across genetically diverse group B strains with different serotypes or serosubtypes.
- Factor H Binding Protein (fHBP, also referred to in the art as lipoprotein 2086 (Fletcher et al, Infect Immun 2004;72:2088-2100), Genome-derived Neisserial antigen (GNA) 1870 (Masignani et al. J Exp Med 2003;197:789-99) or "741") is an N. meningitidis protein which is expressed in the bacterium as a surface-exposed lipoprotein. Based on sequence analysis of 71 N. meningitidis strains representative of its genetic and geographic diversity, N. meningitidis strains have been sub-divided into three fHBP variant groups (referred to as variant 1 (v.1), variant 2 (v.2), and variant 3 (v.3)) based on amino acid sequence variability and immunologic cross-reactivity (Masignani et al. J Exp Med 2003; 197:789-99). Other workers (Fletcher et al, 2004) have subdivided the protein into two sub-families designated A (which includes v.2 and v.3 of Masignani) and B (v.1).
Variant 1 strains account for about 60% of disease-producing group B isolates (Masignani et al. 2003, supra). Within each variant group, there is on the order of about 92% or greater conservation of amino acid sequence. Specifically, conservation within each variant group ranges between 89 and 100%, while between the variant groups (e.g., between v.1 and v.2) the conservation can be as low as 59%. The protein is expressed by all known strains of N. meningitidis. - Mice immunized with recombinant fHBP developed high serum bactericidal antibody responses against strains expressing fHBP proteins of the homologous variant group (Masignani et al. 2003, supra; Welsch et al. 2004, J Immunol. 172(9):5606-15.). Thus, antiserum prepared against fHBP v.1 confers protection against N. meningitidis strains expressing fHBP v.1, but not against strains expressing fHBP v.2 or v.3. Similarly, antiserum prepared against fHBP v.2 protects against strains expressing v.2 (or v.3) but not v.1 (Masignani et al. J Exp Med 2003, 197:789-99; Beernink et al. J Infect Dis 2007;195:1472-9). For vaccine purposes, it would be desirable to have a single protein capable of eliciting cross-protective antibodies against fHBP from different variant groups.
- Chimeric proteins have been used for vaccine development in a variety of ways. For example, a first strategy employs a genetic or chemical linkage of an antigen to a known, but unrelated, immunogenic protein, such as the diphtheria, tetanus or pertussis toxoid proteins, or the cholera toxin B (CTB) domain, in order to enhance the magnitude of the antibody responses to the antigen of interest. A second strategy uses a genetic fusion of two antigens from the same organism, to enhance cross-protection against strains with antigenic diversity (Giuliani et al. Infect Immun 2005 73:1151-60). An example is the multivalent group B meningococcal recombinant protein vaccine, which contains a mixture of two fusion proteins: a first fusion protein of a GNA2091 protein and a GNA1870 (or "fHBP") protein, and a second fusion protein of a GNA2132 protein and a GNA1030 protein (Giuliani et al. Proc Natl Acad Sci U S A 2006, 103:10834-9). A third strategy has been to construct a fusion of different serologic variants ("serovars") of one antigen to induce cross-protection against a strains with antigenic diversity. An example is a tetravalent OspC chimeric Lyme disease vaccine, which induced bactericidal antibody responses against spirochete strains expressing each of the OspC types that were incorporated into the construct (Earnhart et al. Vaccine 2007;25:466-80).
- In the examples of chimeric vaccines described that were designed to broaden protective immune responses, the vaccines were composed of repeats of an individual domain with antigenic variability. The respective variants of the domain were expressed in tandem in one protein (i.e., the same domain from different strains, A1-A2-A3-A4, etc). In some cases, these recombinant tandem proteins can be convenient for manufacturing and quality control. However they also can be very large and subject to improper folding or degradation.
- One approach to avoiding the problem of large tandem fusion proteins is to design a single polypeptide that is composed of different domains of two antigenic variants e.g., by "swapping" different individual domains of an antigen, or even smaller regions such as individual epitopes from two different proteins, to form a chimeric protein that expresses antigenically unrelated epitopes specific for more than one strain (i.e., different domains from two different strains, A1-B2 or A2-B1, etc.).
- This latter approach was undertaken with fHBP. First, in order to facilitate identification of bactericidal regions of fHBP, the protein was divided into three domains, designated A, B and C (Giuliani (2005) Infect. Immun. 73:1151-1160). The A domain is highly conserved across variant groups, whereas the B and C domains contain sequences that diverge among strains. Giuliani et al. identified an fHBP epitope interacting with a bactericidal mAb located in the C domain at R204 (Giuliani (2005) supra). However, a chimeric protein containing the B domain from a
variant 3 strain (B3) fused with the C domain of avariant 1 strain (C1) failed to elicit protective bactericidal responses against strains with either v.1 or v.2 fHBP. - Vaccines that exploit the ability of fHBP to elicit bactericidal antibody responses and that can elicit such antibodies that are effective against strains expressing different fHBP variants remain of interest.
- Chimeric fHBPs that can elicit antibodies that are bactericidal for different fHBP variant strains of N. meningitidis, and methods of use, are provided.
-
Figure 1 is a collection of results of Western blot analysis illustrating the amino acid residues involved in binding of monoclonal antibodies (mAbs)JAR 3 andJAR 5 to factor H binding protein (fHBP). Panel A,JAR 5;lane 1, molecular mass standard;lane 2, pET21b;lane 3, pET21-fHBP(MC58 wildtype);lane 4, pET21-fHBP(MC58)G121R;lane 5, pET21-fHBP(M6190 wildtype)R121;lane 6, pET21-fHBP(M6190)R121G. Panel B,JAR 3. C, Penta-His mAb. Panels B and C have the same lane assignments as panel A. -
Figure 2 is a set of graphs illustrating that binding ofJAR 3 andJAR 5 mAbs to fHBP is competitive. Percent competitive inhibition of binding of anti-fHBP mAbs to fHBP by a second antibody as measured by ELISA. Each panel includes: rabbit polyclonal anti-fHBP antiserum; rabbit pre-immune serum; and a negative control mAb specific for an irrelevant capsular antigen (JW-C2, -A2 or -A1). Panel A, Inhibition of binding ofJAR 3 byJAR 4 orJAR 5. Panel B, Inhibition of binding ofJAR 5 byJAR 3 orJAR 4. Panel C, Inhibition of binding ofJAR 4 byJAR 3 orJAR 5. -
Figure 3 is a schematic illustrating positions of residues associated with the epitopes of the nine anti-fHBP mAbs ("JAR" mAbs) in the structural model based on previously reported NMR data (Cantini et al. "Solution structure of the immunodominant domain of protective antigen GNA1870 of Neisseria meningitidis." J Biol Chem 2006; 281:7220-7). Coordinates from the solution structure of the B and C domains of fHBP v.1 from strain MC58 were used to construct the model. Note that the positions of amino acid residues involved in the epitopes for antibodies raised against the fHBP v.2 and v.3 proteins are shown on the model, even though these antibodies do not bind to the v. 1 protein from strain MC58. It should also be noted that numbering of amino residues is based on the mature protein sequence of fHBP (i.e. lacking the signal sequence) from strain MC58. Because the amino acid sequences of the variant 2 (v.2) fHBP protein (from strain 8047) and variant 3 (v.3) fHBP (from strain M1239) differ by -1 and +7 amino acid residues, respectively, from that of MC58, the numbering used to refer to residues for v.2 and v.3 fHBP proteins differs from numbering based on the actual amino acid sequences of these proteins. Thus, for example, reference to a leucine residue (L) at position 166 of the v.2 or v.3 fHBP sequence inFigure 3 , refers to the residue at position 165 of the v.2 protein and at position 173 in the v.3 protein. For further clarification, seeFigure 4 for alignment. Details of the reactive and non-reactive residues are provided herein. The residue shown formAb 502 is from a previously reported study (Giuliani et al., 2005 Infect Immun 73:1151-60). The numbering is based on amino acid sequence of MC58 v.1 fHBP lacking the signal sequence (Masignani et al., 2003 J Exp Med 197:789-99). -
Figure 4 is a schematic providing an alignment of wild-type and chimeric fHBP amino acid sequences (alignment performed using ClustalW). The deduced amino acid sequences of fHBP v.1 from strain MC58 (bottom) and v.2 strain 8047 (top) are shown, along with the two chimeric sequences (middle, Chimera I and Chimera II). Numbering for all four proteins is based on the native, mature v.1 protein from MC58 (i.e., without the signal sequence). The recombinant fHBP protein as expressed in E. coli lacks both the signal sequence and seven presumably flexible residues (CSSGGGG). An N-terminal methionine was added to each sequence shown to facilitate expression in E. coli (not shown). A C-terminal sequence LEHHHHHH was added to each sequence shown to facilitate isolation (not shown). The identities of the chimeras with the respective wild-type sequences are shown with symbols above and below the alignment (* = identical; : = conserved; = semi-conserved). The position of the amino acid sequence of GEHT at residues 136-139 in the C-terminal portion of the B domain of 8047 following the junction point is indicated in a box. The outer brackets, which encompassresidues 101 to 164, show the region of the protein defined as the B domain (Giuliani et al. "The region comprising ). With one exception, Chimera I and Chimera II have identical amino acid sequences. The exception is at residue 174 where alanine in Chimera I has been replaced by lysine in Chimera II. The position of the A174K substitution in Chimera II is shown in bold. Sequence alignment was performed with ClustalW. -
Figure 5 is a schematic representation of chimeric fHBPs. The N-terminal portion of the B domain from the v. 1 fHBP is on the right, and the C-terminal portion of the B domain encompassing the α-helix of the v.2 protein together with the C domain of the v. 2 fHBP is on the left. The junction point for these chimeras, exemplified by G136 is indicated with an arrow and accompanying text. Both chimeric proteins express theJAR 3 andJAR 5 epitopes expressed on the B domain of fHBP v.1 and theJAR 10 epitope, which is on the C domain of subsets of strains expressing v.1, v.2 or v.3 fHBP. Chimera I contains theJAR 11 epitope, including residue A174 (Panel A), which is expressed on the C domains of a subset of strains expressing fHBP v.2 or v.3. Chimera II contains theJAR 32 /JAR 35 epitopes, including residue K174, which are expressed on the C domains of subsets of strains expressing fHBP v.2 or v.3. A domains are not shown in these representations. The model was constructed based on the NMR structure of Cantini et al. (2006) J Biol Chem 281:7220-7. -
Figure 6 provides the results of SDS-PAGE analysis of purified wild-type and mutant fHBPs. Proteins were expressed from pET21-based plasmids in E. coli BL21(DE3) as C-terminal hexa-histidine fusions and purified by metal chelate chromatography. Proteins were dialyzed against 1x PBS, 5% sucrose, 1 mM DTT and filter sterilized. Proteins (5 µg each) were separated on a 4-12% polyacrylamide gel and stained with Coomassie blue.Lane 1, mass standard; 2, fHBP v.1 (MC58); 3, fHBP v.2 (8047); 4, fHBP Chimera I; 5, fHBP Chimera II. -
Figure 7 is a set of graphs illustrating binding of individual anti-fHBP mAbs to recombinant proteins. Panel A shows mAbs prepared against fHBP v.1; Panel B, fHBP v.2; Panel C, fHBP v.3. The symbols represent different antigens on the plate: open squares, fHBP v.1; open circles, fHBP v.2; open triangles, Chimera I; asterisks, Chimera II. -
Figure 8A provides a table of strains used in the Examples, including those used to measure serum bactericidal antibody responses and description of the amino acid sequence identity compared with prototype fHBP v.1, v.2 and v.3 and JAR mAb binding of the respective fHBPs. -
Figure 8B shows the amino acid identities of different domains of fHBP. Comparisons are made for the A domain (residues 1-100), the B domain (residues 101-164) and the C domain (residues 165-255). Comparisons also are made for the B domain up to the junction point (101-135) and the B domain starting at the junction point (136-164). Numbering of amino acid residues is based on the mature protein (i.e. lacking the signal sequence) from strain MC58. -
Figure 9 is a graph illustrating serum bactericidal antibody responses of mice immunized with chimeric recombinant proteins given with Freund's adjuvant as measured against N. meningitidis group B strains expressing fHBP in the antigenic v.1 group. Strain H44/76 expresses fHBP v. 1 identical to that of the fHBP v. 1 control vaccine. The remaining strains express subvariants of fHBP v.1 (See Table inFigure 8A , above). Values are presented as 1/GMT (Reciprocal (or inverse) geometric mean titer) with a 95% confidence interval. -
Figure 10 is a graph illustrating serum bactericidal antibody responses of mice immunized with chimeric recombinant proteins given with Freund's adjuvant as measured against N. meningitidis group B expressing fHBP in the v.2 or v.3 antigenic groups.Strain 8047 expresses fHBP v.2 identical to that of control rfHBP v.2 vaccine. The remaining strains express subvariants of fHBP v.2 or v.3 (see Table inFigure 8A ). Values are presented as 1/GMT with a 95% confidence interval. The data are stratified based on strains reacting with JAR 11 (left panel) or JAR 32 (right panel). The Chimera I and II vaccines are identical except that Chimera I has residue A174 and is JAR 11-positive and JAR 32-negative, whereas Chimera II has residue K174 and is JAR 11-negative and JAR 32-positive. See figure for bar symbols. -
Figure 11 is a graph illustrating serum bactericidal antibody responses of mice immunized with chimeric recombinant proteins adsorbed to aluminum hydroxide as measured against N. meningitidis group B strains expressing fHBP in the antigenic v.1 group. Strain H44/76 expresses fHBP v.1 identical to that of the fHBP v.1 control vaccine. The remaining strains express subvariants of fHBP v.1. Values are presented as 1/GMT (i.e., reciprocal (or inverse) geometric mean titer) with a 95% confidence interval. Bar symbols for each vaccine are as shown inFigure 10 . -
Figure 12 is a graph illustrating serum bactericidal antibody responses of mice immunized with chimeric recombinant proteins adsorbed to aluminum hydroxide as measured against N. meningitidis group B expressing fHBP in the v.2 or v.3 antigenic groups.Strain 8047 expresses fHBP v.2 identical to that of control rfHBP v.2 vaccine. The remaining strains express subvariants of fHBP v.2 or v.3 (see Table inFigure 8 ). Values are presented as 1/GMT with a 95% confidence interval. The data are stratified based on strains reacting with JAR 11 (left panel) or JAR 32 (right panel). The Chimera I and II vaccines are identical except that Chimera I is JAR 11-positive and JAR 32-negative, whereas Chimera II is JAR 11-negative and JAR 32-positive Bar symbols for each vaccine are as shown inFigure 10 . -
Figure 13 is a schematic showing alignment of fHBP v.1 amino acid sequences with natural polymorphisms in the N-terminal portion of the B domain. In the alternative nomenclature based on three dimensional structural data of the entire fHbp molecule, the sequence shown also comprises a C-terminal portion of the fHbpN domain and a small N-terminal portion of the fHbpC domain as indicated above the alignment. The sequence conservation is shown below the alignment (code as inFigure 4 ). The positions of α-helices are shown above the alignment. The position of the junction point in the chimeric proteins is shown in the box. Numbering is based on the mature protein (i.e. lacking the signal sequence) from strain MC58. Strains MC48, M4105, 4243, NZ98/254 are positive for JAR3/JAR 5 reactivity; strains M6190 and 03S-0408 are negative forJAR 3/5 reactivity, and strains NM452 and CDC1573 have not been tested. The residues G121 and K122, which are associated withJAR 3 andJAR 5 mAb epitopes, are shown in bold and underlined text. Note that althoughstrain 03S-0408 has G121, it is negative forJAR 3/5 reactivity. This strain has three amino acid differences betweenpositions -
Figure 14 is a schematic showing alignment of fHBP v.2 amino acid sequences with natural polymorphisms in the carboxyl-terminal portion of the B domain and the C domain, or alternatively, the complete fHbpC domain based on the three-dimensional structural nomenclature. The sequence conservation is shown below the alignment (code as in legend toFigure 4 ). The residues implicated in anti-fHBP mAb epitopes are designated with the number of the JAR mAb above the alignment: JAR 11 (alanine at residue position 174; A174); JAR 10 (lysine at residue position 180 and glutamate at position 192; K180 and E192); JAR 13 (serine residue at position 216; S216). Numbering in this figure is based on fHBP from strain MC58. -
Figure 15 is a schematic illustrating additional exemplary chimeric vaccines (Chimeras IIb, III, IV, and V). Chimera IIb can be made by introducing the K180R substitution into Chimera II. Chimeras III and V can be made using portions of the A and B domains of strain NZ98/254 (subvariant v.1) with the distal portion of the B domain and C domain of v.2 strain 8047 (Chimera III) or of subvariant v.2 strain RM1090 (Chimera V). Chimera IV uses the A and proximal B domains of MC58 with the distal B and C domains of RM1090. -
Figure 16 is a schematic showing an alignment of amino acid sequences of further exemplary chimeric fHBPs (Chimera III, IV and V) in the region of the crossover position, which is indicated by the box (residues GEHT). The residues, G121 and K122, implicated in theJAR 3 andJAR 5 epitopes are shown in bold and underlining. -
Figure 17 provides a table summarizing cross-reactivity of the different JAR mAbs, their respective Ig isotypes and ability to inhibit binding of human fH. -
Figure 18 is a table listing human complement-mediated bactericidal activity of each of the JAR mAbs when tested individually or in combination with a second anti-fHBP mAb. -
Figure 19 is a series of graphs showing the ability of representative JAR mAbs prepared against fHBP v.2 or v.3 proteins to give concentration-dependent inhibition of binding of fH to rfHBP in an ELISA. Panel A, Inhibition of binding of fH to rfHBP v.2. Panel B, Inhibition of binding of fH to rfHBP v.3. Respective v.2 and v.3 recombinant proteins are those encoded by the fHBP genes ofstrains 8047 and M1239. Panel C, Inhibition of binding of fH to rfHBP v.1. -
Figure 20 is a table listing certain properties of respective pairs of JAR mAbs with or without synergistic complement-mediated bactericidal antibody, including the positions of amino acid residues involved in the epitopes, distances between them, inhibition of fH binding and isotype of each mAb. -
Figure 21 provides the amino acid sequence of variant 1 (v.1) factor H binding protein (fHBP) of MC58, with the A, B and C domains indicated. Positions of the structural domains, fHbpN and fHbpC, are also shown. Glutamine 101 (Q) and glycine 164 (G) indicated by upward arrows define the A/B and B/C domain borders, respectively, as defined by Giuliani et al., Infect. Immun, 2005 73:1151-60. The upward arrow atglycine 136 designates the boundary between the fHbpN and the fHbpC domains, as defined by Cantini et al., J. Biol. Chem. 2009. -
Figure 22 shows the amino- (N-) and carboxyl- (C-) terminal portions of the B and C domains, which are defined with respect to the conserved amino acid sequence of GEHT. The amino acid sequences that can define aJAR 3/5 epitope are positioned N-terminal to the second alpha helix; the amino acid sequence that can define theJAR 11/32/35 epitopes are positioned C-terminal to the second alpha helix. Alpha-helix (AH) 2 is indicated. -
Figure 23 is a schematic showing Chimera I (MC58/8047) nucleotide and protein sequences. The sequence before the junction (cross-over) point is shown in lower case and the sequence following the junction point is shown in upper case. Lines of fifty residues are shown. Only the Neisserial sequences are shown; E. coli expression constructs contained an N-terminal Methionine and C-terminal hexa-histidine tag (LEHHHHHH). -
Figure 24 is a schematic showing Chimera II (MC58/8047 A174K) nucleotide and protein sequences. The sequence before the junction (cross-over) point is shown in lower case and the sequence following the junction point is shown in upper case. Lines of fifty residues are shown. Only the Neisserial sequences are shown; E. coli expression constructs contained an N-terminal Methionine and C-terminal hexa-histidine tag (LEHHHHHH). The A174K substitution is shown in bold and underlined text. -
Figure 25 is a schematic showing Chimera IIb (MC58/8047 A174K/K180R) nucleotide and protein sequences. The sequence before the junction (cross-over) point is shown in lower case and the sequence following the junction point shown in upper case. Lines of fifty residues are shown. Only the Neisserial sequences are shown; E. coli expression constructs contain an N-terminal Methionine and C-terminal hexa-histidine tag (LEHHHHHH). The A174K and K180R substitutions are shown in bold text. -
Figure 26 is a schematic showing Chimera III (NZ98254/8047) nucleotide and protein sequences. The sequence before the junction (cross-over) point is shown in lower case and the sequence following the junction point is shown in upper case. Lines of fifty residues are shown. Only the Neisserial sequences are shown; E. coli expression constructs contain an N-terminal Methionine and C-terminal hexa-histidine tag (LEHHHHHH). -
Figure 27 is a schematic showing Chimera IV (MC58/RM1090) nucleotide and protein sequences. The sequence before the junction (cross-over) point is shown in lower case and the sequence following the junction point is shown in upper case. Lines of fifty residues are shown. Only the Neisserial sequences are shown; E. coli expression constructs contain an N-terminal methionine and C-terminal hexa-histidine tag (LEHHHHHH). -
Figure 28 is a schematic showing Chimera V (NZ98254/RM1090) nucleotide and protein sequences. The sequence before the junction (cross-over) point is shown in lower case and the sequence following the junction point is shown in upper case. Lines of fifty residues are shown. Only the Neisserial sequences are shown; E. coli expression constructs contain an N-terminal methionine and C-terminal hexa-histidine tag (LEHHHHHH). -
Figure 29 provides a table showing positions of residues associated with JAR mAb binding. The reactive residue in fHBP was from the strain used as the source for immunization. For the anti-v.2 mAbs, the reactive strain is 8047, whose fHBP sequence is 99.6% identical to that fromstrain 2996. The non-reactive residue is that present in the non-reactive strain. Loss of reactivity associated with a change from the reactive to the non-reactive residue is indicated as knock-out (KO) and the converse change is indicated as knock-in (KI). -
Figure 30 provides an image of a Western blot indicating residues involved in theJAR 10 andJAR 33 epitopes. E. coli lysates containing plasmids expressing the respective wild-type and mutant fHBPs were analyzed by Western blot with JAR 10 (Panel A), Penta-His mAb (Panel B), or JAR 33 (Panel C). -
Figure 31 provides an image of a Western blot indicating a residue involved in theJAR 11,JAR 32 andJAR 35 epitopes. E. coli lysates containing plasmids expressing the respective wild-type and mutant fHBPs were analyzed by Western blot with JAR 32 (Panel A), JAR 35 (Panel B), JAR 11 (Panel C) or Penta-His mAb (Panel D). -
Figure 32 provides an image of a Western blot indicating residue involved in theJAR 13 epitope. E. coli lysates containing plasmids expressing wild-type and mutant fHBPs:lane 1, molecular weight marker;lane 2, pET21 (empty plasmid);lane 3, fHBP(8047)wt;lane 4, fHBP(8047)S216G;lane 5, fHBP(RM1090)wt;lane 6, fHBP(RM1090)G216S. Blots were probed with JAR 13 (Panel A) or Penta-His mAb (Panel B) and anti-mouse IgG-HRP secondary antibody. -
Figure 33 provides an image of a Western blot of wildtype (WT) or Chimeric fHBP expressed in N. meningitidis.Lane 1, H44/76 KO fHBP transformed with pCom-fHBP v.2 WT plasmid; 2, H44/76 KO fHbp transformed with pCom-Chimera I plasmid; 3, Kaleidoscope marker; 4, Magic Mark marker; 5, H44/76 (v.1) WT cells; 6, 8047 (v.2) WT cells; 7, 8047 KO fHBP cells; 8, recombinant (r) fHBP v.1 protein (gene from strain MC58); 9, rfHBP v.2 protein (gene from strain 8047). Upper panel, blot probed with anti-fHBP mAb JAR 3 (v.1); lower panel, blot probed with anti-fHBP mAb JAR 13 (v.2 or v.3). -
Figure 34 shows ribbon diagrams of full length v. 1 fHBPs. Panel A, fHBP is partitioned into three domains indicated by various shades of gray. The A domain and the N-terminal portion of the B domain are on the left and the boundary between the A and B domains is indicated by an arrow atlysine 100. The C-terminal portion of the B domain together with the C domain is on the right, where the boundary between the two is designated by an arrow atglycine 164. Panel B, an alternative nomenclature describes the fHBP as having two structural domains. The N-terminal domain containing a mix of α helices and β strands is named the fHbpN domain (left) and the C-terminal domain consisting of β strands is labeled as the fHbpC domain (right). The fHbpN and the fHbpC are connected by a linker at or proximal toglycine 136. In some embodiments, the junction point relevant for the chimeric fHBP described herein is at or proximal to G136, indicated by an arrow in both panels. The models shown in both panels are constructed based on the NMR structure of Cantini et al. J Biol Chem 2009. - Before the present invention and specific exemplary embodiments of the invention are described, it is to be understood that this invention is not limited to particular embodiments described, as such may, of course, vary. It is also to be understood that the terminology used herein is for the purpose of describing particular embodiments only, and is not intended to be limiting, since the scope of the present invention will be limited only by the appended claims.
- Where a range of values is provided, it is understood that each intervening value, to the tenth of the unit of the lower limit unless the context clearly dictates otherwise, between the upper and lower limit of that range and any other stated or intervening value in that stated range is encompassed within the invention. The upper and lower limits of these smaller ranges may independently be included in the smaller ranges is also encompassed within the invention, subject to any specifically excluded limit in the stated range. Where the stated range includes one or both of the limits, ranges excluding either both of those included limits are also included in the invention.
- Unless defined otherwise, all technical and scientific terms used herein have the same meaning as commonly understood by one of ordinary skill in the art to which this invention belongs. Although any methods and materials similar or equivalent to those described herein can also be used in the practice or testing of the present invention, the preferred methods and materials are now described. All publications mentioned herein are incorporated herein by reference to disclose and describe the methods and/or materials in connection with which the publications are cited.
- It must be noted that as used herein and in the appended claims, the singular forms "a", "an", and "the" include plural referents unless the context clearly dictates otherwise. Thus, for example, reference to "an antigen" includes a plurality of such antigens and reference to "the protein" includes reference to one or more proteins, and so forth.
- The publications discussed herein are provided solely for their disclosure prior to the filing date of the present application. Nothing herein is to be construed as an admission that the present invention is not entitled to antedate such publication by virtue of prior invention. Further, the dates of publication provided may be different from the actual publication dates which may need to be independently confirmed.
- The present disclosure provides chimeric fHBPs that can elicit antibodies that are bactericidal for different fHBP variant strains of N. meningitidis, and methods of use.
- "Factor H Binding Protein" (fHBP), which is also known in the literature as GNA1870, GNA 1870, ORF2086, LP2086 (lipoprotein 2086), and "741" refers to a polypeptide of N. meningitidis that is a lipoprotein presented on the surface of the bacterium. N. meningitidis strains have been sub-divided into three fHBP variant groups (referred to as variant 1 (v.1), variant 2 (v.2), and variant 3 (v.3) in some reports (Masignani et al. 2003, supra) and Family A and B in other reports (see, e.g., Fletcher et al. 2004 Infect Immun 2088-2100)) based on amino acid sequence variability and immunologic cross-reactivity (Masignani et al. J Exp Med 2003; 197:789-99). For clarity, the present disclosure uses the v.1, v.2 and v.3 terminology. Because the length of variant 2 (v.2) fHBP protein (from strain 8047) and variant 3 (v.3) fHBP (from strain M1239) differ by -1 and +7 amino acid residues, respectively, from that of MC58, the numbering used to refer to residues for v.2 and v.3 fHBP proteins differs from numbering based on the actual amino acid sequences of these proteins. Thus, for example, reference to a leucine residue (L) at position 166 of the v.2 or v.3 fHBP sequence in
Figure 3 refers to the residue at position 165 of the v.2 protein and at position 173 in the v.3 protein. For further clarification, seeFigure 4 for alignment. - The term "heterologous" refers to two components that are defined by structures derived from different sources. For example, where "heterologous" is used in the context of a chimeric polypeptide, the chimeric polypeptide includes operably linked amino acid sequences that can be derived from different polypeptides (e.g., a first component from a fHBP v.1 polypeptide and a second component from a fHBP v.2 polypeptide). Similarly, "heterologous" in the context of a polynucleotide encoding a chimeric polypeptide includes operably linked nucleic acid sequence that can be derived from different genes (e.g., a first component from a nucleic acid encoding a fHBP v.1 polypeptide and a second component from a nucleic acid encoding a fHBP v.2 polypeptide). Such chimeric polypeptides as described herein provide for presentation of epitopes in a single polypeptide that are normally found in different polypeptides. Other exemplary "heterologous" nucleic acids include expression constructs in which a nucleic acid comprising a coding sequence is operably linked to a regulatory element (e.g., a promoter) that is from a genetic origin different from that of the coding sequence (e.g., to provide for expression in a host cell of interest, which may be of different genetic origin relative to the promoter, the coding sequence or both). For example, a T7 promoter operably linked to a polynucleotide encoding a fHBP polypeptide or domain thereof is said to be a heterologous nucleic acid. "Heterologous" in the context of recombinant cells can refer to the presence of a nucleic acid (or gene product, such as a polypeptide) that is of a different genetic origin than the host cell in which it is present. For example, a Neisserial amino acid or nucleic acid sequence of one strain is heterologous to a Neisserial host of another strain.
- "Heterologous" as used herein in the context of a chimeric fHBP (e.g., "heterologous fHBP domain", e.g., a "heterologous B domain", "heterologous C domain") indicates that the chimeric fHBP protein contains operably linked and contiguous amino acid sequences of structural elements of at least two different fHBP variants (e.g., so as to provide for presentation of epitopes of a v. 1 fHBP, and presentation of a v.2 fHBP and/or a v.3 fHBP in a single fHBP polypeptide). For example, a "heterologous B domain" refers to a polypeptide which comprises a B domain that contains a first portion having a contiguous amino acid sequence of a B domain of a first fHBP variant operably linked to a second portion having a contiguous amino acid sequence of a B domain of a second fHBP variant.
- "Derived from" in the context of an amino acid sequence or polynucleotide sequence (e.g., an amino acid sequence "derived from" a v.1 fHBP) is meant to indicate that the polypeptide or nucleic acid has a sequence that is based on that of a reference polypeptide or nucleic acid (e.g., a naturally occurring fHBP protein or encoding nucleic acid), and is not meant to be limiting as to the source or method in which the protein or nucleic acid is made. "Derived from" in the context of bacterial strains is meant to indicate that a strain was obtained through passage in vivo, or in in vitro culture, of a parental strain and/or is a recombinant cell obtained by modification of a parental strain.
- "Conservative amino acid substitution" refers to a substitution of one amino acid residue for another sharing chemical and physical properties of the amino acid side chain (e.g., charge, size, hydrophobicity/hydrophilicity). "Conservative substitutions" are intended to include substitution within the following groups of amino acid residues: gly, ala; val, ile, leu; asp, glu; asn, gln; ser, thr; lys, arg; and phe, tyr. Conservative amino acid substitutions in the context of a chimeric fHBP disclosed herein are selected so as to preserve presentation of an epitope of interest. Guidance for such substitutions can be drawn from alignments of amino acid sequences of polypeptides presenting the epitope of interest.
- The term "protective immunity" means that a vaccine or immunization schedule that is administered to a mammal induces an immune response that prevents, retards the development of, or reduces the severity of a disease that is caused by Neisseria meningitidis, or diminishes or altogether eliminates the symptoms of the disease. Protective immunity can be accompanied by production of bactericidal antibodies. It should be noted that production of bactericidal antibodies against Neisseria meningitidis is accepted in the field as predictive of a vaccine's protective effect in humans. (Goldschneider et al., 1969, J. Exp. Med. 129:1307; Borrow et al. 2001 Infect Immun. 69:1568).
- The phrase "a disease caused by a strain of capsular group B of Neisseria meningitidis" encompasses any clinical symptom or combination of clinical symptoms that are present in an infection of a human with a member of capsular group B of Neisseria meningitidis. These symptoms include but are not limited to: colonization of the upper respiratory tract (e.g. mucosa of the nasopharynx and tonsils) by a pathogenic strain of capsular group B of Neisseria meningitidis, penetration of the bacteria into the mucosa and the submucosal vascular bed, septicemia, septic shock, inflammation, haemmorrhagic skin lesions, activation of fibrinolysis and of blood coagulation, organ dysfunction such as kidney, lung, and cardiac failure, adrenal hemorrhaging and muscular infarction, capillary leakage, edema, peripheral limb ischaemia, respiratory distress syndrome, pericarditis and meningitis.
- The phrase "broad spectrum protective immunity" means that a vaccine or immunization schedule elicits "protective immunity" against at least more than one strain (and can be against at least two, at least three, at least four, at least five, against at least eight, or more strains) of Neisseria meningitidis, wherein each of the strains expresses a different fHBP subvariant or fHBP variant. The present disclosure specifically contemplates and encompasses a vaccine or vaccination regimen that confers protection against a disease caused by a member of any capsular group (e.g., A, B, or C), with protection against disease caused by a capsular group B strain of Neisseria meningitidis being of interest due to the epidemiological prevalence of strains causing disease with this capsular group and lack of broadly effective group B vaccines.
- The phrase "specifically binds to an antibody" or "specifically immunoreactive with", in the context of an antigen (e.g., a polypeptide antigen) refers to a binding reaction which is based on and/or is probative of the presence of the antigen in a sample which may also include a heterogeneous population of other molecules. Thus, under designated conditions, the specified antibody or antibodies bind(s) to a particular antigen or antigens in a sample and do not bind in a significant amount to other molecules present in the sample. "Specifically binds to an antibody" or "specifically immunoreactive with" in the context of an epitope of an antigen (e.g., an epitope of a polypeptide) refers to a binding reaction which is based on and/or is probative of the presence of the epitope in an antigen (e.g., polypeptide) which may also include a heterogeneous population of other epitopes, as well as a heterogeneous population of antigens. Thus, under designated conditions, the specified antibody or antibodies bind(s) to a particular epitope of an antigen and do not bind in a significant amount to other epitopes present in the antigen and/or in the sample.
- The phrase "in a sufficient amount to elicit an immune response" means that there is a detectable difference between an immune response indicator measured before and after administration of a particular antigen preparation. Immune response indicators include but are not limited to: antibody titer or specificity, as detected by an assay such as enzyme-linked immunoassay (ELISA), bactericidal assay, flow cytometry, immunoprecipitation, Ouchter-Lowny immunodiffusion; binding detection assays of, for example, spot, Western blot or antigen arrays; cytotoxicity assays, etc.
- A "surface antigen" is an antigen that is present in a surface structure of Neisseria meningitidis (e.g. the outer membrane, inner membrane, periplasmic space, capsule, pili, etc.).
- "Isolated" refers to an entity of interest that is in an environment different from that in which the compound may naturally occur. "Isolated" is meant to include compounds that are within samples that are substantially enriched for the compound of interest and/or in which the compound of interest is partially or substantially purified."
- "Enriched" means that a sample is non-naturally manipulated (e.g., by an experimentalist or a clinician) so that a compound of interest is present in a greater concentration (e.g., at least a three-fold greater, at least 4-fold greater, at least 8-fold greater, at least 64-fold greater, or more) than the concentration of the compound in the starting sample, such as a biological sample (e.g., a sample in which the compound naturally occurs or in which it is present after administration), or in which the compound was made (e.g., as in a bacterial polypeptide, antibody, chimeric polypeptide, and the like)
- A "knock-out" or "knockout" of a target gene refers to an alteration in the sequence of the gene that results in a decrease of function of the target gene, e.g., such that target gene expression is undetectable or insignificant, and/or the gene product is not functional or not significantly functional. For example, a "knockout" of a gene involved in LPS synthesis indicates means that function of the gene has been substantially decreased so that the expression of the gene is not detectable or only present at insignificant levels and/or a biological activity of the gene product (e.g., an enzymatic activity) is significantly reduced relative to prior to the modification or is not detectable. "Knock-outs" encompass conditional knock-outs, where alteration of the target gene can occur upon, for example, exposure to a predefined set of conditions (e.g., temperature, osmolarity, exposure to substance that promotes target gene alteration, and the like. A "knock-in" or "knockin" of a target gene refers to a genetic alteration in a host cell genome that that results in an increase in a function provided by the target gene,
- Before describing further exemplary chimeric fHBPs contemplated by the present disclosure, it is helpful to describe naturally-occurring fHBP from which the chimeric fHBPs may be derived.
For convenience and clarity, the native amino acid sequence of the v.1 fHBP of the N. meningitidis strain MC58 was arbitrarily selected as a reference sequence for all native v.1, v.2, and v.3 fHBP amino acid sequences, as well as for the chimeric fHBPs described herein. Two nomenclature systems have been adopted to describe fHBP: one, which for convenience divided the protein into three domains, designated A, B and C (Giuliani et al., Infect Immun 2005; 73:1151-60), and the other based on three-dimensional structural data. In the alternative nomenclature system that describes fHBP based on three-dimensional structural data, fHBP is divided into two domains: the fHbpN and the fHbpC. Details of each of these domains with reference to the amino acid sequence of v.1 fHBP of MC58 strain is described below. - As noted above, the nomenclature based on three domains describes fHBP as having an "A domain", a "B domain", and a "C domain". The amino acid sequence of the v.1 fHBP of the MC58 strain along with the boundaries of the A, B and C domains is shown in
Fig. 21 . The Q101 and G164 residues indicated by the upward arrows denote the A/B and B/C domain boundaries, respectively. The "α" symbols indicate the position of the first and second α helices of the fHBP (referred to as AH1 and AH2). Residues GEHT are underlined followed by the second α helix (AH2) of fHBP. Panel A inFig. 34 also shows a ribbon diagram of the full length fHBP with the A, B, and C domains indicated as various shades of gray. -
Fig. 3 provides a schematic of a truncated structural model of fHBP having operably linked B and C domains (the A domain and a portion of the N-terminal portion of the B domain are not shown). The native v.1 fHBP of MC58 was again used as a reference sequence for purposes of residue numbering. Amino acid residues identified by site-directed mutagenesis of fHBP that contribute to binding of nine anti-fHBP mAbs (referred to as "JAR" mAbs) are noted. Coordinates from the solution structure of the B and C domains of fHBP from strain MC58 were used to construct the model. The α helix of the B domain is illustrated, as are the loops and β strands of the C domain. - In an alternative nomenclature system, fHBP is described as having two structural domains as opposed to the three domains described above. The two-domain nomenclature system is based on structural information of a full-length fHBP from which three-dimensional models may be constructed, such as the ones shown in
Fig. 34 . Structural modeling reveals that full-length fHBP is found to exist in solution as two separate domains connected by a linker. The amino acid sequence of the v.1 fHBP of the MC58 strain is shown inFig. 21 with end of the fHbpN domain indicated with an arrow atglycine 136. The N-terminal domain is named fHbpN (residues 8-136) and the C-terminal domain fHbpC (residues 141-255), each comprising at least 8 antiparallel β strands and joined by a native linker (residues 137-140). As seen inFig. 21 , the linker also comprises α-helix AH2 as "α" below the sequence inFig. 21 marks the positions of α helices that reside in fHBP. For purposes of simplification herein, the fHbpC domain is considered to include the linker that connects the N-terminal and C-terminal domains based on the convention of this nomenclature. - fHBP has been divided into three variant groups (referred to as variant 1 (v.1), variant 2 (v.2), and variant 3 (v.3)) based on amino acid sequence variability and immunologic cross-reactivity (Masignani et al. 2003 J Exp Med 197:789-99). In certain studies, fHBP has also been subdivided into two sub-families designated sub-family A (which includes v.2 and v.3 of Masignani et al., 2003 J Exp Med 197:789-99) and sub-family B (v.1) (Fletcher et al., 2004, Infect Immun. 72: 2088-100). "Variant" as used in the context of an "fHBP variant" refers to an fHBP that share at least 89% amino acid sequence identity with the prototype strain of that variant group (strain MC58 for v.1;
strain 2996 for v.2; and strain M1239 for v.3). These were the original prototype sequences described by Masignani et al., J. Exp. Med., 2003. Strains within a variant group encode fHBPs with greater than 88% amino acid identity, whereas strains of different fHBP variant groups range from approximately 60-88% identical. fHBPs in the same "variant" group possess greater than 88% identity to the respective prototype sequence (v.1, strain MC58; v.2,strain 2996; v.3, strain M1239). A "subvariant" as used in the context of an "fHBP subvariant" refers to fHBP polypeptides that differ from the prototype sequence. For example, strain NZ98/254 is referred to as an fHBP v. 1 subvariant, with 91% identity to the prototype sequence from strain MC58; strain RM1090 is referred to as an fHBP v.2 subvariant, with a sequence that is 94% identical to the v.2prototype strain 2996. Examples of subvariants, and their relative amino acid sequence identities, are provided inFigures 8A and8B . - fHBP polypeptides, and encoding nucleic acids, from which portions of the chimeric fHBPs of the present disclosure can be derived may be from any suitable N. meningitidis strain. As is known in the art, N. meningitidis strains are divided into serologic groups (capsular groups), serotypes (PorB phenotypes) and subtypes (PorA phenotypes) on the basis of reactions with polyclonal (Frasch, C. E. and Chapman, 1973, J. Infect. Dis. 127: 149-154) or monoclonal antibodies that interact with different surface antigens. Capsular grouping traditionally has been based on immunologically detectable variations in the capsular polysaccharide but is being replaced by PCR of genes encoding specific enzymes responsible for the biosynthesis of the structurally different capsular polysaccharides. About 12 capsular groups (including A, B, C, X, Y, Z, 29-E, and W-135) are known. Strains of the capsular groups A, B, C, Y and W-135 account for nearly all meningococcal disease. Serotyping traditionally has been based on monoclonal antibody defined antigenic differences in an outer membrane protein called Porin B (PorB). Antibodies defining about 21 serotypes are currently known (Sacchi et al., 1998, Clin. Diag. Lab. Immunol. 5:348). Serosubtyping has been based on antibody defined antigenic variations on an outer membrane protein called Porin A (PorA). Both serotyping and serosubtyping are being replaced by PCR and/or DNA sequencing for identification of genes encoding the variable regions of PorB and PorA, respectively that are associated with mAb reactivity (e.g. Sacchi, Lemos et al., supra; Urwin et al., 1998, Epidem. and Infect. 120:257).
- N. meningitidis also may be divided into clonal groups or subgroups, using various techniques that directly or indirectly characterize the bacterial genome. These techniques include multilocus enzyme electrophoresis (MLEE), based on electrophoretic mobility variation of an enzyme, which reflects the underlying polymorphisms at a particular genetic locus. By characterizing the variants of a number of such proteins, genetic "distance" between two strains can be inferred from the proportion of mismatches. Similarly, clonality between two isolates can be inferred if the two have identical patterns of electrophoretic variants at number of loci. In more recent literature, multilocus sequence typing (MLST) has superseded MLEE as the method of choice for characterizing the microorganisms. Using MLST, the genetic distance between two isolates, or clonality, is inferred from the proportion of mismatches in the DNA sequences of seven housekeeping genes in Neisseria meningitidis strains (Maiden et al., 1998, Proc. Natl. Acad. Sci. USA 95:3140).
- While N. meningitidis strains of any capsular group may be used, N. meningitidis strains of capsular group B are of particular interest as sources from which nucleic acid encoding fHBP and domains thereof are derived.
- While the specification provides the amino acid sequence of exemplary fHBPs from which the chimeric fHBP can be derived, this is not intended to be limiting. For example, the chimeric fHBP can contain amino acid sequences that are at least 80%, at least 85%, at least 90%, or at least 95% identical to an amino acid sequence of a naturally-occurring fHBP.
- Nucleic acids encoding fHBP polypeptides for use in construction of chimeric fHBPs contemplated herein are known in the art. Exemplary fHBP polypeptides are described in, for example,
WO 2004/048404 ; Masignani et al. 2003 J Exp Med 197:789-799; Fletcher et al. Infect Immun 2004 2088-2100; Welsch et al. J Immunol 2004 172:5606-5615; andWO 99/57280 - For purposes of identifying relevant amino acid sequences contemplated for use in the chimeric fHBPs disclosed herein, it should be noted that the immature fHBP protein includes a leader sequence of about 19 residues. Furthermore, when provided an amino acid sequence the ordinarily skilled person can readily envision the sequences of nucleic that can encode for, and provide for expression of, a polypeptide having such an amino acid sequence.
- In addition to the specific amino acid sequences and nucleic acid sequences provided herein, the disclosure also contemplates polypeptides and nucleic acids having sequences that are at least 80%, at least 85%, at least 90%, or at least 95% identical in sequence to such exemplary amino acid and nucleic acids. The terms "identical" or percent "identity," in the context of two or more polynucleotide sequences, or two or more amino acid sequences, refers to two or more sequences or subsequences that are the same or have a specified percentage of amino acid residues or nucleotides that are the same (e.g., at least 80%, at least 85%, at least 90%, or at least 95% identical over a specified region), when compared and aligned for maximum correspondence over a designated region, e.g., a B domain or portion thereof, e.g., a region at least about 30, 35, 40, 45, 50, 55, 60, 65 or more amino acids or nucleotides in length, and can be up to the full-length of the reference amino acid or nucleotide sequence (e.g., a full-length fHBP). The disclosure specifically contemplates both naturally-occurring polymorphisms and synthetically produced amino acid sequences and their encoding nucleic acids.
- For sequence comparison, typically one sequence acts as a reference sequence (e.g., a naturally-occurring fHBP polypeptide sequence), to which test sequences are compared. When using a sequence comparison algorithm, test and reference sequences are input into a computer program, subsequence coordinates are designated, if necessary, and sequence algorithm program parameters are designated. The sequence comparison algorithm then calculates the percent sequence identity for the test sequence(s) relative to the reference sequence, based on the designated program parameters.
- Examples of algorithms that are suitable for determining percent sequence identity are the BLAST and BLAST 2.0 algorithms, which are described in Altschul et al. (1990) J. Mol. Biol. 215: 403-410 and Altschul et al. (1977) Nucleic Acids Res. 25: 3389-3402, respectively. Software for performing BLAST analyses is publicly available through the National Center for Biotechnology Information (www.ncbi.nlm.nih.gov). Further exemplary algorithms include ClustalW (Higgins D., et al. (1994) Nucleic Acids Res 22: 4673-4680), available at www.ebi.ac.uk/Tools/clustalw/index.html.
- In one embodiment, residue positions which are not identical differ by conservative amino acid substitutions. Conservative amino acid substitutions refer to the interchangeability of residues having similar side chains. For example, a group of amino acids having aliphatic side chains is glycine, alanine, valine, leucine, and isoleucine; a group of amino acids having aliphatic-hydroxyl side chains is serine and threonine; a group of amino acids having amide-containing side chains is asparagine and glutamine; a group of amino acids having aromatic side chains is phenylalanine, tyrosine, and tryptophan; a group of amino acids having basic side chains is lysine, arginine, and histidine; and a group of amino acids having sulfur-containing side chains is cysteine and methionine..
- Sequence identity between two nucleic acids can also be described in terms of hybridization of two molecules to each other under stringent conditions. The hybridization conditions are selected following standard methods in the art (see, for example, Sambrook, et al., Molecular Cloning: A Laboratory Manual, Second Edition, (1989) Cold Spring Harbor, N.Y.). An example of stringent hybridization conditions is hybridization at 50°C or higher and 0.1 × SSC (15 mM sodium chloride/1.5 mM sodium citrate). Another example of stringent hybridization conditions is overnight incubation at 42 °C in a solution: 50 % formamide, 5 × SSC (150 mM NaCl, 15 mM trisodium citrate), 50 mM sodium phosphate (pH7.6), 5 × Denhardt's solution, 10% dextran sulfate, and 20 mg/ml denatured, sheared salmon sperm DNA, followed by washing the filters in 0.1 × SSC at about 65 °C. Stringent hybridization conditions are hybridization conditions that are at least as stringent as the above representative conditions, where conditions are considered to be at least as stringent if they are at least about 80% as stringent, typically at least 90% as stringent as the above specific stringent conditions.
- The chimeric fHBP of the present disclosure is described in more detail below in the context of both the nomenclature dividing the protein into three domains used by Giuliani et al. (Infect Immun 2005; 73:1151-60) and the three-dimensional structural nomenclature.
- As noted above, fHBP may be described as having the following three domains to facilitate analysis: A domain, B domain, and C domain. As shown in
Fig. 21 , the upward arrows at Q101 and G164 demarcate the boundaries between A/B domains and B/C domains, respectively. The chimeric fHBPs of the present disclosure optionally include an A domain. For convenience and clarity, the A domain can be structurally defined as those residues corresponding to residues 1-100 of v.1 fHBP of MC58, where the numbering is based on amino acid sequence of MC58 v.1 fHBP lacking the signal sequence (Masignani et al., 2003 J Exp Med 197:789-99) (seeFigure 21 ). As exemplified in the alignment of v.1 fHBP of MC58 and v.2 fHBP of 8047, the respective amino acid sequences of the A domains of fHBPs normally share significant amino acid sequence identity (seeFig. 8B ). Chimeric fHBPs which contain an A domain can contain a contiguous A domain amino acid sequence that is at least 85%, at least 90%, or at least 95% identical to an amino acid sequence of an A domain of a naturally occurring fHBP. The A domain may be derived from the same variant group (and may be derived from the same fHBP) as the N-terminal portion of the B domain, such that the amino acid sequence at the A/B junction is one that may be found in nature. Alternatively, the A domain amino acid sequence may be derived from a fHBP variant group different from the fHBP variant group from which the N-terminal amino acid sequence of the B domain is derived (e.g., the A domain may be derived from a v.2 fHBP and the N-terminal amino acid sequence of the B domain derived from a v.1 fHBP). - As noted above, the chimeric fHBPs of the present disclosure contain amino acid sequence of a v.1 fHBP B domain. Amino acid sequences of v.1 fHBP, including v.1 fHBP B domains, are well known in the art and can be used to derive the desired amino acid sequence of a chimeric fHBP disclosed herein.
Fig. 13 provides the amino acid sequences of an N-terminal portion of the B domain of selected v. 1 fHBPs. The alignment illustrates the position and identity of naturally occurring polymorphisms among v.1 fHBPs.Figure 8A illustrates the amino acid sequence identity between full length fHBPs of exemplary v.1, v.2 and v.3 strains, and further illustrates the presence or absence of epitopes defined by the indicated JAR mAbs.Figure 8B illustrates the amino acid sequence identity between the A, B, and C domains of exemplary v.1, v.2 and v.3 fHBPs, as well as amino acid sequence identity within the N-terminal (101-135) and C-terminal (136-164) portions of B domains. -
Fig. 21 shows the amino acid sequence of the fHBP of the v.1 strain MC58, and illustrates the position and of a full-length B domain (defined by residues 101-164 and encompassing the amino acid sequence of GEHT followed by α -helix AH2).Fig. 22 , Panel A illustrates that an N-terminal portion of the B domain of the v.1 fHBP of the MC58 strain, can encompass an amino acid sequence defined by residues corresponding to residues N-terminal of the GEHT residues and extending to the N-terminus of the B domain at a residue corresponding toresidue 101. The C-terminal portion of the B domain of the v. 1 fHBP of the MC58 strain can encompass an amino acid sequence defined by those residues corresponding to an amino acid sequence extending N-terminally fromresidue 164 of the B domain, and encompassing up to and including the amino acid sequence of GEHT. Thus, a full-length B domain is structurally defined by the residues corresponding to residues 101-164 of the v.1 of fHBP of MC58, where residues 101-135 can define an exemplary N-terminal portion of the B domain and residues 136-164 can define an exemplary C-terminal portion of the B domain, where the numbering is based on amino acid sequence of MC58 v.1 fHBP lacking the signal sequence (Masignani et al., 2003 J Exp Med 197:789-99). - As will be described below in more detail, it should be noted that in the context of chimeric fHBPs of the present disclosure having a heterologous B domain, the C-terminus of the N-terminal portion of the B domain (and thus the N-terminus of the C-terminal portion of the heterologous B domain) is defined by the position of the junction point, which can be present N-terminal or C-terminal to the amino acid sequence of GEHT, as discussed below in more detail. For example, the junction point of a heterologous B domain of a chimeric fHBP can be positioned C-terminal to a sequence corresponding to the GEHT, and thus can extend beyond a residue corresponding to residue 135.
- Exemplary chimeric fHBP include those comprising a B domain having a contiguous amino acid sequence that is at least 80%, at least 85%, at least 90%, or at least 95% identical to an N-terminal B domain amino acid sequence of a v.1 fHBP, e.g., at least 80%, at least 85%, at least 90%, or at least 95% identical to a contiguous amino acid sequence of the N-terminal B domain amino acid sequence exemplified in
Fig. 13 . Exemplary chimeric fHBP having a heterologous B domain contain at least 35, at least 40, at least 45, at least 50 residues (and in some embodiments no more than 50 residues) of a contiguous N-terminal amino acid sequence of a B domain of a v.1 fHBP. - Exemplary chimeric fHBPs of the present disclosure contain a heterologous B domain containing an N-terminal amino acid sequence derived from an N-terminal portion of a v. 1 fHBP B domain and the remaining C-terminal portion derived from the corresponding C-terminal portion of a v.2 (or v.3) fHBP B domain, followed by the contiguous amino acid sequence of a v.2 (or v.3) C domain. For convenience and clarity, the C domain can be structurally defined as those residues corresponding to residues 165-255 of v.1 fHBP of MC58, where the numbering is based on amino acid sequence of MC58 v.1 fHBP lacking the signal sequence (Masignani et al., 2003 J Exp Med 197:789-99) (see
Figure 21 ). - Amino acid sequences of v.2 and v.3 fHBP, including v.2 and v.3 fHBP B and C domains, are well known in the art and can be used to derive the desired amino acid sequence of a chimeric fHBP disclosed herein.
Fig. 14 provides the amino acid sequences of a C-terminal portion of the B domain (as exemplified by the C-terminal 25 amino acids of v.2 fHBP B domain) and the full-length C domains of selected v.2 fHBPs. The alignment illustrates the position and identity of naturally occurring polymorphisms among v.2 fHBPs. - Exemplary chimeric fHBP include those comprising a B domain containing a C-terminal amino acid sequence derived from a v.2 or v.3 B domain, usually having a contiguous amino acid sequence that is greater than or at least 85%, at least 90%, or at least 95% identical to an C-terminal B domain amino acid sequence of a v.2 or v.3 fHBP, e.g., at least 80%, at least 85%, at least 90%, or at least 95% identical to a contiguous amino acid sequence of the N-terminal B domain amino acid sequence, such as those v.2 sequences exemplified in
Fig. 14 . Where the chimeric fHBP contains a heterologous C domain, the B domain can be at least 80%, at least 85%, at least 90%, or at least 95% identical to a contiguous amino acid sequence of a full-length B domain amino acid sequence of a v. 1 fHBP. A full-length B domain of a v.1 fHBP generally is about 64 residues in length. - As discussed previously, fHBP may also be described has having two structural domains: fHbpN and fHbpC, based on an alternative nomenclature that is derived from the structure of the full-length fHBP. As shown in
Fig. 21 and panel B ofFig. 32 ,glycine 136 marks approximately the beginning of a linker between the N-terminal and the C-terminal domains, named the fHbpN and fHbpC domains, respectively. The chimeric fHBP of the present disclosure may include a full-length fHbpN domain or a partial fHbpN domain. For convenience and clarity, the fHbpN domain can be structurally defined as those residues corresponding to residues 1-136 of v.1 fHBP of MC58, where the numbering is based on amino acid sequence of MC58 v.1 fHBP lacking the signal sequence (Masignani et al., 2003 J Exp Med 197:789-99) (seeFig. 21 ). As exemplified in the alignment of v.1 fHBP of MC58 and v.2 fHBP of 8047, the respective amino acid sequences of the first 100 residues of the fHbpN domain normally share significant amino acid sequence identity (Fig. 8B ). Chimeric fHBP which contains an fHbpN domain can contain a contiguous fHbpN domain amino acid sequence that is at least 85%, at least 90%, or at least 95% identical to an amino acid sequence of an fHbpN domain of a naturally occurring fHBP. - Alternatively, the chimeric fHBP may include a partial fHbpN domain, such that an N-terminal portion of the fHbpN is truncated. The partial fHbpN domain may comprise at least 30, 40, or 50 of a contiguous C-terminal amino acid sequence of the full length fHbpN domain.
- Exemplary chimeric fHBPs include those comprising a full or partial fHbpN domain having a contiguous amino acid sequence that is at least 80%, at least 85%, at least 90%, or at least 95% identical to at least a C-terminal portion of the fHbpN amino acid sequence of a v.1 fHBP, e.g., at least 80%, at least 85%, at least 90%, or at least 95% identical to a contiguous amino acid sequence of the C-terminal fHbpN amino acid sequence exemplified in
Fig. 13 . An exemplary chimeric fHBP having heterologous domains contains at least 35, at least 40, at least 45, at least 50 residues (and in some embodiments no more than 50 residues) of a contiguous C-terminal amino acid sequence of an fHbpN domain of a v.1 fHBP. - The full or partial fHbpN domain may be derived from the same variant group (and may be derived from the same fHBP) as certain portions of the fHbpC domain. Alternatively, the fHbpN amino acid sequence may be derived from a fHBP variant group different from the fHBP variant group from which the N-terminal amino acid sequence of the fHbpC domain is derived (e.g., the fHbpC domain may be derived from a v.2 fHBP and the C-terminal amino acid sequence of the fHbpN domain derived from a v.1 fHBP).
- As noted above, the chimeric fHBPs of the present disclosure contain amino acid sequence of a v.1 fHbpN domain. Amino acid sequences of v.1 fHBP, including v.1 fHbpN domains, are well known in the art and can be used to derive the desired amino acid sequence of a chimeric fHBP disclosed herein.
Fig. 13 provides the C-terminal amino acid sequences of the fHbpN domain of selected v.1 fHBPs. The alignment illustrates the position and identity of naturally occurring polymorphisms among v.1 fHBPs.Figure 8A illustrates the amino acid sequence identity between full length fHBPs of exemplary v.1, v.2 and v.3 strains, and further illustrates the presence or absence of epitopes defined by the indicated JAR mAbs.Figure 8B illustrates the amino acid sequence identity between exemplary v.1, v.2 and v.3 fHBPs, as well as amino acid sequence identity within the C-terminal portion of the fHbpN (101-135) and N-terminal (136-164) portion of the fHbpC domains. - As will be described below in more detail, it should be noted that in the context of chimeric fHBPs of the present disclosure having heterologous domains, the position of the junction point between heterologous domains can be present within or proximal to the linker that connects the fHbpN and the fHbpC domains.
Glycine 136 defines the boundary between fHbpN and fHbpC and also marks the beginning of the linker sequence. The linker sequence corresponds approximately toresidues 136 to 149 and includes α-helix AH2. For example, the junction point between heterologous domains of a chimeric fHBP can be positioned C-terminal to a sequence corresponding to the GEHT sequence underlined inFig. 21 . In some embodiments, the junction may be no more than 20, no more than 15, no more than 5 or less amino acid residues away from the amino acid sequence of GEHT or the linker sequence. In other embodiments where heterologous domains are present in the fHbp C domain, the junction between the heterologous domains may be positioned C-terminal toglycine 164.Glycine 164 is also indicated by an arrow inFig. 21 . - Exemplary chimeric fHBPs of the present disclosure contain heterologous domains comprising a full or partial fHbpN domain of a v.1 fHBP fHbpN domain and a fHbpC domain derived from the fHbpC of a v.2 (or v.3) fHBP. For convenience and clarity, the fHbpC domain can be structurally defined as those residues corresponding to residues 141-255 of v.1 fHBP of MC58, where the numbering is based on amino acid sequence of MC58 v.1 fHBP lacking the signal sequence (Masignani et al., 2003 J Exp Med 197:789-99) (
Fig. 21 ). - Amino acid sequences of v.2 and v.3 fHBP, including v.2 and v.3 fHBP fHbpN and fHbpC domains, are well known in the art and can be used to derive the desired amino acid sequence of a chimeric fHBP disclosed herein.
Fig. 14 provides the amino acid sequences of the full-length fHbpC domains of selected v.2 fHBPs. The alignment illustrates the position and identity of naturally occurring polymorphisms among v.2 fHBPs. Exemplary chimeric fHBPs include those comprising an fHbpC amino acid sequence derived from a v.2 or v.3 fHbpC domain, usually having a contiguous amino acid sequence that is greater than or at least 85%, at least 90%, or at least 95% identical to the amino acid sequence of the fHbpC domain of a v.2 or v.3 fHBP, e.g., at least 80%, at least 85%, at least 90%, or at least 95% identical to a contiguous amino acid sequence of the fHbpC domain amino acid sequence, such as those v.2 sequences exemplified inFig. 14 . - In certain cases, instead of having the amino acid sequence of fHbpN derived from one variant and that of fHbpC derived from a different variant, fHbpC domain may contain two contiguous amino acid sequences derived from different variants. In cases where fHbpC contains heterologous sequences, a contiguous N-terminal amino acid sequence of fHbpC can be at least 80%, at least 85%, at least 90%, or at least 95% identical to a contiguous amino acid sequence of the corresponding amino acid sequence of a v.1 fHBP.
- As explained previously, fHBP may be described in the context of the three domains assigned by Giuliani et al (Infect Immun 2005; 73:1151-60) or in the context of two three-dimensional structural domains. For the sake of brevity, the disclosure will adopt the nomenclature of the three domains, designated A, B, and C domains. However, all discussion in the context of the three functional domains can be readily understood in the context of the two structural domains based on what has been detailed above.
- As set out above, the chimeric fHBPs of the present disclosure generally include either a heterologous B domain and a C domain; or a B domain and a heterologous C domain. Such chimeric fHBPs are constructed so as to contain epitopes that elicit bactericidal antibodies effective against N. meningitidis strains producing more than one fHBP variant.
- The term "chimeric factor H binding protein" or "chimeric fHBP" refers to a polypeptide comprising, from N-terminus to C-terminus, an amino acid sequence of a B domain and of a C domain, wherein at least one of the B domain and the C domain contains a heterologous amino acid sequence characterized as having an N-terminal portion derived from a contiguous amino acid sequence of a v.1 fHBP with the remaining B and C-terminal portion (or C terminal portion) being derived from a contiguous amino acid sequence of a v.2 or v.3 fHBP. The B domain and/or C domain amino acid sequences are generally derived from a contiguous amino acid sequence of a naturally-occurring fHBP and mutants thereof that maintain or introduce desired epitopes. Chimeric fHBP can optionally include an amino acid sequence of an fHBP A domain operably linked and N-terminal to the B domain. Chimeric fHBP can further optionally include a leader sequence, e.g., to provide for expression of the chimeric fHBP on a cell surface of a bacterial host cell.
- Where the chimeric fHBP contains a heterologous B domain, the heterologous B domain generally comprises at least an N-terminal portion derived from a contiguous amino acid sequence of a v.1 fHBP B domain and a C-terminal portion derived from a contiguous amino acid sequence of a v.2 or v.3 B domain, with the heterologous B domain being operably linked to a C domain derived from a contiguous amino acid sequence of a v.2 or v.3 fHBP C domain. Thus, for example, such chimeric fHBP can be described as having a heterologous B domain composed of an N-terminal portion for which a corresponding contiguous amino acid sequence of a v.1 fHBP B domain sequence serves as a scaffold, and a C-terminal portion for which a corresponding contiguous amino acid sequence of a v.2 or v.3 fHBP B domain sequence serves as a scaffold.
- As noted above, exemplary chimeric fHBP having a heterologous B domain contain at least 35, at least 40, at least 45, at least 50 residues (and in some embodiments no more than 50 residues) of a contiguous N-terminal amino acid sequence of a B domain of a v.1 fHBP.
- Where the chimeric fHBP contains a heterologous C domain, the B domain of the chimeric fHBP comprises a contiguous amino acid sequence of a v.1 fHBP B domain operably linked to heterologous C domain comprising at least an N-terminal portion of a v. 1 fHBP C domain and a C-terminal portion of a v.2 or v.3 C domain. Exemplary chimeric fHBP of this embodiment contain 2, 4, 6, 8 residues of an N-terminal sequence of a v.1 C domain, with the remainder of the C domain being derived from a v.2 or v.3 C domain amino acid sequence.
- Chimeric fHBP contemplated by the present disclosure include those having an amino acid sequence corresponding to a full-length B domain and a full-length C domain, and, optionally, a full-length A domain wherein the chimeric fHBP includes at least a heterologous B domain or a heterologous C domain. Other embodiments include chimeric fHBP having an amino acid sequence corresponding to a fragment of an A domain composed of a contiguous amino acid sequence encompassing amino acid defining an epitope bound by the
JAR 4 mAb. Further embodiments include chimeric fHBP in which the C domain is truncated at the C-terminus, with the proviso that epitopes of interest (e.g., one or more of the epitopes bound bymAbs JAR 10,JAR 11,JAR 33,JAR 32/35, and JAR 13) are preserved so as to retain the ability to elicit antibodies that bind these epitopes. Chimeric fHBP also include those that lack an A domain, and have an N-terminally truncated B domain, with the proviso that the truncated B domain maintains expression of an epitope(s) of interest. Chimeric fHBP include those having a B domain that expresses an epitope bound by theJAR 5 mAb. - Chimeric polypeptides described herein can include additional heterologous amino acid sequences, e.g., to provide an N-terminal methionine or derivative thereof (e.g., pyroglutamate) as a result of expression in a bacterial host cell (e.g., E. coli) and/or to provide a chimeric polypeptide having a fusion partner at its N-terminus or C-terminus. Fusion partners of interest include, for example, glutathione-S-transferase (GST), maltose binding protein (MBP), His6-tag, and the like, as well as leader peptides from other proteins, particularly lipoproteins. Fusion partners can provide for additional features, such as in facilitating isolation and purification of the chimeric polypeptide.
- Native fHBP usually contains an N-terminal cysteine to which a lipid moiety can be covalently attached. This cysteine residue is usually lipidated in the naturally-occurring protein, and can be lipidated in the chimeric fHBPs disclosed herein. Thus, in the amino acid sequences described herein (including those presented in any Sequence Listing), reference to "cysteine" or "C" at this position specifically includes reference to both an unmodified cysteine as well as to a cysteine that is lipidated (e.g., due to post-translational modification). Thus, the chimeric fHBP can be lipidated or non-lipidated. Methods for production of lipidated proteins in vitro, (see, e.g., Andersson et al., 2001 J. Immunological Methods 255(1-2):135-48) or in vivo are known in the art. For example, lipidated fHBP previously has been purified from the membrane fraction of E. coli protein by detergent extraction (Fletcher et al., 2004 Infection and Immunity 72(4):2088-100), which method may be adapted for the production of lipidated chimeric fHBP. Lipidated proteins may be of interest as such can be more immunogenic than soluble protein (see, e.g., Fletcher et al., 2004 Infection and Immunity 72(4):2088-100).
- Exemplary chimeric fHBPs are described in detail below.
- The chimeric fHBPs of the present disclosure encompass those that can be described in terms of one or more of, for example, the site at which heterologous sequences are joined within the chimeric fHBP (i.e., the "junction point"), the presence of epitopes specifically bound by a mAb, amino acid sequence, or any combination of such features that may be present in exemplary fHBPs.
- In general, the junction point of the chimeric fHBP is the point at which amino acid sequence of the chimeric fHBP shifts from being derived from a contiguous amino acid sequence of a v.1 fHBP to being derived from contiguous amino acid sequence of a v.2 or v.3 fHBP. The junction point thus provides for an amino acid sequence that is heterologous, i.e., derived from different fHBPs. The N-terminal portion and the C-terminal portions of a heterologous domain (i.e., heterologous B domain or heterologous C domain) of chimeric fHBP are joined at a junction point, with the junction point thus defining the length of the N-terminal and C-terminal portions of the chimeric domain that are derived from a v. 1 or v.2/v.3 amino acid sequence.
- In general, a B domain amino acid sequence comprising an amino acid sequence N-terminal to the second α helix of fHBP, which includes residues corresponding to those implicated in defining the
JAR 5 mAb epitope (i.e., residues at positions 121 and 122 of a B domain v.1 fHBP MC58, which are glycine and lysine, respectively) is denoted as the "N-terminal portion of the B domain" (see, e.g.,Fig. 13 ,Fig. 21 andFig. 22 , Panel A). The amino acid sequence flanking and C-terminal to the N-terminal portion of the B domain is the "C-terminal (or distal) portion of the B domain" and is derived from a contiguous amino acid sequence of a v.2 or v.3 fHBP (Fig. 14 andFig. 22 ). Together, the N-terminal and C-terminal portions of the B domain compose a heterologous B domain of a chimeric fHBP of the present disclosure. - Where the chimeric fHBP has a heterologous B domain, the junction point may be positioned at a residue adjacent to the second α helix (AH2) (e.g., adjacent and C-terminal to a residue corresponding to residue 121 or 122 of
Figure 21 , e.g., adjacent and C-terminal to one of the residues of GEHTSFDK, e.g., adjacent and C-terminal to one of the residues of GEHT, N-terminal to AH2), or at a position C-terminal to AH2. - In one embodiment, the junction point of the heterologous B domain can be positioned at any site corresponding to a site after the glycine residue or after the lysine residue, that define a
JAR 5 monoclonal antibody (mAb) epitope of a v. 1 fHBP (which residue is positioned within the B domain, i.e., at G121 or K122 of v.1 fHBP strain MC58 reference sequence) but before a residue corresponding to a residue defining aJAR 11 mAb epitope of a v.2 fHBP (which residue is positioned in the C domain, i.e., A174 of v.2fHBP strain 8047 reference sequence). In a related embodiment, the heterologous B domain is provided such that theJAR 5 mAb epitope, theJAR 11 epitope, or both theJAR 5 andJAR 11 epitopes are maintained such that the chimeric fHBP is specifically bound by the respective mAb. - In one embodiment, the junction point is positioned so that the chimeric fHBP contains a heterologous B domain, which has an N-terminal portion composed of a contiguous amino acid sequence of an N-terminal portion of a B domain of a v. 1 fHBP containing a
JAR 5 epitope (defined in part by G121 of v.1 fHBP strain MC58) with the remaining portion (i.e., the C-terminal portion) of the B domain derived from a contiguous amino acid sequence of the corresponding C-terminal portion of a v.2 or v.3 fHBP B domain. The heterologous B domain is operably linked to a C domain derived from a contiguous amino acid sequence of a v.2 or v.3 fHBP, which can be the same or different v.2 or v.3 fHBP as that from which the C-terminal portion of the B domain is derived. - Exemplary heterologous B domains include those at least 80% identical, at least 85% identical, at least 90% identical, at least 99% identical or more to a contiguous amino acid sequence of a v.1 fHBP corresponding to residues 101-121, 101-122, 101-123, 101-124, 101-125, 101-126, 101-127, 101-128, 101-129, 101-130, 101-131, 101-132, 101-133, 101-134, 101-134, 101-136, 101-137, 101-138, or 101-139 of a v.1 fHBP amino acid sequence, where the numbering is based on MC58 fHBP as a reference. Such heterologous B domains include those having an amino acid sequence that is at least 80% identical, at least 85% identical, at least 90% identical, at least 99% identical or more to a contiguous amino acid sequence of a v.2 or v.3 fHBP so as to provide the remainder of the heterologous B domain having a C-terminus corresponding to residue 164 (again, using MC58 fHBP as a reference sequence of purposes of numbering).
- For example, where the heterologous B domain includes residues 101-122 or a v.1 fHBP, the C-terminal portion of the heterologous B domain includes residues 123-164 of a v.2 or v.3 fHBP. Accordingly, the C-terminal portion of the heterologous B domain can include an amino acid sequence at least 80% identical, at least 85% identical, at least 90% identical, at least 99% identical or more to a contiguous amino acid sequence of a v.2 or v.3 fHBP corresponding to residues 122-164, 123-164, 124-164, 125-164, 126-164,127-164, 128-164, 129-164, 130-164, 131-164, 132-164, 133-164, 134-164, 135-164, 136-164, 137-164, 139-164, or 140-164, where the N-terminal portion of the heterologous B domain is provided by the v.1 sequences exemplified above.
- In another embodiment, the junction point is positioned N-terminal to the second α helix (AH2), which are denoted in
Figure 22 by "α". As pointed out above, the residues GEHT are highly conserved across v.1, v.2, and v.3 fHBP variants, and thus can serve as convenient junction point residues, as well as a convenient reference for the position of a junction point in a chimeric fHBP. For example, the junction point can be positioned within 14, 13, 12, 11, 10, 9, 8, 7, 6, 5, 4, 3, 2, or 1 residue(s) N-terminal to GEHT to provide a heterologous B domain (e.g., positioned at a site not more than 14, 13, 12, 11, 10, 9, 8, 7, 6, 5, 4, 3, 2, or 1 residue N-terminal of GEHT); or is positioned within 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33 or 34 residues C-terminal to GEHT (e.g., positioned at a site not more than 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33 or 34 residues C-terminal of GEHT), where a junction point at a site less than or equal to 26 residues C-terminal to GEHT provides a heterologous B domain and a junction point positioned at more than 26 residues C-terminal to GEHT produces a chimeric fHBP having a heterologous C domain. - For example, the junction point of the heterologous B domain can be selected such that the heterologous B domain amino acid sequence positioned N-terminal and flanking the amino acid sequence GEHT is derived from a v.1 fHBP B domain amino acid sequence and the heterologous B domain amino acid sequence positioned C-terminal and flanking the GEHT is derived from a v.2 or v.3 fHBP B amino acid sequence.
- In some embodiments, the junction point is positioned so as to provide a heterologous B domain comprising an amino acid sequence that is greater than 80% (e.g., at least 81%), at least 85%, at least 90%, at least 95% or identical to an amino acid sequence of
- QSHSALTAFQ TEQIQDSEHS GK (SEQ ID NO: 1) where the amino acid sequence optionally provides for an epitope that mediates specific binding of a
JAR 5 mAb. Exemplary amino acid substitutions of the above sequence are as follows: QSHSALTA(F/L)Q TEQ(I/V/E)QD(S/P)E(H/D)S (G/E/R)K. - Exemplary modifications of the amino acid sequences of the heterologous B domain as set out above include, for example, one or more of the following substitutions of SEQ ID NO: 1 as follows:
- leucine (L) for the phenylalanine (F) at a residue corresponding to
position 9; - valine (V) or glutamic acid (E) for isoleucine (I) at
residue position 14; - proline (P) for serine (S) at residue position 17;
- aspartic acid (D) for histidine (H) at residue position 19;
- arginine (R) for glutamine (Q) at
residue position 28; - valine (V) for alanine (A) at
residue position 35; - glycine (G) for aspartic acid (D) at
residue position 42; or - lysine (K) for glutamic acid (E) at
residue position 46. -
- In some embodiments, the junction point is positioned so as to provide a heterologous B domain comprising an amino acid sequence that is at least 80%, at least 85%, at least 90%, at least 95% or identical to an amino acid sequence of
TEQIQDSEHS GKMVAKRQFR IGDIAGEHTA FNQLPD,
where the amino acid sequence optionally provides for an epitope that mediates specific binding of aJAR 5 mAb. - In other embodiments the heterologous B domain comprises an amino acid sequence that is at least 80%, at least 85%, at least 90%, at least 95% or identical to an amino acid sequence of
QSHSALTAFQ TEQIQDSEHS GKMVAKRQFR IGDIAGEHTA FNQLPD
where the amino acid sequence optionally provides for an epitope specifically bound byJAR 5 MAB. - In still other embodiments, the heterologous B domain comprises a sequence at least 80%, at least 85%, at least 90%, at least 95% or identical to an amino acid sequence set out in
Fig. 13 , which provides an alignment of exemplary chimeric fHBPs III, IV and V sequences in the region of the junction point, which is indicated by the box. The residue, G121, implicated in theJAR 5 epitope is shown in bold and underlined. - In some embodiments, the junction point is positioned so as to provide a heterologous B domain comprising an amino acid sequence that is at least 80%, at least 85%, at least 90%, at least 95% or identical to an amino acid sequence of:
LTAFQ TEQIQDSEHS GKMVAKRQFR IGDIA
where the amino acid sequence optionally provides for an epitope that mediates specific binding of aJAR 5 mAb. - In another embodiment, the junction point of the chimeric fHBP is positioned so that the chimeric fHBP contains a heterologous C domain composed of a contiguous amino acid sequence of an N-terminal portion of a C domain of a v. 1 fHBP and a contiguous amino acid sequence of a C-terminal portion of a C domain of a v.2 or v.3 fHBP.
- For example, the junction point of a chimeric fHBP having a heterologous C domain can be in the loop regions of the β-barrel of the C domain, or in any highly conserved segment, for example at residues D160 or I170. In one embodiment, the heterologous C domain includes an N-terminal sequence of KLTYTIDFA.
- Exemplary chimeric fHBP are provided in the Examples below. The present disclosure contemplates these exemplary chimeric fHBP, as well as chimeric fHBP having at least 85%, at least 90%, at least 95% or greater amino acid sequence identity to the amino acid sequences of these exemplary chimeric fHBP (e.g., Chimera I, Chimera II, Chimera IIb, Chimera III, Chimera IV, and Chimera V). The amino acid and nucleic acid sequences encoding Chimera I, Chimera II, Chimera IIb, Chimera III, Chimera IV, and Chimera V are provided in
Figures 23, 24 ,25, 26 ,27, and 28 , respectively. The asterisk denotes the C-terminus of the amino acid sequence (corresponding to the stop codon of the encoding nucleic acid). - Chimeric fHBP encompass chimeric fHBP that contain pairs of epitopes that elicit antibodies that, when both are bound to their respective epitopes, exhibit enhanced bactericidal activity against N. meningitidis than when either one is bound alone. Chimeric fHBP can be designed so as to ensure that such epitopes are maintained or to introduce such epitopes (e.g., by modification of an fHBP amino acid sequence to include a pair of epitopes heterologous to that fHBP amino acid sequence).
- In general (and subject to the exception below), the distance between epitopes of such epitope pairs is selected so as to be less than 27 Ǻ but more than 14 Ǻ, and are usually located within a distance of about 18 Ǻ - 20 Ǻ. As discussed in the Examples below, a greater bactericidal effect was observed when two antibodies bound epitopes located at distances within these parameters. Without being held to theory, when bound by their respective antibodies, the distance between the epitopes is sufficient to facilitate interaction of the antibodies with factors of the complement cascade, but not so close as to result in inhibition of binding due to steric hindrance. Chimeric fHBP containing such epitopes for v.2 and v.3 strains can thus provide for production of antibodies having greater bactericidal activity against such strains. Examples of such epitope pairs are those epitopes bound by
JAR 10 and JAR 11 (fHBP v.2); and byJAR 33 andJAR 32/ 35 (JAR 32 andJAR 35 bind to the same or overlapping epitopes) (fHBP v.3). - Chimeric fHBPs can also include epitope pairs where one epitope of the pair is defined by binding by the
mAb JAR 4 and the second epitope is bound by an antibody that inhibits fH binding. Such an epitope pair is not necessarily subject to the constraints on distance between the epitopes as discussed above, with the proviso that the epitopes are not so close as to inhibit binding of their respective antibodies. As discussed in the Examples below, binding of an antibody that inhibits fH binding can be bactericidal along with another mAb that does not inhibit fH binding. For example, a mAb pair such asJAR 4 along with any anti-v.1 or v.2 mAb that blocks fH binding can provide for production of antibodies that have enhanced bactericidal activity. - Chimeric fHBPs can be designed so as to include an epitope(s) that elicits antibodies that, when bound to fHBP, inhibit fH binding. For example, as set out below, when the epitopes bound by JAR 13 (v.2 epitope), JAR 11 (v.2 epitope), and
JAR 32/35 (v.3 epitope) are bound by antibody, binding of fHBP to fH is inhibited. Thus, the presence of such fH-binding epitopes in the chimeric fHBP polypeptides can provide for production of antibodies that can facilitate protection through this pathway. - The chimeric fHBP can be generated using recombinant techniques to manipulate nucleic acids of different fHBPs known in the art to provide constructs encoding a chimeric fHBP of interest. As noted above, nucleic acids encoding a variety of different v.1, v.2, and v.3 fHBPs of N. meningitidis are available in the art, and their nucleotide sequences are known.
- Amino acid and nucleic acid sequences of exemplary chimeric fHBPs are provided in
Figures 23-28 . It will be appreciated that the nucleotide sequences encoding the chimeric fHBPs can be modified so as to optimize the codon usage to facilitate expression in a host cell of interest (e.g., E. coli, N. meningitidis, human (as in the case of a DNA-based vaccine), and the like). Methods for production of codon optimized sequences are known in the art. - Chimeric fHBPs can be produced by any suitable method, including recombinant and non-recombinant methods (e.g., chemical synthesis). Where the chimeric fHBP is produced using recombinant techniques, the methods can involve any suitable construct and any suitable host cell, which can be a prokaryotic or eukaryotic cell, usually a bacterial or yeast host cell, more usually a bacterial cell. Methods for introduction of genetic material into host cells include, for example, transformation, electroporation, conjugation, calcium phosphate methods and the like. The method for transfer can be selected so as to provide for stable expression of the introduced chimeric fHBP -encoding nucleic acid. The chimeric fHBP -encoding nucleic acid can be provided as an inheritable episomal element (e.g., plasmid) or can be genomically integrated.
- Suitable vectors for transferring chimeric fHBP-encoding nucleic acid can vary in composition. Integrative vectors can be conditionally replicative or suicide plasmids, bacteriophages, and the like. The constructs can include various elements, including for example, promoters, selectable genetic markers (e.g., genes conferring resistance to antibiotics (for instance kanamycin, erythromycin, chloramphenicol, or gentamycin)), origin of replication (to promote replication in a host cell, e.g., a bacterial host cell), and the like. The choice of vector will depend upon a variety of factors such as the type of cell in which propagation is desired and the purpose of propagation. Certain vectors are useful for amplifying and making large amounts of the desired DNA sequence. Other vectors are suitable for expression in cells in culture. Still other vectors are suitable for transfer and expression in cells in a whole animal. The choice of appropriate vector is well within the skill of the art. Many such vectors are available commercially.
- In one embodiment, the vector is an expression vector based on episomal plasmids containing selectable drug resistance markers and elements that provide for autonomous replication in different host cells (e.g., in both E. coli and N. meningitidis). One example of such a "shuttle vector" is the plasmid pFP10 (Pagotto et al. Gene 2000 244:13-19).
- Constructs can be prepared by, for example, inserting a polynucleotide of interest into a construct backbone, typically by means of DNA ligase attachment to a cleaved restriction enzyme site in the vector. Alternatively, the desired nucleotide sequence can be inserted by homologous recombination or site-specific recombination. Typically homologous recombination is accomplished by attaching regions of homology to the vector on the flanks of the desired nucleotide sequence, while site-specific recombination can be accomplished through use of sequences that facilitate site-specific recombination (e.g., cre-lox, att sites, etc.). Nucleic acid containing such sequences can be added by, for example, ligation of oligonucleotides, or by polymerase chain reaction using primers comprising both the region of homology and a portion of the desired nucleotide sequence.
- Vectors can provide for extrachromosomal maintenance in a host cell or can provide for integration into the host cell genome. Vectors are amply described in numerous publications well known to those in the art, including, e.g., Short Protocols in Molecular Biology, (1999) F. Ausubel, et al., eds., Wiley & Sons. Vectors may provide for expression of the nucleic acids encoding a chimeric fHBP, may provide for propagating the subject nucleic acids, or both.
- Exemplary vectors that may be used include but are not limited to those derived from recombinant bacteriophage DNA, plasmid DNA or cosmid DNA. For example, plasmid vectors such as pBR322, pUC 19/18, pUC 118, 119 and the M13 mp series of vectors may be used. pET21 is also an expression vector that may be used. Bacteriophage vectors may include λgt10, λgt11, λgt18-23, λZAP/R and the EMBL series of bacteriophage vectors. Further vectors that may be utilized include, but are not limited to, pJB8,
pCV 103, pCV 107, pCV 108, pTM, pMCS, pNNL, pHSG274, COS202, COS203, pWE15, pWE16 and thecharomid 9 series of vectors. - For expression of a chimeric fHBP of interest, an expression cassette may be employed. Thus, the present disclosure provides a recombinant expression vector comprising a subject nucleic acid. The expression vector provides transcriptional and translational regulatory sequences, and may provide for inducible or constitutive expression, where the coding region is operably linked under the transcriptional control of the transcriptional initiation region, and a transcriptional and translational termination region. These control regions may be native to an fHBP from which the chimeric fHBP is derived, or may be derived from exogenous sources. In general, the transcriptional and translational regulatory sequences may include, but are not limited to, promoter sequences, ribosomal binding sites, transcriptional start and stop sequences, translational start and stop sequences, and enhancer or activator sequences. Promoters can be either constitutive or inducible, and can be a strong constitutive promoter (e.g., T7, and the like).
- Expression vectors generally have convenient restriction sites located near the promoter sequence to provide for the insertion of nucleic acid sequences encoding proteins of interest. A selectable marker operative in the expression host may be present to facilitate selection of cells containing the vector. In addition, the expression construct may include additional elements. For example, the expression vector may have one or two replication systems, thus allowing it to be maintained in organisms, for example in mammalian or insect cells for expression and in a procaryotic host for cloning and amplification. In addition the expression construct may contain a selectable marker gene to allow the selection of transformed host cells. Selection genes are well known in the art and will vary with the host cell used.
- It should be noted that chimeric fHBP of the present disclosure may comprise additional elements, such as a detectable label, e.g., a radioactive label, a fluorescent label, a biotin label, an immunologically detectable label (e.g., an HA tag, a poly-Histidine tag) and the like. Additional elements of chimeric fHBP can be provided to facilitate isolation (e.g., biotin tag, immunologically detectable tag) through various methods (e.g., affinity capture, etc.). Chimeric fHBP can optionally be immobilized on a support through covalent or noncovalent attachment.
- Isolation and purification of chimeric fHBP can be accomplished according to methods known in the art. For example, chimeric fHBP can be isolated from a lysate of cells genetically modified to express a chimeric fHBP, or from a synthetic reaction mix, by immunoaffinity purification, which generally involves contacting the sample with an anti-chimeric fHBP antibody (e.g., an anti-chimeric fHBP mAb, such as a
JAR 5 mAb or other appropriate JAR mAb described herein), washing to remove non-specifically bound material, and eluting specifically bound chimeric fHBP. Isolated chimeric fHBP can be further purified by dialysis and other methods normally employed in protein purification methods. In one embodiment, the chimeric fHBP can be isolated using metal chelate chromatography methods. - Any of a number of suitable host cells can be used in the production of chimeric fHBP. In general, the chimeric fHBP described herein may be expressed in prokaryotes or eukaryotes, usually bacteria, more usually E. coli or Neisseria (e.g., N. meningitidis) in accordance with conventional techniques. Thus, the present disclosure further provides a genetically modified host cell, which contains a nucleic acid encoding a chimeric fHBP. Host cells for production (including large scale production) of a chimeric fHBP can be selected from any of a variety of available host cells. Exemplary host cells for expression include those of a prokaryotic or eukaryotic unicellular organism, such as bacteria (e.g., Escherichia coli strains), yeast (e.g., S. cerevisiae, Pichia spp., and the like)., and may include host cells originally derived from a higher organism such as insects, vertebrates, particularly mammals, (e.g. CHO, HEK, and the like). Generally bacterial host cells and yeast are of particular interest for chimeric fHBP production.
- Chimeric fHBPs can be prepared in substantially pure or substantially isolated form (i.e., substantially free from other Neisserial or host cell polypeptides) or substantially isolated form. In certain embodiments, the chimeric fHBP is present in a composition that is enriched for the polypeptide relative to other components that may be present (e.g., other polypeptides or other host cell components). Purified chimeric fHBP can be provided such that the polypeptide is present in a composition that is substantially free of other expressed polypeptides, e.g., less than 90%, usually less than 60% and more usually less than 50% of the composition is made up of other expressed polypeptides.
- Where a chimeric fHBP is to be provided in a membrane vesicle (as discussed in more detail below), a Neisserial host cell is genetically modified to express a chimeric fHBP. Any of a variety of Neisseria spp. strains can be modified to produce a chimeric fHBP, and, optionally, which produce or can be modified to produce other antigens of interest, such as PorA, can be used in the methods disclosed herein.
- Methods and vectors to provide for genetic modification of Neisserial strains and expression of a desired polypeptide are known in the art. Exemplary vectors and methods are provided in
WO 02/09746 - Pathogenic Neisseria spp. or strains derived from pathogenic Neisseria spp., particularly strains pathogenic for humans or derived from strains pathogenic or commensal for humans, are of particular interest for use in membrane vesicle production. Exemplary Neisserial spp. include N. meningitidis, N. flavescens, N. gonorrhoeae, N. lactamica, N. polysaccharea, N. cinerea, N. mucosa, N. subflava, N. sicca, N. elongata, and the like.
- N. meningitidis strains are of particular interest for genetic modification to express a chimeric fHBP and for use in vesicle production. The strain used for vesicle production can be selected according to a number of different characteristics that may be desired. For example, the strain may be selected according to: a desired PorA type (a "serosubtype", as described above), capsular group, serotype, and the like; decreased capsular polysaccharide production; and the like. For example, the production strain can produce any desired PorA polypeptide, and may express one or more PorA polypeptides (either naturally or due to genetic engineering). Exemplary strains includes those that produce a PorA polypeptide which confers a serosubtype of P1.7,16; P1.19,15; P1.7,1; P1.5,2; P1.22a,14; P1.14; P1.5,10; P1.7,4; P1.12,13; as well as variants of such PorA polypeptides which may or may not retain reactivity with conventional serologic reagents used in serosubtyping. Also of interest are PorA polypeptides characterized according to PorA variable region (VR) typing (see, e.g., Russell et al. Emerging Infect Dis 2004 10:674-678; Sacchi CT, et al, Clin Diagn Lab Immunol 1998;5:845-55; Sacchi et al, J. Infect Dis 2000;182:1169-1176). A substantial number of distinct VR types have been identified, which can be classified into VR1 and VR2 family "prototypes". A web-accessible database describing this nomenclature and its relationship to previous typing schemes is found at neisseria.org/nm/typing/pora. Alignments of exemplary PorA VR1 and VR2 types is provided in Russell et al. Emerging Infect Dis 2004 10:674-678.
- Alternatively or in addition, the production strain can be a capsule deficient strain. Capsule deficient strains can provide vesicle-based vaccines that provide for a reduced risk of eliciting a significant autoantibody response in a subject to whom the vaccine is administered (e.g., due to production of antibodies that cross-react with sialic acid on host cell surfaces). "Capsule deficient" or "deficient in capsular polysaccharide" as used herein refers to a level of capsular polysaccharide on the bacterial surface that is lower than that of a naturally-occurring strain or, where the strain is genetically modified, is lower than that of a parental strain from which the capsule deficient strain is derived. A capsule deficient strain includes strains that are decreased in surface capsular polysaccharide production by at least 10%, 20%, 25%, 30%, 40%, 50%, 60%, 75%, 80%, 85%, 90% or more, and includes strains in which capsular polysaccharide is not detectable on the bacterial surface (e.g., by whole cell ELISA using an anti-capsular polysaccharide antibody).
- Capsule deficient strains include those that are capsule deficient due to a naturally-occurring or recombinantly-generated genetic modification. Naturally-occurring capsule deficient strains (see, e.g., Dolan-Livengood et al. J. Infect. Dis. (2003) 187(10):1616-28), as well as methods of identifying and/or generating capsule-deficient strains (see, e.g., Fisseha et al. (2005) Infect. Immun. 73(7):4070-4080; Stephens et al. (1991) Infect Immun 59(11):4097-102; Frosch et al. (1990) Mol Microbiol. 1990 4(7):1215-1218) are known in the art.
- Modification of a Neisserial host cell to provide for decreased production of capsular polysaccharide may include modification of one or more genes involved in capsule synthesis, where the modification provides for, for example, decreased levels of capsular polysaccharide relative to a parent cell prior to modification. Such genetic modifications can include changes in nucleotide and/or amino acid sequences in one or more capsule biosynthesis genes rendering the strain capsule deficient (e.g., due to one or more insertions, deletions, substitutions, and the like in one or more capsule biosynthesis genes). Capsule deficient strains can lack or be non-functional for one or more capsule genes.
- Of particular interest are strains that are deficient in sialic acid biosynthesis. Such strains can provide for production of vesicles that have reduced risk of eliciting anti-sialic acid antibodies that cross-react with human sialic acid antigens, and can further provide for improved manufacturing safety. Strains having a defect in sialic acid biosynthesis (due to either a naturally occurring modification or an engineered modification) can be defective in any of a number of different genes in the sialic acid biosynthetic pathway. Of particular interest are strains that are defective in a gene product encoded by the N-acetylglucosamine-6-phosphate 2-epimerase gene (known as synX AAF40537.1 or siaA AAA20475), with strains having this gene inactivated being of especial interest. For example, in one embodiment, a capsule deficient strain is generated by disrupting production of a functional synX gene product (see, e.g., Swartley et al. (1994) J Bacteriol. 176(5):1530-4).
- Capsule-deficient strains can also be generated from naturally-occurring strains using non-recombinant techniques, e.g., by use of bactericidal anti-capsular antibodies to select for strains that reduced in capsular polysaccharide.
- Where the disclosure involves use of two or more strains (e.g., to produce antigenic compositions containing a chimeric fHBP-presenting vesicles from different strains), the strains can be selected so as to differ in one or more strain characteristics, e.g., to provide for vesicles that differ in the chimeric fHBP used, PorA, and the like.
- The antigenic compositions contemplated by the present disclosure generally include vesicles prepared from Neisserial cells that express a chimeric fHBP. As referred to herein "vesicles" is meant to encompass outer membrane vesicles as well as microvesicles (which are also referred to as blebs).
- In one embodiment, the antigenic composition comprises outer membrane vesicles (OMV) prepared from the outer membrane of a cultured strain of Neisseria meningitidis spp. genetically modified to express a chimeric fHBP. OMVs may be obtained from Neisseria meningitidis grown in broth or solid medium culture, preferably by separating the bacterial cells from the culture medium (e.g. by filtration or by a low-speed centrifugation that pellets the cells, or the like), lysing the cells (e.g. by addition of detergent, osmotic shock, sonication, cavitation, homogenization, or the like) and separating an outer membrane fraction from cytoplasmic molecules (e.g. by filtration; or by differential precipitation or aggregation of outer membranes and/or outer membrane vesicles, or by affinity separation methods using ligands that specifically recognize outer membrane molecules; or by a high-speed centrifugation that pellets outer membranes and/or outer membrane vesicles, or the like); outer membrane fractions may be used to produce OMVs.
- In another embodiment, the antigenic composition comprises microvesicles (MV) (or "blebs") containing chimeric fHBP, where the MV or blebs are released during culture of a Neisseria meningitidis strain genetically modified to express a chimeric fHBP. For example, MVs may be obtained by culturing a strain of Neisseria meningitidis in broth culture medium, separating whole cells from the broth culture medium (e.g. by filtration, or by a low-speed centrifugation that pellets only the cells and not the smaller blebs, or the like), and then collecting the MVs that are present in the cell-free culture medium (e.g. by filtration, differential precipitation or aggregation of MVs, or by a high-speed centrifugation that pellets the blebs, or the like). Strains for use in production of MVs can generally be selected on the basis of the amount of blebs produced in culture (e.g., bacteria can be cultured in a reasonable number to provide for production of blebs suitable for isolation and administration in the methods described herein). An exemplary strain that produces high levels of blebs is described in
PCT Publication No. WO 01/34642 - The antigenic compositions of the present disclosure can comprise vesicles from one strain, or from 2, 3, 4, 5 or more strains, which strains may be homologous or heterologous, usually heterologous, to one another. For example, the strains may be homologous or heterologous with respect to PorA. In one embodiment, the vesicles can be prepared from strains that express more than one chimeric fHBP (e.g., 1, 2, 3, or more chimeric fHBP) which may be composed of fHBP amino acid sequences from different variants (v.1, v.2, or v.3) or subvariants (e.g., a subvariant of v.1, v.2, or v.3).
- The antigenic compositions can comprise a mixture of OMVs and MVs presenting the same or different chimeric fHBPs, where the chimeric fHBPs may optionally present epitopes from different combinations of fHBP variants and/or subvariants and where the OMVs and/or MVs may be from the same or different strains. Vesicles from different strains can be administered as a mixture, or can be administered serially.
- Where desired (e.g., where the strains used to produce vesicles are associated with endotoxin or particular high levels of endotoxin), the vesicles are optionally treated to reduce endotoxin, e.g., to reduce toxicity following administration. Although less desirable as discussed below, reduction of endotoxin can be accomplished by extraction with a suitable detergent (for example, BRIJ-96, sodium deoxycholate, sodium lauroylsarcosinate, Empigen BB, Triton X-100, TWEEN 20 (sorbitan monolaurate polyoxyethylene),
TWEEN 80, at a concentration of 0.1-10%, preferably 0.5-2%, and SDS). Where detergent extraction is used, it is preferable to use a detergent other than deoxycholate. - In some embodiments the vesicles of the antigenic compositions are prepared without detergent, e.g., without use of deoxycholate. Although detergent treatment is useful to remove endotoxin activity, it may deplete the native fHBP lipoprotein and/or chimeric fHBP (including lipidated chimeric fHBP) by extraction during vesicle production. Thus it may be particularly desirable to decrease endotoxin activity using technology that does not require a detergent. In one approach, strains that are relatively low producers of endotoxin (lipopolysaccharide, LPS) are used so as to avoid the need to remove endotoxin from the final preparation prior to use in humans. For example, the vesicles can be prepared from Neisseria mutants in which lipooligosaccharide or other antigens that may be undesirable in a vaccine (e.g. Rmp) is reduced or eliminated.
- Vesicles can be prepared from N. meningitidis strains that contain genetic modifications that result in decreased or no detectable toxic activity of lipid A. For example, such strain can be genetically modified in lipid A biosynthesis (Steeghs et al. Infect Immun 1999;67:4988-93; van der Ley et al. Infect Immun 2001;69:5981-90; Steeghs et al. J Endotoxin Res 2004;10:113-9; Fissha et al, Infect Immun 73:4070,.2005). The immunogenic compositions may be detoxified by modification of LPS, such as downregulation and/or inactivation of the enzymes encoded by lpxL1 or lpxL2, respectively. Production of a penta-acylated lipid A made in lpxL1 mutants indicates that the enzyme encoded by lpxL1 adds the C12 to the N-linked 3-OH C14 at the 2' position of GlcN II. The major lipid A species found in lpxL2 mutants is tetra-acylated, indicating the enzyme encoded by lpxL2 adds the other C12, i.e., to the N-linked 3-OH C14 at the 2 position of GlcN I. Mutations resulting in a decreased (or no) expression of these genes (or decreased or no activity of the products of these genes) result in altered toxic activity of lipid A (van der Ley et al. 2001;69:5981-90). Tetra-acylated (lpxL2 mutant) and penta acylated (lpxL1 mutant) lipid A are less toxic than the wild-type lipid A. Mutations in the lipid A 4'-kinase encoding gene (lpxK) also decreases the toxic activity of lipid A. Of particular interest for use in production of vesicles (e.g., MV or OMV) are N. meningitidis strains genetically modified so as to provide for decreased or no detectable functional LpxL1-encoded protein. Such vesicles provide for reduced toxicity as compared to N. meningitidis strains that are wild-type for LPS production, while retaining immunogenicity of chimeric fHBP.
- LPS toxic activity can also be altered by introducing mutations in genes/loci involved in polymyxin B resistance (such resistance has been correlated with addition of aminoarabinose on the 4' phosphate of lipid A). These genes/loci could be pmrE that encodes a UDP-glucose dehydrogenase, or a region of antimicrobial peptide-resistance genes common to many enterobacteriaciae which could be involved in aminoarabinose synthesis and transfer. The gene pmrF that is present in this region encodes a dolicol-phosphate manosyl transferase (Gunn J. S., Kheng, B. L., Krueger J., Kim K., Guo L., Hackett M., Miller S. I. 1998. Mol. Microbiol. 27: 1171-1182).
- Mutations in the PhoP-PhoQ regulatory system, which is a phospho-relay two component regulatory system (e.g., PhoP constitutive phenotype, PhoPc), or low Mg++ environmental or culture conditions (that activate the PhoP-PhoQ regulatory system) lead to the addition of aminoarabinose on the 4'-phosphate and 2-hydroxymyristate replacing myristate (hydroxylation of myristate). This modified lipid A displays reduced ability to stimulate E-selectin expression by human endothelial cells and TNF secretion from human monocytes.
- Polymyxin B resistant strains are also suitable for use, as such strains have been shown to have reduced LPS toxicity (see, e.g., van der Ley et al. 1994. In: Proceedings of the ninth international pathogenic Neisseria conference. The Guildhall, Winchester, England). Alternatively, synthetic peptides that mimic the binding activity of polymyxin B may be added to the antigenic compositions to reduce LPS toxic activity (see, e.g., Rustici et al. 1993, Science 259:361-365; Porro et al. Prog Clin Biol Res. 1998;397:315-25).
- Endotoxin can also be reduced through selection of culture conditions. For example, culturing the strain in a growth medium containing 0.1 mg-100 mg of aminoarabinose per liter medium provides for reduced lipid toxicity (see, e.g.,
WO 02/097646 - "Antigen composition", "antigenic composition" or "immunogenic composition" is used herein as a matter of convenience to refer generically to compositions comprising a chimeric fHBP as disclosed herein, which chimeric fHBP may be optionally conjugated to further enhance immunogenicity. Compositions useful for eliciting antibodies, particularly antibodies against Neisseria meningitidis group B (NmB), in a human are specifically contemplated by the present disclosure. Antigenic compositions can contain 2 or more different chimeric fHBPs, where the chimeric fHBPs may present epitopes from different combinations of fHBP variants and/or subvariants.
- Antigenic compositions generally comprise an immunologically effective amount of chimeric fHBP, and may further include other compatible components, as needed. By "immunologically effective amount" is meant that the administration of that amount to an individual, either in a single dose, as part of a series of the same or different antigenic compositions, is effective to elicit an antibody response effective for treatment or prevention of a symptom of, or disease caused by, for example, infection by Neisseria, particularly N. meningitidis, more particularly Group B N. meningitidis. This amount varies depending upon the health and physical condition of the individual to be treated, age, the capacity of the individual's immune system to produce antibodies, the degree of protection desired, the formulation of the vaccine, the treating clinician's assessment of the medical situation, and other relevant factors. It is expected that the amount will fall in a relatively broad range that can be determined through routine trials.
- Dosage regimen may be a single dose schedule or a multiple dose schedule (e.g., including booster doses) with a unit dosage form of the antigenic composition administered at different times. The term "unit dosage form," as used herein, refers to physically discrete units suitable as unitary dosages for human and animal subjects, each unit containing a predetermined quantity of the antigenic compositions of the present invention in an amount sufficient to produce the desired effect, which compositions are provided in association with a pharmaceutically acceptable excipient (e.g., pharmaceutically acceptable diluent, carrier or vehicle). The antigenic composition may be administered in conjunction with other immunoregulatory agents.
- Antigenic compositions can be provided in a pharmaceutically acceptable excipient, which can be a solution such as a sterile aqueous solution, often a saline solution, or they can be provided in powder form. Such excipients can be substantially inert, if desired.
- The antigenic compositions can further comprise an adjuvant. Examples of known suitable adjuvants that can be used in humans include, but are not necessarily limited to, alum, aluminum phosphate, aluminum hydroxide, MF59 (4.3% w/v squalene, 0.5% w/
v Tween 80™, 0.5% w/v Span 85), CpG-containing nucleic acid (where the cytosine is unmethylated), QS21, MPL, 3DMPL, extracts from Aquilla, ISCOMS, LT/CT mutants, poly(D,L-lactide-co-glycolide) (PLG) microparticles, Quil A, interleukins, and the like. For experimental animals, one can use Freund's, N-acetyl-muramyl-L-threonyl-D-isoglutamine (thr-MDP), N-acetyl-nor-muramyl-L-alanyl-D-isoglutamine (CGP 11637, referred to as nor-MDP), N-acetylmuramyl-L-alanyl-D-isoglutaminyl-L-alanine-2-(1'-2'-dip- almitoyl-sn-glycero-3-hydroxyphosphoryloxy)-ethylamine (CGP 19835A, referred to as MTP-PE), and RIBI, which contains three components extracted from bacteria, monophosphoryl lipid A, trehalose dimycolate and cell wall skeleton (MPL+TDM+CWS) in a 2% squalene/Tween 80 emulsion. The effectiveness of an adjuvant may be determined by measuring the amount of antibodies directed against the immunogenic antigen or antigenic epitope thereof. - Further exemplary adjuvants to enhance effectiveness of the composition include, but are not limited to: (1) oil-in-water emulsion formulations (with or without other specific immunostimulating agents such as muramyl peptides (see below) or bacterial cell wall components), such as for example (a) MF59™ (
WO 90/14837 WO 00/07621 WO99/44636 GB-2220221 EP-A-0689454 , optionally in the substantial absence of alum when used with pneumococcal saccharides e.g.WO 00/56358 EP-A-0835318 ,EP-A-0735898 ,EP-A-0761231 ; (7) oligonucleotides comprising CpG motifs (Krieg Vaccine 2000, 19, 618-622; Krieg Curr opin Mol Ther2001 3:15-24; Roman et al., Nat. Med, 1997, 3, 849-854; Weiner et al., PNAS USA, 1997, 94, 10833-10837; Davis et al, J. Immunol, 1998, 160, 810-876; Chu et al., J. Exp. Med, 1997, 186, 1623-1631; Lipford et al, Ear. J. Immunol., 1997, 27, 2340-2344; Moldoveami e/al., Vaccine, 1988, 16, 1216-1224, Krieg et al., Nature, 1995, 374, 546-549; Klinman et al., PNAS USA, 1996, 93, 2879-2883; Ballas et al, J. Immunol, 1996, 157, 1840-1845; Cowdery et al, J. Immunol, 1996, 156, 4570-4575; Halpern et al, Cell Immunol, 1996, 167, 72-78; Yamamoto et al, Jpn. J. Cancer Res., 1988, 79, 866-873; Stacey et al, J. Immunol., 1996, 157,2116-2122; Messina et al, J. Immunol, 1991, 147, 1759-1764; Yi et al, J. Immunol, 1996, 157,4918-4925; Yi et al, J. Immunol, 1996, 157, 5394-5402; Yi et al, J. Immunol, 1998, 160, 4755-4761; and Yi et al, J. Immunol, 1998, 160, 5898-5906; International patent applicationsWO 96/02555 WO 98/16247 WO 98/18810 WO 98/40100 WO 98/55495 WO 98/37919 WO 98/52581 WO 99/52549 WO 01/21207 WO 01/21152 WO 00/62800 WO 00/23105 WO 99/11241 WO 98/57659 - The antigen compositions may comprise other components, such as pharmaceutical grades of mannitol, lactose, starch, magnesium stearate, sodium saccharin, talcum, cellulose, glucose, sucrose, magnesium, carbonate, and the like. The compositions may contain pharmaceutically acceptable auxiliary substances as required to approximate physiological conditions such as pH adjusting and buffering agents, toxicity adjusting agents and the like, for example, sodium acetate, sodium chloride, potassium chloride, calcium chloride, sodium lactate and the like.
- The concentration of chimeric fHBP in a formulation can vary widely (e.g., from less than about 0.1%, usually at or at least about 2% to as much as 20% to 50% or more by weight) and will usually be selected primarily based on fluid volumes, viscosities, and patient-based factors in accordance with the particular mode of administration selected and the patient's needs.
- Chimeric fHBP-containing formulations can be provided in the form of a solution, suspension, tablet, pill, capsule, powder, gel, cream, lotion, ointment, aerosol or the like. It is recognized that oral administration can require protection of the compositions from digestion. This is typically accomplished either by association of the composition with an agent that renders it resistant to acidic and enzymatic hydrolysis or by packaging the composition in an appropriately resistant carrier. Means of protecting from digestion are well known in the art.
- Chimeric fHBP-containing formulations can also provided so as to enhance serum half-life of chimeric fHBP following administration. For example, where isolated chimeric fHBP are formulated for injection, the chimeric fHBP may be provided in a liposome formulation, prepared as a colloid, or other conventional techniques for extending serum half-life. A variety of methods are available for preparing liposomes, as described in, e.g., Szoka et al., Ann. Rev. Biophys. Bioeng. 9:467 (1980),
U.S. Pat. Nos. 4,235,871 ,4,501,728 and4,837,028 . The preparations may also be provided in controlled release or slow-release forms. - The chimeric fHBP-containing antigenic compositions are generally administered to a human subject that is at risk of acquiring a Neisserial disease so as to prevent or at least partially arrest the development of disease and its complications. An amount adequate to accomplish this is defined as a "therapeutically effective dose." Amounts effective for therapeutic use will depend on, e.g., the antigenic composition, the manner of administration, the weight and general state of health of the patient, and the judgment of the prescribing physician. Single or multiple doses of the antigenic compositions may be administered depending on the dosage and frequency required and tolerated by the patient, and route of administration.
- The chimeric fHBP-containing antigenic compositions are generally administered in an amount effective to elicit an immune response, particularly a humoral immune response, in the host. As noted above, amounts for immunization will vary, and can generally range from about 1 µg to 100 µg per 70 kg patient, usually 5 µg to 50 µg/70 kg. Substantially higher dosages (e.g. 10 mg to 100 mg or more) may be suitable in oral, nasal, or topical administration routes. The initial administration can be followed by booster immunization of the same of different chimeric fHBP-containing antigenic composition. Usually vaccination involves at least one booster, more usually two boosters.
- In general immunization can be accomplished by administration by any suitable route, including administration of the composition orally, nasally, nasopharyngeally, parenterally, enterically, gastrically, topically, transdermally, subcutaneously, intramuscularly, in tablet, solid, powdered, liquid, aerosol form, locally or systemically, with or without added excipients. Actual methods for preparing parenterally administrable compositions will be known or apparent to those skilled in the art and are described in more detail in such publications as Remington's Pharmaceutical Science, 15th ed., Mack Publishing Company, Easton, Pa. (1980).
- An anti-chimeric fHBP immune response can be assessed by known methods (e.g. by obtaining serum from the individual before and after the initial immunization, and demonstrating a change in the individual's immune status, for example an immunoprecipitation assay, or an ELISA, or a bactericidal assay, or a Western blot, or flow cytometric assay, or the like).
- In one embodiment, the antigenic compositions can be administered to a human subject that is immunologically naive with respect to Neisseria meningitidis. In a particular embodiment, the subject is a human child about five years or younger, and preferably about two years old or younger, and the antigenic compositions are administered at any one or more of the following times: two weeks, one month, 2, 3, 4, 5, 6, 7, 8, 9, 10, or 11 months, or one year or 15, 18, or 21 months after birth, or at 2, 3, 4, or 5 years of age.
- It may be generally desirable to initiate immunization prior to the first sign of disease symptoms, or at the first sign of possible or actual exposure to infection or disease (e.g., due to exposure or infection by Neisseria).
- It is understood that the examples and embodiments described herein are for illustrative purposes only and that various modifications or changes in light thereof will be suggested to persons skilled in the art and are to be included within the spirit and purview of this application and scope of the appended claims. All publications, patents, and patent applications cited herein are hereby incorporated by reference in their entirety for all purposes.
- The following methods and materials were used in the Examples below.
- Gene cloning. Wild-type fHBP genes were amplified from genomic DNA by PCR and cloned into pGEM-T-Easy (Promega). The resulting plasmids were treated with the restriction enzymes NdeI and XhoI and the approximately 800 base-pair fragments containing the fHBP coding sequences were ligated into pET21b (Novagen) cut with the same two enzymes. The plasmid clones were confirmed by DNA sequence determination of PCR products obtained by the amplification of the plasmid with primers specific for the T7 promotor and terminator regions. The plasmids encoded the full-length fHBP proteins except for the amino-terminal 19 amino acid signal sequence and 7 presumably flexible N-terminal residues, and included a C-terminal hexa-histidine (His6) tag originating from the pET21b plasmid.
- fHBP Chimera I lacking a signal sequence was constructed by PCR amplification of the region encoding residues 8-135 from genomic DNA from strain MC58 (fHBP v.1) and that encoding residues 136-255 from strain 8047 (v.2). The two fragments, including an overlapping region of 48 base pairs centered around amino acids 136-139, were assembled by PCR amplification using external, gene-specific primers containing the NdeI and XhoI restriction sites. The chimeric gene was cloned into pET21b as described for wild-type genes above.
- Site-specific mutagenesis. Site-specific mutagenesis was used to test predictions of amino acid residues involved in anti-fHBP mAb epitopes and to create Chimera II. Mutagenesis was performed using the QuikChange II kit (Stratagene) using 10 ng of plasmid template and the manufacturer's protocols. For testing residues putatively involved in mAb epitopes, mutagenesis reactions were performed on pET21-based plasmids encoding wild-type fHBP genes from various strains. A residue in a reactive sequence was changed to that naturally present in a non-reactive sequence or vice versa. To construct Chimera II, site-specific mutagenesis was used to introduce the A174K substitution into the pET21 plasmid encoding Chimera I. Mutant fHBP genes were confirmed by DNA sequencing as described for the wild-type plasmids, above.
- fHBP expression and purification. Wild-type, mutant and chimeric fHBPs were expressed in Escherichia coli BL21(DE3) (Novagen). fHBP purifications were performed from 1 L cultures. Mid-exponential cultures (optical density at 600 nm of 0.5-0.6) were grown at 37 °C, induced with 0.5 mM isopropylthiogalactoside for 3-4 h and the bacteria harvested by centrifugation. The cells were lysed by incubation with chicken egg white lysozyme (Sigma) and two freeze/thaw cycles. Bacterial lysates were treated with DNase and RNase (Sigma) and protease inhibitors (Complete EDTA-free, Roche) and clarified by centrifugation at 13,000 x g. Recombinant fHBPs were purified by nickel chelate chromatography using Ni-NTA agarose (Qiagen) and buffers recommended by the supplier. Fractions containing purified fHBP were pooled and dialyzed against PBS (Roche) containing 5% (w/v) sucrose and 0.01% NaN3, filter sterilized and stored at 4 °C.
- mAb preparation. We generated hybridoma cell lines from spleens from CD-1 mice immunized with recombinant fHBP variant group 2 (gene from strain 2996) or variant group 3 (gene from strain M1239) using methods previously described for preparation of hybridoma cell lines secreting mAbs against fHBP v.1 protein (Welsch et al., J. Immunol. 2004). mAbs were precipitated from tissue culture supernatants with 50% saturated (NH4)2SO4 and dialyzed against phosphate-buffered saline (PBS; Roche). IgG isotypes were determined using Clonotyping-AP reagents (Southern Biotech).
- Direct-binding and inhibition ELISA. Binding of the mAbs to recombinant fHBP was measured by ELISA. The wells of a microtiter plate (Immulon 2B; Thermo Electron Corp.) were coated with 1 µg/ml of recombinant fHBP in PBS and incubated overnight at 4 °C. The plates were blocked with PBS containing 0.1% Tween-20 (Sigma) (PBST) and 1% BSA (Sigma). The primary antibodies were anti-fHBP mAbs (0.016 to 5 µg/ml) and the secondary antibody was rabbit anti-mouse IgG-alkaline phosphatase (Zymed; 1:5,000), each diluted in PBST. After 1 h at room temperature, alkaline phosphatase substrate (Sigma) was added and the absorbance at 405 nm was measured after 30 min.
- For competitive inhibition ELISAs, one mAb was held at a fixed concentration sufficient to obtain an OD at 405 nm of 1.0 determined by direct binding ELISA, as described above. A second mAb of a different isotype was added together with the first mAb to the wells of a microtiter plate coated with the antigen as described above, at concentrations ranging from 0.4 to 50 µg/ml. The secondary mAb was an isotype specific mouse anti-IgG-alkaline phosphatase conjugate. The ELISA was developed as described above.
- Inhibition of binding of factor H. The ability of an anti-fHBP mAb to inhibit binding of fH to fHBP was measured by ELISA. Wells of a microtiter plate were coated with rfHBP as described above. Dilutions containing 0.016 to 50 µg/ml of the mAb were added to the wells together with 50 µg/ml purified fH (Complement Technology, Inc.). The plates were incubated overnight at 4°C. Bound fH was detected with goat polyclonal anti-fH (Bethyl Laboratories) (1:1000) followed by mouse anti-goat IgG alkaline phosphatase conjugate (Santa Cruz Biotech) (1:2000). Both steps were performed at room temperature for 2 hours. After washing, substrate was added and developed as described above for the antibody binding ELISA.
- Western blotting. One mL of bacterial culture was grown and induced as described above (see fHBP expression and purification, above). The cells were harvested by centrifugation and were resuspended in 0.5 mL of 1x LDS sample buffer (Invitrogen) containing 25 mM 2-ME.Bacterial lysates were separated by SDS-PAGE using 4-12% NuPAGE polyacrylamide gels and MES SDS-PAGE buffer (Invitrogen). Proteins were transferred to polyvinylidene difluoride (PVDF) membranes (Immobilon-P; Millipore). The membranes were blocked using PBST containing 2% nonfat dry milk (Carnation, Nestle, Inc.). The membranes were washed, incubated with the different anti-fHBP mAbs (1 to 5 µg/ml) or, as a control for protein expression by the different clones, 0.02 µg/ml of Penta-His mAb (Qiagen). The membranes were washed in PBST and incubated with a 1:10,000 dilution of a rabbit anti-mouse IgG-horseradish peroxidase conjugate (Zymed) and washed again. The membranes were developed with a chemiluminescent substrate (ECL+; GE Healthcare) and visualized on a Storm 840 imager (Molecular Dynamics).
- Mouse immunization. Groups (5 mice each) of five-week old CD-1 mice (Charles River) were immunized with four doses containing 20 µg of wild-type or chimeric fHBP vaccines or adjuvant alone at two-week intervals. Each experimental or control vaccine was administered with aluminum hydroxide or Freund's adjuvant (FA) (complete FA for the first dose and incomplete FA for subsequent doses).
- Bactericidal activity. Complement-mediated bactericidal activity was measured as described previously using washed, log-phase bacteria grown in Mueller-Hinton broth supplemented with 0.25 % glucose and 0.02 mM CMP-NANA to an OD620 of 0.6. The buffer was Dulbecco's phosphate buffered saline (Mediatech, Inc.) containing 0.9 mM CaCl2 x 2 H2O, 0.5 mM MgCl2 x 6 H2O and 1% (w/v) BSA. The complement source was human serum from a healthy adult with no detectable intrinsic bactericidal activity. For synergism of mAb bactericidal activity, equal quantities of two mAbs ranging from 0.4 to 50 ug/ml (final concentration) were used. The bactericidal activity (BC50) of the mouse antiserum (or mAb combination) was defined by the dilution (or mAb concentration) that gave a 50% decrease in the number of CFU after 60 min incubation at 37 °C as compared with the CFU at
time 0 in the negative control reactions. - This study used a panel of twelve murine monoclonal antibodies (mAbs) that had been prepared against recombinant proteins representative of the three major variant groups of factor H binding protein (fHBP). These variant groups are designated variant 1 (v.1; Welsch et al. J Immunol 2004;172: 5606-15), variant 2 (v.2, Beernink et al. J Infect Dis 2007;195:1472-9) and v.3 (Beernink et al, (2008) Infect Immun 76: 4232-4240). As illustrated by the summary of selected features of these mAbs in the tables of
Figures 17 and18 , each of these mAbs is bactericidal when combined with a second mAb. Inaddition JAR 1 andJAR 3 are individually bactericidal when tested against certain strains expressing v.1 fHBP. - The results summarized in
Figure 18 are evidence that the epitopes recognized by each of the mAbs is surface-exposed on encapsulated meningococcal strains and capable of interacting with protective antibodies. - Nine of these JAR mAbs were used as tools to determine amino acid residues in fHBP that contribute to the epitopes for binding of these mAbs so as to provide for structural predictions on the locations of epitopes of fHBP from different variant groups that interact with bactericidal antibodies. This information could then be used to construct chimeric fHBP vaccines that express epitopes from more than one variant group and that are capable of eliciting antibodies that confer protection against strains expressing different fHBP variants.
- For convenience in facilitating prior studies aimed at identifying bactericidal regions of fHBP, the protein was divided into three domains, designated A, B and C (Giuliani et all. Infect Immun 2005;73:1151-60). As discussed above, the A domain is highly conserved across v.1 and v.2 variant groups, whereas the B and C domains contain sequences that diverge among strains. Previously, the only known fHBP epitope interacting with a bactericidal mAb was located in the C domain at R204 (Giuliani et al. supra). (Note that the convention of numbering amino acid residues beginning with the first residue after the signal sequence is adopted herein). However, a chimeric protein vaccine composed of the B domain from a
variant 3 strain (B3) fused with the C domain of avariant 1 strain (C1) failed to elicit protective bactericidal responses against strains with eithervariant - As will be set out in more detail below, the inventors identified the location of an epitope defined by two anti-fHBP mAbs,
JAR 3 and 5 (referred to herein as the "JAR3/5" epitope), in the B1 domain around residue G121.JAR 3 individually was known to be bactericidal with human complement against strains from sequence type (ST) complex 32 (Welsch et al. J Immunol 2004;172:5606-15) and, bothJAR 3 andJAR 5 when combined with other mAbs were broadly bactericidal against strains expressing subvariants ofvariant 1 fHBP (Welsch et al., supra). JAR 3 (Madico et al. J Immunol 2006;177:501-10) andJAR 5 also inhibited binding of factor H (fH) to the surface of encapsulated N. meningitidis strains. It should be noted that with the exception of JAR3/5, all of the other mAbs mapped to date were found to bind to epitopes that are part of the C domain. - The observations relating to the
JAR 3/5 epitope being present in the B domain formed the rationale for fusing the portion of the protein of v. 1 B domain containing the JAR3/5 epitope (e.g., up to residue 136) with the remaining portion of the B domain and entire C domain of the v.2 protein (Chimera I). Inclusion of theJAR 3/5 epitope from v. 1 at resides near and including G121 elicited broadly protective antibodies to v.1 and v.1 subvariant strains. - Further, by inclusion of the other epitopes such as
JAR - Thus, in contrast to the B3C1 chimeric previously reported, a chimeric protein vaccine composed of the A1 domain (which is highly conserved across
variant 1 and 2), the N-terminal portion of the B1 domain expressing theJAR 3/5 epitope fused with the distal terminal portion of the B1 domain and C1 domain elicited cross-protective bactericidal antibodies in immunized mice. - The
JAR 11 epitope is expressed by about one-third of disease-producing N. meningitidis strains in the U.S. that express fHBP v.2 or v.3 (Beernink 2007 J. Infect Dis, supra). Approximately 50 percent of the JAR 11-negative strains with v.2 or v.3 fHBP express theJAR 32/35 epitope. Therefore, to increase coverage against these strains, the Chimera II vaccine was prepared, in which a single amino acid change, A174K, was introduced into the C domain that inactivated the epitope recognized byJAR 11 and introduced the epitope recognized byJAR 32/35. Despite engineering expression of theJAR 11 epitope in Chimera I and theJAR 32 epitope in Chimera II, there was no statistically significant differences in the respective serum bactericidal antibody responses of mice immunized either vaccine against strains expressing v.2 or v.3 fHBP that were JAR 11-positive or JAR 32-positive. - As set out below, it was later found that binding of antibody to an epitope located near residue 174 (i.e.,
JAR 11 in some strains, andJAR 32 in others; seeFigure 1 ) was not sufficient to elicit significant complement-mediated bactericidal activity in the absence of a second mAb binding to an epitope associated with ion pair at residues 180 and 192 (such asJAR 10 in some strains orJAR 33 in others (See Table inFig. 20 )). Among wild-type strains expressing fHBP v.2 or v.3, expression ofJAR 32 is often associated with expression of JAR 33 (for example, strains 03S-0658, M1239 and SK104, Table inFigure 8A ), while expression ofJAR 11 is usually associated with expression of JAR 10 (see for example ourstrains 8047, MD1435 and MD1321,Figure 8A ). This insight pointed to production of chimeric fHBP vaccines effective against JAR 32-positive strains by also introducing theJAR 33 epitope. - Further, as set out below, it was discovered that bactericidal activity of antibodies is enhanced when two antibodies bind their respective epitopes located at a distance of about 18 - 20 Ǻ. Stated differently, a greater bactericidal effect was observed when two antibodies bound epitopes located about 18-20 Ǻ apart on the chimeric fHBP compared to the bactericidal effect of these antibodies alone. In contrast, binding of two antibodies to epitopes positioned at a greater distance apart (e.g., ≥ about 27 Ǻ) did not enhance bactericidal activity, which may be due to the reduced ability of these bound antibodies to provide for enhanced interaction with C1q of the complement cascade. Binding of two antibodies to epitopes positioned ≤ about 14 Ǻ apart also did not provide for enhanced bactericidal activity, which may be the result of steric hindrance of binding of one antibody by the other. Thus, chimeric fHBP which contain epitopes that elicit antibodies that bind to epitopes within about 18 - 20 Ǻ apart can provide for further enhanced bactericidal antibody production. Examples of such epitope pairs are those epitopes bound by
JAR 10 andJAR 11; and byJAR 33 andJAR 32/ 35 (JAR 32 andJAR 35 bind to the same (or overlapping) epitopes). - The effect of chimeric fHBP polypeptides as vaccines can be further enhanced by including epitopes that elicit antibodies that block fH binding. For example, as set out below, when the epitopes bound by JAR 13 (v.2 epitope), JAR 11 (v.2 epitope), and
JAR 32/35 (v.3 epitope) are bound by antibody, binding of fHBP to fH is inhibited. Thus, the presence of such fH-binding epitopes in the chimeric fHBP polypeptides can provide for production of antibodies that can facilitate protection through this pathway. - Details of the studies that led to this discovery are set out below.
- Selected known properties of JAR mAbs are summarized in the tables of
Figures 17 and18 . Notably,JAR 3 andJAR 5 were known to bind to v.1 or subvariants of v.1 fHBP expressed by strains MC58, 4243, M1390, and NZ98/254 but not to strain M6190 (Welsch et al. J Immunol 2004;172:5606-15). Further, fHBP expressed by M6190 had an arginine at position 121 (R121) whereas the fHBPs from the four reactive strains had glycine at position 121 (G121) (Welsch et al. J Immunol 2004;172:5606-15). - In order to confirm that G121 was important for
JAR 3 andJAR 5 binding, site-specific mutagenesis was used to change the glycine residue at position 121 in the fHBP sequence of strain MC58 to arginine. - As illustrated in the Western blots of
Figure 1 , the G121R substitution resulted in loss ofJAR 3 andJAR 5 reactivity (Figure 1 , Panel A). The converse change in fHBP from strain M6190, R121G, introduced theJAR 5 epitope (Figure 1 , Panel A, lane 6) and, to a lesser extent, theJAR 3 epitope (Figure 1 , Panel B, lane 6). The weaker signals for the M6190 mutant R140G protein, particularly forJAR 3, indicated that additional residues may have been important for the these epitopes. The Penta-His control mAb showed that the wild-type and mutant proteins were produced in similar quantities (Figure 1 , Panel C). - Additional evidence that
JAR 3 andJAR 5 recognized overlapping epitopes was derived from competitive inhibition experiments. - The results are shown in
Figure 2 . JAR 5 (5 µg/ml) inhibited binding ofJAR 3 by greater than 90% (Figure 2 , Panel A) and the reciprocal reaction withJAR 3 inhibited binding of JAR 5 (Figure 2 , Panel B). In contrast, there was no detectable inhibition of binding ofJAR 4 by JAR 3 (50 µg/ml) or JAR 5 (50 µg/ml) (Figure 2C ).JAR 4 also did not inhibit binding of JAR 3 (Figure 2 , Panel A) or JAR 5 (Figure 2 , Panel B). The positive control, a 1:10 dilution of rabbit anti-fHBP v.1 antiserum, inhibited binding of all three mAbs, whereas pre-immune rabbit serum and negative control mAbs gave less than 7% inhibition. ThusJAR 3 andJAR 5 recognize overlapping (or identical) epitopes, since each of these mAbs inhibited binding of the other to fHBP. - To investigate the epitopes defined by the remaining anti-fHBP mAbs in the panel, site-specific mutagenesis was used to create knock-outs (KO) of recombinant fHBPs. For nine of the mAbs, an fHBP KO lacking the indicated residue resulted in a significant loss of binding of the corresponding JAR mAb as measured by Western blot and/or ELISA (see Table in
Figure 29 .) For seven of the mAbs, it was demonstrated that the respective mAb that was negative for binding became positive for binding after introduction of one or two of the corresponding amino acid substitutions (see Table inFigure 29 ). Taken together, one or both of these strategies was successful in identifying amino acid residues involved in the reactivity of nine of the JAR mAbs (Figure 3 ). -
Figures 30-32 provide supporting data for identification of residues involved in JAR mAb binding. E. coli lysates containing plasmids expressing the respective wild-type and mutant fHBPs were analyzed by Western blot using the appropriate JAR mAb, as well as a control antibody to detect an epitope tag present on the fHBP (penta-His). - Specifically,
Figure 30 is a Western blot indicating residues involved in theJAR 10 andJAR 33 epitopes, in which E. coli lysates containing plasmids expressing the respective wild-type and mutant fHBPs were analyzed by Western blot with JAR 10 (Panel A) or Penta-His mAb (Panel B).Figure 31 is a Western blot indicating a residue involved in theJAR 11,JAR 32 andJAR 35 epitopes, in which E. coli lysates containing plasmids expressing the respective wild-type and mutant fHBPs were analyzed by Western blot with JAR 32 (Panel A), JAR 35 (Panel B), JAR 11 (Panel C) or Penta-His mAb (Panel D).Figure 32 is a Western blot indicating residue involved in theJAR 13 epitope, in which E. coli lysates containing plasmids expressing wild-type and mutant fHBPs were were probed with JAR 13 (Panel A) or Penta-His mAb (Panel B) and anti-mouse IgG-HRP secondary antibody. - It should be noted that the numbering of the amino residues used herein is with reference to the mature protein sequence (i.e. lacking the signal) of fHBP from strain MC58 (i.e., the fHBP amino acid sequence of MC58 was used as the reference v.1 fHBP amino acid sequence). Because the total number of amino acid residues in v.2 and/or v.3 fHBPs differ from the total number of amino acid residues in v.1 fHBPs, the amino acid sequences of the v.2 protein (with fHBP from
strain 8047 used as the reference v.2 amino acid sequence) and v.3 fHBP (with fHBP from strain M1239 used as the reference v.3 amino acid sequence) differ by -1 and +7 amino acid residues, respectively, from that of MC58. Thus, for example, a leucine residue (L) referred to using the numbering system herein as being at position 166 of the v.2 or v.3 fHBP sequence is actually at position 165 of the v.2 protein and at position 173 in the v.3 protein based on the actual amino acid sequence of these proteins, rather than on the numbering used herein based on the alignment of these sequences with v. 1 fHBP of MC58. - In addition, the role of JAR mAb epitopes in fH binding by fHBP was investigated.
Figure 19 is a series of graphs showing the ability of representative JAR mAbs prepared against fHBP v.2 (8047), v.3 (MI239), or v.1 (MC58) recombinant proteins to give concentration-dependent inhibition of binding of fH to rfHBP v.2 (Panel A), rfHBP v.3 (Panel B), or rfHBP v.1 (Panel C) in an ELISA. These data show that some of the contact residues defined by the JAR mAb epitopes are involved in binding to fH. These data thus argue for possible inclusion or preservation of JAR mAb epitopes that are involved in fH binding since blocking of binding of fH to N. meningitidis can provide a further mechanism of protection. - As noted above, the epitopes defined by
JAR 3 andJAR 5, are located within the B domain ofvariant 1 fHBP beginning approximately 19 amino acid residues N-terminal to the start of α-helix AH2, or approximately 15 amino acid residues N-terminal to the amino acid sequence of GEHT,. A first chimeric fHBP (referred to herein as "Chimera I") was constructed by combining a portion of the gene encoding the A domain and the N-terminal portion of the B domain up to residue G136 from v.1 fHBP of MC58 with the distal portion of the gene encoding the alpha-helix of the B domain and C domain of v.2 fHBP fromstrain 8047. The residue at position G136 was used as a convenient crossover position (the point at which the chimeric sequence "shifted" from that of the v.1 fHBP to that of the v.2 fHBP). G136 is N-terminal the α-helix AH2 and begins a sequence of four highly conserved residues, GEHT, which are shown in a box inFigure 4 . The outer brackets show the region of the protein previously defined as the B domain (Giuliani et al. Infect Immun 2005;73:1151-60). - A second chimeric fHBP, referred to herein as Chimera II, was generated. Chimera II was identical in amino acid sequence to Chimera I except for the introduction the A174K substitution (Bold and underlined K, Chimera II,
Figure 4 ). It should be noted that the A domain is not shown inFigure 4 , or in the NMR-based structure ofFigure 5 , but would be attached at the N-terminus labeled "N" inFigure 5 . - Models of the two chimera vaccines are shown in
Figure 5 , Panels A and B. Chimera I contains theJAR 11 epitope, including residue A174 (Figure 5 , Panel A). Chimera II contains theJAR 32 andJAR 35 epitopes, including residue K174 (Figure 5 , Panel B). The model of the fHBP chimeras was constructed based on the NMR structure of Cantini et al. J Biol Chem 2006;281:7220-7. - Recombinant proteins were expressed in E. coli as C-terminal hexahistidine (His6) fusions, which were purified by metal chelate chromatography. Specifically, Proteins were expressed from pET21-based plasmids in E. coli BL21(DE3) as C-terminal hexa-histidine fusions. Fusion proteins were then isolated by metal chelate chromatography according to methods known in the art. Isolated proteins were dialyzed against 1x PBS, 5% sucrose, 1 mM DTT and filter sterilized. Proteins (5 µg each) were separated on a 4-12% polyacrylamide gel and stained with Coomassie blue.
- The results are shown in
Figure 6 .Lane 1, mass standard; 2, fHBP v.1 (MC58); 3, fHBP v.2 (8047); 4, fHBP Chimera I; 5, fHBP Chimera II. - ELISA was used to assess concentration-dependent binding of the anti-fHBP mAbs to the chimeric antigens isolated in Example 4. As expected,
JAR 1, which binds to a v.1 epitope in the C domain (R204), did not bind to either of the chimeric proteins (Fig. 7 , Panel A).JAR 5, which is specific for an epitope on the B domain of fHBP v.1, andJAR 4, which cross-reacts with an epitope that is not yet defined by expressed by v.1 and v.2, showed identical respective concentration-dependent binding with the two chimeric proteins as compared with the respective wild-type v.1 and/or v.2 proteins. -
Figure 7 , Panel B, provides binding data formAbs JAR Figure 20 ), and they showed similar respective concentration-dependent binding with the Chimera I protein as they did with the wild-type rfHBP v.2 control protein expressed from the gene of strain 8047 (Fig. 7 , Panel B). As expected,JAR 11 did not bind to Chimera II, since this protein had lysine substituted for alanine at position 174 (A174K), which eliminated theJAR 11 epitope and introduced theJAR 32 epitope (Panel C).JAR 36, which cross-reacts with an epitope not yet defined but present on fHBP v.2 and v.3 fHBP bound to both of the chimeric proteins, and to the wild-type rfHBP v.2 control but not with the fHBP v.1 control (Fig. 7 , Panel C). Collectively, the data showed that the two chimeric fHBPs expressed epitopes associated with fHBP v.1, v.2, and/or v.3 proteins, and reacted as expected with the various mAbs in accordance with our studies localizing the epitopes. - The proteins shown in
Figure 6 were used to immunize mice according to the schedule in Table 1, below. Four doses of vaccine (20 µg of protein) were administered IP with intervals of 2 weeks between doses. Mice were bled 2.5 weeks afterdose 4. CFA = complete Freund's adjuvant; IFA = incomplete Freund's adjuvant; Al(OH)3 = aluminum hydroxide. CFA/IFA below indicates that the mice received an initial dose with CFA, then subsequent booster doses with IFA. Where Al(OH)3 was used as the adjuvant, all doses were administered with aluminum hydroxide as the adjuvant.Table 1. Immunization schedule1 Group fHBP Protein Adjuvant 1 --- CFA/ IFA 2 fHBP v.1 CFA/ IFA 3 fHBP v.2 CFA/ IFA 4 Chimera I CFA/ IFA 5 Chimera II CFA/ IFA 6 --- Al(OH)3 7 fHBP v.1 Al(OH)3 8 fHBP v.2 Al(OH)3 9 Chimera I Al(OH)3 10 Chimera II Al(OH)3 1 Groups 1 to 10 consist of 5 CD-1 mice each (N=60). Each animal received four injections -
Figure 9 summarizes the serum antibody responses of the mice that received the chimeric vaccines administered with FA when measured against strain H44/76 (variant 1) and four additional strains that express subvariants of v.1 fHBP (i.e., fHBP proteins with relatively small amino acid differences (e.g., with greater than about 88%, and less than 97% amino acid sequence identity) between the sequence of the respective protein and that of v.1.1 fHBP of H44/76). The mice immunized with the wild-type rfHBP v.1 control protein had high responses to H44/76 (reciprocal GMT of nearly 10,000) and lower and variable responses against the other four test strains (ranging from a GMT of <1:10 against strain NZ98/254 to a GMT of >1:1,000 against SK084). The sera from the mice immunized with the rfHBP v.2 control protein were either negative for bactericidal activity (bactericidal titers <1:10, four strains) or weakly positive (reciprocal GMT of 1:10; strain SK141). The mice immunized with either chimeric protein vaccine developed serum bactericidal antibodies against all four strains that were susceptible to bactericidal activity of sera from the control mice immunized with rfHBP v.1. For three of the four strains, the respective reciprocal GMTs of the chimeric vaccine groups where ~ 1 log lower than those of mice given the control rfHBP v.1 vaccine whereas the responses to the fifth strain, SK141, were as high or higher than those of the mice given the control rfHBP v.1 vaccine. -
Figure 10 summarizes the serum bactericidal antibody responses as measured against the six strains expressing fHBPs in the v.2 or v.3 variant groups. Three of the strains wereJAR 11 positive (left panel) and three wereJAR 32 positive (right panel). Sera from control mice immunized with rfHBP v.2 were bactericidal against all six strains whereas, with one exception (strain 03S-0658), the serum bactericidal titers of control mice immunized with rfHBP v.1 were <1:10. The sera from the mice immunized with either chimeric vaccine were bactericidal against all six strains. For four of the strains (8047, MD1321, M1239 and SK104), the respective titers were ~1 log lower than those of the control mice immunized with rfHBP v.2. For the remaining two strains, 03S-0658 and MD1435) the titers elicited by one or both chimeric vaccines were similar to those of the mice given the positive control rfHBP v.2 vaccine. Thus, in contrast to the control rfHBP v.1 or v.2 vaccines, the chimeric vaccines elicited bactericidal antibody responses against strains expressing fHBP from each of the three antigenic variant groups. - The Chimera I vaccine expressed the
JAR 11 epitope while the Chimera II vaccine expressed theJAR 32 epitope (Fig. 1 ). However, with one exception, the respective responses of mice immunized with either chimeric vaccine when measured against strains expressing JAR 11- or JAR 32-positive fHBP were not significantly different from each other (Fig. 5 ). The exception was the JAR 11-positive strain MD1435, where there was a trend for a higher reciprocal GMT in the group of mice immunized with Chimera I than Chimera II (P =0.06). - Thus, the A174K substitution in Chimera II that eliminated the
JAR 11 epitope (v.2) and introduced theJAR 32/35 epitope (v.3) did not appreciably increase the bactericidal responses against a test strain expressing the v.3 protein. -
Figure 11 summarizes the serum bactericidal antibody responses of mice immunized with the chimeric vaccines when absorbed with aluminum hydroxide as measured against the panel of test strains with v.1 fHBP. The corresponding data for responses to test strains expressing v.2 or v.3 fHBP are shown inFigure 12 . In general the respective responses to the different vaccines absorbed with aluminum hydroxide paralleled those observed to the vaccines given with Freund's adjuvant although as expected the titers were somewhat lower with the aluminum hydroxide adjuvant. - The data above indicate that the JAR3/5 epitope, which is common to virtually all v.1 proteins but is not present in fHBP from v.2 or v.3 strains, is important for eliciting high bactericidal antibody titers to the
variant 1 fHBP protein. This discovery that the epitope recognized byJAR 3/5 plays an important role in eliciting v.1 fHBP bactericidal antibodies provides the basis for the rational design of further chimeric fHBP vaccines that can elicit bactericidal antibodies across strains expressing different fHBP protein variants, particularly against both v.1 and v.2 fHBP-expressing strains. For example, the two chimeric vaccines described above (Chimera I and Chimera II) included, from N-terminus to C-terminus: - 1) an A domain (common to both v.1 and v.2);
- 2) a heterologous B domain composed of, from N-terminus to C-terminus,
- a) a contiguous amino acid sequence of an N-terminal portion of a B domain of a v.1 fHBP containing the amino acid sequence defining the
JAR 3/5 epitope, operably linked to - b) a contiguous amino acid sequence defining the remainder of the B domain, which amino acid sequence is that of a B domain of a v.2 fHBP, where the v.2 fHBP amino acid sequence is present in the heterologous B domain following the amino acid sequence of GEHT; and
- a) a contiguous amino acid sequence of an N-terminal portion of a B domain of a v.1 fHBP containing the amino acid sequence defining the
- 3) a C domain of the v.2 protein.
- As noted above, the discovery that the
JAR 3/5 epitope in the N-terminal portion of v. 1 fHBP provides the basis for construction of additional chimeric fHBP polypeptides that can serve as vaccines to elicit cross-reactive, bactericidal antibodies against v.1 fHBP-expressing N. meningitidis strains and v.2 fHBP-expressing N. meningitidis strains. In order to provide guidance as to the amino acid sequences of v.1 fHBP that find use in the fHBP chimeric vaccines contemplated here, various v.1 fHBP amino acid sequences of the B domain were analyzed. -
Figure 13 provides an alignment of fHBP v.1 sequences with natural polymorphisms in the N-terminal portion of the B domain. The sequence conservation is shown below the alignment, with "*" denoting residues that are identical, ":"denoting residues that are conserved, and "."denoting residues that are semi-conserved across the aligned sequences. The positions of alpha-helices are shown above the alignment, with the residues implicated in the alpha helices indicated by italics. The residue, G121, which is implicated in theJAR 3 andJAR 5 epitope, is shown in bold and underlining. A lysine at position 122 (K122) also appears to be important in theJAR 3/5 epitope, since one strain that is negative forJAR 3 andJAR 5 binding, 03S-0408, has G121 but differs fromJAR 3/5 reactive strains in having serine at position 122 (S122). (data not shown) The amino acid sequence of GEHT that provides the point at which the B domain sequence of the chimera "switches" or "crosses over" to the amino acid sequence of a v.2 B domain in Chimera I and Chimera II (referred to herein as the "junction point") is shown in the box. - As shown in
Figure 13 , there are a number of natural polymorphisms in the region of G121, which is involved in theJAR 3/JAR 5 epitope. Notably, a fHBP containing R121 (rather than G121) does not express theJAR 3/JAR 5 epitope. However, polymorphisms near G121, for example P117 in NZ98/254 and D121 in 4243, do not interfere with the binding ofJAR 3 orJAR 5. Thus, some modifications at residues other than G121 provide forJAR 3/5 epitope expression. - The alignment thus provides guidance as to the types of amino acid substitutions that can be introduced while maintaining
JAR 3/5 epitope expression. Such amino acid substitutions can be either naturally-occurring (i.e., natural polymorphisms) or can be introduced by synthetic means (e.g., recombinant polymorphisms). Thus, the heterologous B domains of the chimeric fHBP polypeptides contemplated herein include those containing v. 1 B domain sequences with natural and synthetic polymorphisms in the proximal B domain, including both natural and synthetic variants. - In addition, to the
JAR 3/5 epitope, chimeric fHBPs contemplated herein generally include one or more epitopes of v.2 fHBP B and C domains, where the v.2 fHBP B domain epitopes are present at a location C-terminal to (i.e., distal to) the location of theJAR 3/5 epitope of v.1 fHBPs, which is generally C-terminal to the alpha helix that follows the sequence of GEHT, which is shared between v.1 and v.2 fHBPs. In order to provide guidance as to the amino acid sequences of v.2 fHBP that find use in the fHBP chimeric vaccines contemplated here, various v.2 fHBP amino acid sequences of the B domain, as well as the C domain were analyzed. -
Figure 14 provides an alignment of exemplary v.2 fHBP sequences of the distal portion of the B domain, and further provides exemplary v.2 fHBP sequences of the C domain, where the B domain is generally defined asresidues 101 to 164, with numbering based on MC58 fHBP as a reference. - Therefore, based on the polymorphic variants shown in
Figures 13 and 14 , variations in the amino acid sequence of v.2 fHBP B domains and C domains, as well as additional combinations of v.1/v.2 heterologous B domains with different v.2 C domains to can be readily envisioned to generate additional chimeric fHBPs.Figures 13 and 14 provide 7 exemplary amino acid sequences of the N-terminal region of the v.1 B domain (Figure 10) and 9 exemplary amino acid sequences for the distal portion of the B domain of v.2 fHBP and for the C domain of v.2 fHBP (Figure 11 ). Thus, the sequences inFigures 13 and 14 provide for a least 63 different fHBP chimeras, simply by combining the amino acid sequences as provided. Further, the alignments provide guidance as to the amino acid residues that can be substituted. - Thus, not only do these exemplary sequences provide guidance for use of amino acid sequences containing naturally-occurring polymorphisms, they also provide guidance for production of synthetically-generated variants (e.g., using recombinant methods). For example, additional point mutations may be introduced into the coding nucleic acid to provide for fHBP chimeras that express other desirable epitopes, such as the v.1 epitope recognized by
JAR 1/mAb 502 that is in the portion of the C domain (R204), or theJAR 11 epitope in Chimeras IV and V. Introduction of the JAR1/mAb 502 epitope can provide for improved cross-reactivity against v.1 strains from the ST-32 lineage that nearly always express theJAR 1 epitope, while eliciting antibodies to theJAR 11 epitope can provide for improved titers against v.2 strains (see Koeberling et al., J Infect Dis 2008, 198:262-270, for a description of v.1.1). - Note also, that despite engineering expression of the
JAR 11 epitope in Chimera I, and theJAR 32 epitope in Chimera II, no statistically significant differences were observed in the respective serum bactericidal antibody responses of mice immunized either vaccine against strains expressing v.2 or v.3 fHBP that were JAR 11-positive or JAR 32-positive. However, the discovery that binding of antibody to an epitope located near residue 174 (i.e.,JAR 11 in some strains, andJAR 32 in others; seeFigure 3 ) was not sufficient to elicit complement-mediated bactericidal activity in the absence of eliciting additional antibodies that bind to a second epitope associated with ion pair at residues 180 and 192 (such asJAR 10 in some strains orJAR 33 in others (Table inFigure 20 ) indicates that coverage can be improved against JAR 32-positive strains by engineering expression of a second epitope defined by binding with JAR 33 (i.e., R180/E192). Note that among wild-type strains expressing fHBP v.2 or v.3, expression ofJAR 32 is often associated with expression ofJAR 33, while expression ofJAR 11 is usually associated with expression of JAR 10 (see, for example, strain panel,Figure 8 ). - Table 2 and
Figures 15 and 16 provide for additional hypothetical chimeric vaccines, designated Chimera III, Chimera IV and Chimera V. Each of these chimeric fHBPs are generated using a strategy similar to that used to generate Chimera I to provide for a chimeric fHBP that elicits bactericidal anti-v.1 and v.2 antibodies. - As illustrated in
Figure 15 , Chimera III contains the A domain and proximal B domain of subvariant v.1.10 encoded by the fHBP from NZ98/254, and uses the same distal B domain and C domain of Chimera I and Chimera II. - Chimera IV, illustrated in
Figure 15 , includes the A and proximal B domains of Chimera I and Chimera II, but substitutes the distal B and C domains of v.2 from strain 8047 (v.2.1) of these chimera with those from RM1090 (v.2 subvariant). - Chimera V fuses the A and proximal B domains of a v. 1 subvariant (strain NZ98/254) with that distal B and C domains of v.2 subvariant (strain RM1090).
- The amino acid changes that will result in the respective Chimera III, IV and V vaccine antigens, as compared with the respective amino acid sequences of the A and proximal B domain of MC58 and distal B and C domains of 8047 used to prepare
Chimera 1 are shown inFigure 16 . Chimeras III and V can provide for increased breadth of protection against certain strains expressing subvariants of v.1, such as NZ98/254, which is not covered by the Chimera I or II vaccines. Chimeras IV and V can provide for extended protection against v.3 strains, which are poorly covered by Chimera I or Chimera II. - Table 2 provides a summary of the observed epitope expression for Chimera I and Chimera II, and further sets out the predicted epitope expression for proposed Chimeras III, IV, and V.
Table 2 Predicted (or observed) epitope expression by chimeric proteins Variant 1 Variant 1/2/3Variant 2/3mAb mAb 502/ J AR1 JAR 3/5 JAR 10JAR 11JAR 13JAR 32/35JAR 33Domain C B C C C C C Epitope R204 G121 K180 and E192 A174 S216 K174 R180, E192 Wild-type proteins MC58 (v.1) 1 1 0 0 0 0 0 NZ98/254 (v.1, sv) 0 1 1 0 0 0 0 8047 (v.2) 0 0 1 1 1 0 0 RM1090 (v.2, sv) 0 0 0 0 0 1 1 Chimeric proteins Chimera I 0 1 1 1 1 0 0 Chimera II 0 1 1 0 1 1 0 Proposed Chimerae Chimera III 0 1 1 1 1 0 0 Chimera IV 0 1 0 0 0 1 1 Chimera V 0 1 0 0 0 1 1 1 = presence of epitope; 0 = absence of epitope; sv, subvariant. mAb 502 was described by Giuliani et al (Infect Immun 2005; 73:1151-60).JAR JAR JAR Chimeras I and II were constructed to contain amino acid residues 1 to 135 encoded by fHBP gene v.1.1 (MC58) fused withresidues 136 to 255 of v.2.1 gene from 8047. Chimera II also contains a point mutation A174K introduced into the C domain that inactivates the epitope recognized byJAR 11 and introduces the epitope recognized byJAR 32/35.Proposed Chimeras III, IV and V are examples of additional chimeric fHBPs, with predicted epitope expression as defined by binding of the respective JAR mAbs shown. - Further modifications of the chimeric fHBP include varying the residue within the heterologous B domain at which the v.1 fHBP B domain sequence ends and the v.2 (or v.2) fHBP B domain sequence ends. Specifically, although residue G136 was used as the position of the "crossover" between fHBP variants, the "crossover" residue can be any residue C-terminal of the amino acid sequence defining the
JAR 3/JAR 5 epitope and a residue within M123-S136 can also be selected. In addition, residue positions C-terminal to G136 (E137-D142), or residue positions adjacent or within α-helix AH2 (K143-A150, preceding the first beta-strand) can be suitable crossover residue positions. Therefore, a number of different crossover residue positions are contemplated herein, where the crossover residue may be positioned after G121 of theJAR 3/5 epitope (G121) through and including A174 of theJAR 11 epitope, where the presence of theJAR 3/5 epitope can be assessed using immunoassay methods known in the art, (Note that numbering above is based on the amino acid sequence number of the fHBP reference sequence of MC58.) -
Figure 33 shows a Western blot of samples of N. meningitidis expressing either wildtype (WT) or a chimeric fHBP (Chimera I (seeFig. 23 )). The Chimera I corresponded to a full-length fHBP and further included the signal sequence (but lacked any epitope tags, such as a Penta-His tag) As shown inFigure 33 , bacterial cells transformed with the plasmid containing the gene encoding Chimera I were positive for both anti-fHbp mAbs, whereas the cells from H44/76 transformed with the plasmid containing the gene encoding fHbp v.2 or WT H44/76 react only with JAR 3 (v.1) and the cells from 8047 react only with JAR 13 (v.2). - Hybridomas producing the
JAR 4,JAR 5,JAR 11, andJAR 32 monoclonal antibodies were deposited under the terms of the Budapest Treaty with the American Type Culture Collection, 10801 University Blvd., Manassas, Va. 20110-2209, USA (ATCC) on the date indicated in the table below, and were assigned the designations set out in the table below.ATCC Deposit No. (Deposit Date) Material Deposited PTA-8943 (Feb. 7, 2008) Hybridoma producing JAR 4 Monoclonal AntibodyPTA-8941 (Feb. 7, 2008) Hybridoma producing JAR 5 Monoclonal AntibodyPTA-8940 (Feb. 7, 2008) Hybridoma producing JAR 10 Monoclonal AntibodyPTA-8938 (Feb. 7, 2008) Hybridoma producing JAR 11 Monoclonal AntibodyPTA-8942 (Feb. 7, 2008) Hybridoma producing JAR 32 Monoclonal AntibodyPTA-8939 (Feb. 7, 2008) Hybridoma producing JAR 33 Monoclonal Antibody - It should be noted that
JAR 5 mAb specifically binds to an epitope that at least overlaps with the epitope specifically bound byJAR 3 mAb, and thatJAR 32 mAb specifically binds to an epitope that at least overlaps with the epitope specifically bounds byJAR 35 mAb. - These deposits were made under the provisions of the Budapest Treaty on the International Recognition of the Deposit of Microorganisms for the Purpose of Patent Procedure and the Regulations there under (Budapest Treaty). This assures maintenance of a viable culture of the deposit for 30 years from the date of deposit and for at least five (5) years after the most recent request for the furnishing of a sample of the deposit received by the depository. The deposits will be made available by ATCC under the terms of the Budapest Treaty, and subject to an agreement between Children's Hospital & Research Center at Oakland and the ATCC (the assignee of the present application) which assures that all restrictions imposed by the depositor on the availability to the public of the deposited material will be irrevocably removed upon the granting of the pertinent U.S. patent, assures permanent and unrestricted availability of the progeny of the culture of the deposit to the public upon issuance of the pertinent U.S. patent or upon laying open to the public of any U.S. or foreign patent application, whichever comes first, and assures availability of the progeny to one determined by the U.S. Commissioner of Patents and Trademarks to be entitled thereto according to 35 U.S.C. § 122 and the Commissioner's rules pursuant thereto (including 37 C.F.R. § 1.14 with particular reference to 886 OG 638).
- The assignee(s) of the present application has agreed that if a culture of the materials on deposit should die or be lost or destroyed when cultivated under suitable conditions, the materials will be promptly replaced on notification with another of the same. Availability of the deposited material is not to be construed as a license to practice the invention in contravention of the rights granted under the authority of any government in accordance with its patent laws.
- The invention is further defined by the following numbered embodiments:
- 1. A chimeric factor H binding protein (fHBP) comprising, from N-terminus to C-terminus:
- a) a heterologous B domain comprising, from N-terminus to C-terminus,
- i) a contiguous N-terminal amino acid sequence of a variant 1 (v.1) factor H Binding Protein (fHBP) B domain; and
- ii) a contiguous C-terminal amino acid sequence of a variant 2 (v.2) fHBP B domain or a variant 3 (v.3) fHBP B domain; and
- b) a C domain operably linked to the heterologous B domain of a), wherein the C domain comprises a contiguous amino acid sequence of a variant 2 (v.2) fHBP C domain or a variant 3 (v.3) fHBP C domain;
JAR 5 monoclonal antibody and specifically binds a monoclonal antibody specific for an epitope of a v.2 or v.3 fHBP C domain. - a) a heterologous B domain comprising, from N-terminus to C-terminus,
- 2. The chimeric fHBP of
embodiment 1, wherein the contiguous N-terminal amino acid sequence of the v. 1 fHBP B domain comprises an amino acid sequence at least 80% identical to the contiguous amino acid sequence of
QSHSALTAFQ TEQIQDSEHS GK (SEQ ID NO: 1),
LTAFQ TEQIQDSEHS GKMVAKRQFR IGDIA,
TEQIQDSEHS GKMVAKRQFR IGDIAGEHTA FNQLPD, or
QSHSALTAFQ TEQIQDSEHS GKMVAKRQFR IGDIAGEHTA FNQLPD. - 3. The chimeric fHBP of
embodiment 2, wherein the amino acid sequence of the heterologous B domain comprises one or more of:- a substitution of leucine (L) for the phenylalanine (F) at
residue position 9 of QSHSALTAFQ TEQIQDSEHS GK (SEQ ID NO: 1); - a substitution of a valine (V) or glutamic acid (E) for isoleucine (I) at
residue position 4 of SEQ ID NO:1; - a substitution of a proline (P) for serine (S) at residue position 17 of SEQ ID NO:1;
- a substitution of an aspartic acid (D) for histidine (H) at residue position 19 of SEQ ID NO:1;
- a substitution of an arginine (R) for glutamine (Q) at
residue position 28 of SEQ ID NO:1; - a substitution of valine (V) for alanine (A) at
residue position 35 of SEQ ID NO:1; - a substitution of glycine (G) for aspartic acid (D) at
residue position 42 of SEQ ID NO:1; and - a substitution of lysine (K) for glutamic acid (E) at
residue position 46 of SEQ ID NO:1.
- a substitution of leucine (L) for the phenylalanine (F) at
- 4. The chimeric fHBP of
embodiment 1, wherein the chimeric fHBP comprises an amino acid sequence of an A domain of a v.1, v.2 or v.3 fHBP positioned N-terminal of and operably linked to the heterologous B domain. - 5. The chimeric fHBP of
embodiment 1, wherein the chimeric fHBP comprises at least one epitope that when bound by an antibody blocks binding of fH to fHBP. - 6. The chimeric fHBP of
embodiment 1, wherein the chimeric fHBP comprises a pair of epitopes that elicit antibodies that, when bound to their respective epitopes, exhibit bactericidal activity. - 7. The chimeric fHBP of
embodiment 6, wherein the pair of epitopes is aJAR 10 monoclonal antibody epitope and aJAR 11 monoclonal antibody epitope. - 8. The chimeric fHBP of
embodiment 6, wherein the pair of epitopes is aJAR 33 monoclonal antibody epitope and aJAR 35 monoclonal antibody epitope. - 9. A chimeric factor H binding protein (fHBP) comprising, from N-terminus to C-terminus:
- a) a first amino acid sequence at least 80% identical to a contiguous amino acid sequence of a variant 1 (v.1) factor H binding protein (fHBP) B domain comprising the amino acid sequence QSHSALTAFQ TEQIQDSEHS GK (SEQ ID NO: 1); and
- b) operably linked to a), a second amino acid sequence at least 80% identical to a contiguous amino acid sequence of a variant 2 (v.2) or variant 3 (v.3) fHBP;
wherein the first and second amino acid sequences are operably linked at a junction point positioned within a B domain or a C domain of the chimeric fHBP;
wherein the chimeric specifically binds a monoclonal antibody specific for an epitope of a v.2 or v.3 fHBP C domain.
- 10. The chimeric fHBP of
embodiment 9, wherein the junction point is positioned within the B domain such that the chimeric fHBP comprises a heterologous B domain. - 11. The chimeric fHBP of
embodiment 9, wherein the junction point is positioned within the C domain such that the chimeric fHBP comprises a heterologous C domain. - 12. The chimeric fHBP of
embodiment 9, wherein the second amino acid sequence is greater than 80% identical to a contiguous amino acid sequence of a v.2 fHBP and the junction point is positioned at a site following the lysine of SEQ ID NO: 1 of the first amino acid sequence and prior to a residue defining aJAR 11 monoclonal antibody epitope. - 13. The chimeric fHBP of
embodiment 9, wherein the second amino acid sequence is greater than 80% identical to a contiguous amino acid sequence of a v.3 fHBP and the junction point is positioned at a site following the lysine of SEQ ID NO: 1 of the first amino acid sequence and prior to a residue defining aJAR 32 monoclonal antibody epitope. - 14. The chimeric fHBP of
embodiment 9, wherein the junction point is positioned within the B domain adjacent or within the second alpha helix. - 15. The chimeric fHBP of
embodiment 14, wherein the junction point is positioned C-terminal of the amino acid sequence GEHT of the B domain. - 16. The chimeric fHBP of
embodiment 9, wherein the junction point is positioned at a site that is not more than 14 residues N-terminal of the amino acid sequence GEHT. - 17. The chimeric fHBP of
embodiment 9, wherein the junction point is positioned at site not more than 34 residues C-terminal of the amino acid sequence GEHT. - 18. The chimeric fHBP of
embodiment 9, wherein the junction point is positioned so as to provide a heterologous B domain comprising an amino acid sequence at least 80% identical to the amino acid sequence TEQIQDSEHS GKMVAKRQFR IGDIAGEHTA FNQLPD. - 19. The chimeric fHBP of
embodiment 9, wherein the chimeric fHBP comprises a heterologous B domain comprising an amino acid sequence at least 80% identical to the amino acid sequence
QSHSALTAFQ TEQIQDSEHS GKMVAKRQFR IGDIAGEHTA FNQLPD. - 20. The chimeric fHBP of
embodiment 9, wherein the junction point is positioned such that the chimeric fHBP comprises a heterologous C domain, wherein the heterologous C domain comprises an N-terminal amino acid sequence of KLTYTIDFA. - 21. The chimeric fHBP of
embodiment 9, wherein the chimeric fHBP comprises at least one epitope that elicits an antibody that blocks binding of fH to fHBP. - 22. The chimeric fHBP of
embodiment 9, wherein the chimeric fHBP comprises a pair of epitopes that elicit antibody pairs that, when bound to their respective epitopes, exhibit bactericidal activity. - 23. The chimeric fHBP of embodiment 22, wherein the pair of epitopes is a
JAR 10 monoclonal antibody epitope and aJAR 11 monoclonal antibody epitope. - 24. The chimeric fHBP of embodiment 22, wherein the pair of epitopes is a
JAR 33 monoclonal antibody epitope and aJAR 35 monoclonal antibody epitope. - 25. The chimeric fHBP of
embodiment 9, wherein the chimeric fHBP comprises an amino acid sequence of an A domain of a v.1, v.2 or v.3 fHBP positioned N-terminal of and operably linked to the heterologous B domain. - 26. A nucleic acid encoding the chimeric fHBP of
embodiment 1. - 27. A nucleic acid encoding the chimeric fHBP of
embodiment 9. - 28. A recombinant host cell containing the nucleic acid of embodiment 26.
- 29. A recombinant host cell containing the nucleic acid of
embodiment 27. - 30. A method of producing a chimeric fHBP, the method comprising: culturing the recombinant host cell of
embodiment 28 under conditions suitable for expression of the chimeric fHBP; and isolating the chimeric fHBP. - 31. A method of producing a chimeric fHBP, the method comprising: culturing the recombinant host cell of embodiment 29 under conditions suitable for expression of the chimeric fHBP; and isolating the chimeric fHBP.
- 32. An immunogenic composition comprising a chimeric fHBP according to
embodiment 1, and a pharmaceutically acceptable excipient. - 33. The immunogenic composition of
embodiment 32, wherein the chimeric fHBP is in a vesicle preparation prepared from a Neisseria meningitidis strain. - 34. An immunogenic composition comprising a chimeric fHBP according to
embodiment 9, and a pharmaceutically acceptable excipient. - 35. The immunogenic composition of embodiment 34, wherein the chimeric fHBP is in a vesicle preparation prepared from a Neisseria meningitidis strain.
- 36. A method of eliciting an antibody response in a mammal, the method comprising administering to a mammal a chimeric fHBP according to
embodiment 1. - 37. The method of
embodiment 36, wherein the mammal is a human. - 38. The method of embodiment 37, wherein said administering provides for production of antibodies that bind a factor H binding protein (fHBP) of a
variant 1 N. meningitidis strain and that bind a fHBP of avariant 2 N. meningitidis strain. - 39. A method of eliciting an antibody response in a mammal, the method comprising administering to a mammal a chimeric fHBP according to
embodiment 9. - 40. The method of embodiment 39, wherein the mammal is a human.
- 41. The method of embodiment 39, wherein said administering provides for production of antibodies that bind a factor H binding protein (fHBP) of a
variant 1 N. meningitidis strain and that bind a fHBP of avariant 2 N. meningitidis strain.
Claims (14)
- A chimeric factor H binding protein (fHbp) comprising, from N-terminus to C-terminus:a) a first amino acid sequence at least 80% identical to a contiguous amino acid sequence of a variant 1 (v.1) factor H binding protein (fHbp) comprising the amino acid sequence; andb) operably linked to a), a second amino acid sequence at least 80% identical to a contiguous amino acid sequence of a variant 2 (v.2) or variant 3 (v.3) fHbp;
wherein the first and second amino acid sequences are operably linked at a junction point positioned within a B domain, to provide a heterologous B domain, or within a C domain, to provide a heterologous C domain, of the chimeric fHbp;
wherein the chimeric specifically binds a monoclonal antibody specific for an epitope of a v.2 or v.3 fHbp C domain. - The chimeric factor H binding protein (fHbp) of claim 1 comprising:a) a heterologous B domain comprising, from N-terminus to C-terminus,i) a contiguous N-terminal amino acid sequence of a variant 1 (v.1) factor H Binding Protein (fHbp) B domain; andii) a contiguous C-terminal amino acid sequence of a variant 2 (v.2) fHbp B domain or a variant 3 (v.3) fHbp B domain; andb) a C domain operably linked to the heterologous B domain of a), wherein the C domain comprises a contiguous amino acid sequence of a variant 2 (v.2) fHbp C domain or a variant 3 (v.3) fHbp C domain;
wherein the chimeric fHbp comprises the epitope bound by the JAR 5 antibody (ATCC PTA-8941). - The chimeric fHbp of claim 1 or 2, wherein the contiguous amino acid sequence of the v.1 fHbp B domain comprises an amino acid sequence at least 80% identical to the contiguous amino acid sequence of
QSHSALTAFQ TEQIQDSEHS GK,
LTAFQ TEQIQDSEHS GKMVAKRQFR IGDIA,
TEQIQDSEHS GKMVAKRQFR IGDIAGEHTA FNQLPD, or
QSHSALTAFQ TEQIQDSEHS GKMVAKRQFR IGDIAGEHTA FNQLPD. - The chimeric fHbp of claim 3, wherein the amino acid sequence of the heterologous B domain comprises one or more of:a substitution of leucine (L) for the phenylalanine (F) at residue position 9 of QSHSALTAFQ TEQIQDSEHS GK;a substitution of a valine (V) or glutamic acid (E) for isoleucine (I) at residue position 4 of QSHSALTAFQ TEQIQDSEHS GK;a substitution of a proline (P) for serine (S) at residue position 17 of QSHSALTAFQ TEQIQDSEHS GK;a substitution of an aspartic acid (D) for histidine (H) at residue position 19 of QSHSALTAFQ TEQIQDSEHS GK;a substitution of an arginine (R) for glutamine (Q) at residue position 28 of the sequence QSHSALTAFQ TEQIQDSEHS GKMVAKRQFR IGDIAGEHTA FNQLPD; anda substitution of valine (V) for alanine (A) at residue position 35 of the sequence QSHSALTAFQ TEQIQDSEHS GKMVAKRQFR IGDIAGEHTA FNQLPD.
- The chimeric fHbp of any one of claims 1-4, wherein the chimeric fHbp comprises an amino acid sequence of an A domain of a v.1, v.2 or v.3 fHbp positioned N-terminal of and operably linked to the heterologous B domain.
- The chimeric fHbp of any one of claims 1-5, wherein the chimeric fHbp comprises at least one epitope that when bound by an antibody blocks binding of fH to fHbp.
- The chimeric fHbp of any one of claims 1-6, wherein the chimeric fHbp comprises a pair of epitopes that elicit antibodies that, when bound to their respective epitopes, exhibit bactericidal activity.
- The chimeric fHbp of claim 7, wherein the pair of epitopes is the epitope bound by the JAR 10 antibody (ATCC PTA-8940) and the epitope bound by the JAR 11 antibody (ATCC PTA-8938) or the pair of epitopes is the epitope bound by the JAR 33 antibody (ATCC PTA-8939) and the epitope bound by the JAR 32 antibody (ATCC PTA-8942).
- A nucleic acid encoding the chimeric fHbp of any one of the preceding claims.
- A recombinant host cell containing the nucleic acid of claim 9.
- A method of producing a chimeric fHbp, the method comprising:culturing the recombinant host cell of claim 10 under conditions suitable for expression of the chimeric fHbp; andisolating the chimeric fHbp.
- An immunogenic composition comprising a chimeric fHbp according to any one of claims 1-8, and a pharmaceutically acceptable excipient.
- The immunogenic composition of claim 12, wherein the chimeric fHbp is in a vesicle preparation prepared from a Neisseria meningitidis strain.
- A chimeric fHbp according to any one of claims 1-8, or composition of claims 12 or 13, for use in a method of vaccination of a mammal.
Applications Claiming Priority (3)
| Application Number | Priority Date | Filing Date | Title |
|---|---|---|---|
| US3532908P | 2008-03-10 | 2008-03-10 | |
| US3725208P | 2008-03-17 | 2008-03-17 | |
| EP09720813.6A EP2265640B1 (en) | 2008-03-10 | 2009-03-09 | Chimeric factor h binding proteins (fhbp) containing a heterologous b domain and methods of use |
Related Parent Applications (2)
| Application Number | Title | Priority Date | Filing Date |
|---|---|---|---|
| EP09720813.6 Division | 2009-03-09 | ||
| EP09720813.6A Division-Into EP2265640B1 (en) | 2008-03-10 | 2009-03-09 | Chimeric factor h binding proteins (fhbp) containing a heterologous b domain and methods of use |
Publications (1)
| Publication Number | Publication Date |
|---|---|
| EP2631245A1 true EP2631245A1 (en) | 2013-08-28 |
Family
ID=41065783
Family Applications (2)
| Application Number | Title | Priority Date | Filing Date |
|---|---|---|---|
| EP09720813.6A Not-in-force EP2265640B1 (en) | 2008-03-10 | 2009-03-09 | Chimeric factor h binding proteins (fhbp) containing a heterologous b domain and methods of use |
| EP13154049.4A Withdrawn EP2631245A1 (en) | 2008-03-10 | 2009-03-09 | Chimeric factor H binding proteins (fHBP) containing a heterologous B domain and methods of use |
Family Applications Before (1)
| Application Number | Title | Priority Date | Filing Date |
|---|---|---|---|
| EP09720813.6A Not-in-force EP2265640B1 (en) | 2008-03-10 | 2009-03-09 | Chimeric factor h binding proteins (fhbp) containing a heterologous b domain and methods of use |
Country Status (6)
| Country | Link |
|---|---|
| US (1) | US9511131B2 (en) |
| EP (2) | EP2265640B1 (en) |
| AU (1) | AU2009223613B2 (en) |
| CA (1) | CA2717870A1 (en) |
| ES (1) | ES2557282T3 (en) |
| WO (1) | WO2009114485A2 (en) |
Families Citing this family (37)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| BR9910089A (en) | 1998-05-01 | 2004-06-08 | Chiron Corp | Compositions and antigens of neisseria meningitidis |
| WO2000071725A2 (en) | 1999-05-19 | 2000-11-30 | Chiron S.P.A. | Combination neisserial compositions |
| AU784203B2 (en) | 1999-10-29 | 2006-02-23 | Glaxosmithkline Biologicals S.A. | Neisserial antigenic peptides |
| RU2299906C2 (en) | 2000-02-28 | 2007-05-27 | Новартис Вэксинс Энд Диагностикс С.Р.Л. | Heterologous expression of neisseria proteins |
| GB0118249D0 (en) | 2001-07-26 | 2001-09-19 | Chiron Spa | Histidine vaccines |
| GB0121591D0 (en) | 2001-09-06 | 2001-10-24 | Chiron Spa | Hybrid and tandem expression of neisserial proteins |
| MX339524B (en) | 2001-10-11 | 2016-05-30 | Wyeth Corp | Novel immunogenic compositions for the prevention and treatment of meningococcal disease. |
| GB0227346D0 (en) | 2002-11-22 | 2002-12-31 | Chiron Spa | 741 |
| GB0408977D0 (en) | 2004-04-22 | 2004-05-26 | Chiron Srl | Immunising against meningococcal serogroup Y using proteins |
| GB0524066D0 (en) | 2005-11-25 | 2006-01-04 | Chiron Srl | 741 ii |
| WO2009038889A1 (en) * | 2007-08-02 | 2009-03-26 | Children's Hospital And Research Center At Oakland | Fhbp- and lpxl1-based vesicle vaccines for broad spectrum protection against diseases caused by neisseria meningitidis |
| US9579372B2 (en) * | 2008-02-21 | 2017-02-28 | Glaxosmithkline Biologicals Sa | Meningococcal fHBP polypeptides |
| AU2009288095A1 (en) | 2008-09-03 | 2010-03-11 | Children's Hospital & Research Center At Oakland | Peptides presenting an epitope of a domain of factor H binding protein and methods of use |
| CA2756522C (en) | 2009-03-24 | 2018-06-26 | Novartis Ag | Adjuvanting meningococcal factor h binding protein |
| AU2010302344A1 (en) | 2009-09-30 | 2012-04-26 | Novartis Ag | Expression of meningococcal fhbp polypeptides |
| JP2013521327A (en) * | 2010-03-10 | 2013-06-10 | グラクソスミスクライン バイオロジカルズ ソシエテ アノニム | Immunogenic composition |
| ES2910199T3 (en) | 2010-03-30 | 2022-05-11 | Childrens Hospital & Res Center At Oakland | Factor H-binding proteins (fHbp) with altered properties and methods of using them |
| CA2803239A1 (en) | 2010-06-25 | 2011-12-29 | Novartis Ag | Combinations of meningococcal factor h binding proteins |
| HRP20240965T1 (en) | 2010-08-23 | 2024-10-25 | Wyeth Llc | Stable formulations of neisseria meningitidis rlp2086 antigens |
| PE20140173A1 (en) | 2010-09-10 | 2014-02-20 | Wyeth Llc | NON-LIPIDED VARIANTS OF NEISSERIA MENINGITIDIS ANTIGENS ORF2086 |
| EP2809785B1 (en) | 2012-02-02 | 2017-11-01 | GlaxoSmithKline Biologicals SA | Promoters for increased protein expression in meningococcus |
| SG10201602558UA (en) | 2012-03-09 | 2016-05-30 | Pfizer | Neisseria meningitidis compositions and methods thereof |
| SA115360586B1 (en) | 2012-03-09 | 2017-04-12 | فايزر انك | Neisseria meningitidis compositions and methods thereof |
| MX357538B (en) | 2012-06-14 | 2018-07-13 | Novartis Ag | Vaccines for serogroup x meningococcus. |
| CN104736563A (en) | 2012-07-27 | 2015-06-24 | 国家健康与医学研究院 | Cd147 as receptor for pilus-mediated adhesion of meningococci to vascular endothelia |
| GB201215005D0 (en) * | 2012-08-23 | 2012-10-10 | Isis Innovation | Stabilised meningitis vaccine |
| US9802987B2 (en) | 2013-03-08 | 2017-10-31 | Pfizer Inc. | Immunogenic fusion polypeptides |
| CN105431167A (en) | 2013-08-02 | 2016-03-23 | 奥克兰儿童医院及研究中心 | Non-naturally occurring factor h binding proteins (FHBP) and methods of use thereof |
| WO2015033251A2 (en) | 2013-09-08 | 2015-03-12 | Pfizer Inc. | Neisseria meningitidis compositions and methods thereof |
| RU2714248C2 (en) * | 2014-07-23 | 2020-02-13 | Чилдрен'З Хоспитал Энд Рисёрч Сентер Эт Окленд | Versions of factor n-binding protein and methods of use thereof |
| MX2017010705A (en) | 2015-02-19 | 2017-12-04 | Pfizer | Neisseria meningitidis compositions and methods thereof. |
| CA2987306A1 (en) * | 2015-06-02 | 2016-12-08 | De Staat Der Nederlanden, Vert. Door De Minister Van Vws, Ministerie Van Volksgezondheid, Welzijn En Sport | Surface display of antigens on gram-negative outer membrane vesicles |
| BR112018016322A2 (en) | 2016-02-10 | 2019-01-22 | Eng Antigens Inc | polynucleotides and slam polypeptides and their uses |
| GB201614687D0 (en) * | 2016-08-31 | 2016-10-12 | Univ Oxford Innovation Ltd | fHbp scaffold |
| SG11201906519RA (en) | 2017-01-31 | 2019-08-27 | Pfizer | Neisseria meningitidis compositions and methods thereof |
| CN110804101A (en) * | 2019-11-08 | 2020-02-18 | 苏州微超生物科技有限公司 | Group B meningococcus related fusion protein, vaccine, preparation method and application thereof |
| CN110804102B (en) * | 2019-11-08 | 2021-07-20 | 苏州微超生物科技有限公司 | Group B meningococcal vaccine, and preparation method and application thereof |
Citations (33)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| US4235871A (en) | 1978-02-24 | 1980-11-25 | Papahadjopoulos Demetrios P | Method of encapsulating biologically active materials in lipid vesicles |
| US4501728A (en) | 1983-01-06 | 1985-02-26 | Technology Unlimited, Inc. | Masking of liposomes from RES recognition |
| US4837028A (en) | 1986-12-24 | 1989-06-06 | Liposome Technology, Inc. | Liposomes with enhanced circulation time |
| GB2220221A (en) | 1988-07-02 | 1990-01-04 | Bkl Extrusions Ltd | Glazing bead |
| WO1990014837A1 (en) | 1989-05-25 | 1990-12-13 | Chiron Corporation | Adjuvant formulation comprising a submicron oil droplet emulsion |
| EP0689454A1 (en) | 1993-03-23 | 1996-01-03 | Smithkline Beecham Biolog | Vaccine compositions containing 3-o deacylated monophosphoryl lipid a |
| WO1996002555A1 (en) | 1994-07-15 | 1996-02-01 | The University Of Iowa Research Foundation | Immunomodulatory oligonucleotides |
| EP0735898A1 (en) | 1993-12-23 | 1996-10-09 | SMITHKLINE BEECHAM BIOLOGICALS s.a. | Vaccines |
| EP0761231A1 (en) | 1992-06-25 | 1997-03-12 | SMITHKLINE BEECHAM BIOLOGICALS s.a. | Vaccine composition containing adjuvants |
| EP0835318A2 (en) | 1995-06-29 | 1998-04-15 | SMITHKLINE BEECHAM BIOLOGICALS s.a. | Vaccines against hepatitis c |
| WO1998016247A1 (en) | 1996-10-11 | 1998-04-23 | The Regents Of The University Of California | Immunostimulatory polynucleotide/immunomodulatory molecule conjugates |
| WO1998018810A1 (en) | 1996-10-30 | 1998-05-07 | The University Of Iowa Research Foundation | Immunostimulatory nucleic acid molecules |
| WO1998037919A1 (en) | 1997-02-28 | 1998-09-03 | University Of Iowa Research Foundation | USE OF NUCLEIC ACIDS CONTAINING UNMETHYLATED CpG DINUCLEOTIDE IN THE TREATMENT OF LPS-ASSOCIATED DISORDERS |
| WO1998040100A1 (en) | 1997-03-10 | 1998-09-17 | Ottawa Civic Loeb Research Institute | USE OF NUCLEIC ACIDS CONTAINING UNMETHYLATED CpG DINUCLEOTIDE AS AN ADJUVANT |
| WO1998052581A1 (en) | 1997-05-20 | 1998-11-26 | Ottawa Civic Hospital Loeb Research Institute | Vectors and methods for immunization or therapeutic protocols |
| WO1998055495A2 (en) | 1997-06-06 | 1998-12-10 | Dynavax Technologies Corporation | Immunostimulatory oligonucleotides, compositions thereof and methods of use thereof |
| WO1998057659A1 (en) | 1997-06-14 | 1998-12-23 | Smithkline Beecham Biologicals S.A. | Adjuvant compositions for vaccines |
| WO1999011241A1 (en) | 1997-09-05 | 1999-03-11 | Smithkline Beecham Biologicals S.A. | Oil in water emulsions containing saponins |
| WO1999044636A2 (en) | 1998-03-05 | 1999-09-10 | The Medical College Of Ohio | Il-12 enhancement of immune responses to t-independent antigens |
| WO1999052549A1 (en) | 1998-04-09 | 1999-10-21 | Smithkline Beecham Biologicals S.A. | Adjuvant compositions |
| WO1999057280A2 (en) | 1998-05-01 | 1999-11-11 | Chiron Corporation | Neisseria meningitidis antigens and compositions |
| WO2000007621A2 (en) | 1998-08-05 | 2000-02-17 | Smithkline Beecham Biologicals S.A. | Vaccine comprising an iscom consisting of sterol and saponin which is free of additional detergent |
| WO2000023105A2 (en) | 1998-10-16 | 2000-04-27 | Smithkline Beecham Biologicals S.A. | Adjuvant systems and vaccines |
| WO2000056358A2 (en) | 1999-03-19 | 2000-09-28 | Smithkline Beecham Biologicals S.A. | Vaccine against streptococcus pneumoniae capsular polysaccharides |
| WO2000062800A2 (en) | 1999-04-19 | 2000-10-26 | Smithkline Beecham Biologicals Sa | Adjuvant composition comprising saponin and an immunostimulatory oligonucleotide |
| WO2001021207A2 (en) | 1999-09-24 | 2001-03-29 | Smithkline Beecham Biologicals S.A. | Use of combination of polyoxyethylene sorbitan ester and octoxynol as adjuvant and its use in vaccines |
| WO2001021152A1 (en) | 1999-09-24 | 2001-03-29 | Smithkline Beecham Biologicals S.A. | Adjuvant comprising a polyxyethylene alkyl ether or ester and at least one nonionic surfactant |
| WO2001034642A2 (en) | 1999-11-12 | 2001-05-17 | University Of Iowa Research Foundation | Control of neisserial membrane synthesis |
| WO2002009746A2 (en) | 2000-07-31 | 2002-02-07 | Glaxosmithkline Biologicals S.A. | Vaccines comprising outer membrane vesciles from gram negative bacteria |
| WO2002097646A2 (en) | 2001-05-31 | 2002-12-05 | Koninklijke Philips Electronics N.V. | Parallel data communication having skew intolerant data groups |
| WO2004048404A2 (en) | 2002-11-22 | 2004-06-10 | Chiron Srl | Multiple variants of meningococcal protein nmb1870 |
| WO2006024954A2 (en) * | 2004-09-01 | 2006-03-09 | Novartis Vaccines And Diagnostics Srl | Domains and epitopes of meningococcal protein nmb1870 |
| WO2007060548A2 (en) * | 2005-11-25 | 2007-05-31 | Novartis Vaccines And Diagnostics Srl | Chimeric, hybrid and tandem polypeptides of meningococcal nmb1870 |
Family Cites Families (7)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| GB0121591D0 (en) * | 2001-09-06 | 2001-10-24 | Chiron Spa | Hybrid and tandem expression of neisserial proteins |
| NZ555937A (en) | 2005-01-27 | 2009-05-31 | Childrens Hosp & Res Ct Oak | GNA1870-based vesicle vaccines for broad spectrum protection against diseases caused by Neisseria meningitidis |
| US9036015B2 (en) | 2005-11-23 | 2015-05-19 | Koninklijke Philips N.V. | Rendering views for a multi-view display device |
| WO2009038889A1 (en) | 2007-08-02 | 2009-03-26 | Children's Hospital And Research Center At Oakland | Fhbp- and lpxl1-based vesicle vaccines for broad spectrum protection against diseases caused by neisseria meningitidis |
| US8476032B2 (en) | 2008-08-27 | 2013-07-02 | Children's Hospital & Research Center Oakland | Complement factor H-based assays for serum bactericidal activity against Neisseria meningitidis |
| GB0819633D0 (en) | 2008-10-25 | 2008-12-03 | Isis Innovation | Composition |
| ES2910199T3 (en) | 2010-03-30 | 2022-05-11 | Childrens Hospital & Res Center At Oakland | Factor H-binding proteins (fHbp) with altered properties and methods of using them |
-
2009
- 2009-03-09 CA CA2717870A patent/CA2717870A1/en not_active Abandoned
- 2009-03-09 EP EP09720813.6A patent/EP2265640B1/en not_active Not-in-force
- 2009-03-09 US US12/921,123 patent/US9511131B2/en active Active
- 2009-03-09 EP EP13154049.4A patent/EP2631245A1/en not_active Withdrawn
- 2009-03-09 ES ES09720813.6T patent/ES2557282T3/en active Active
- 2009-03-09 WO PCT/US2009/036577 patent/WO2009114485A2/en active Application Filing
- 2009-03-09 AU AU2009223613A patent/AU2009223613B2/en not_active Ceased
Patent Citations (33)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| US4235871A (en) | 1978-02-24 | 1980-11-25 | Papahadjopoulos Demetrios P | Method of encapsulating biologically active materials in lipid vesicles |
| US4501728A (en) | 1983-01-06 | 1985-02-26 | Technology Unlimited, Inc. | Masking of liposomes from RES recognition |
| US4837028A (en) | 1986-12-24 | 1989-06-06 | Liposome Technology, Inc. | Liposomes with enhanced circulation time |
| GB2220221A (en) | 1988-07-02 | 1990-01-04 | Bkl Extrusions Ltd | Glazing bead |
| WO1990014837A1 (en) | 1989-05-25 | 1990-12-13 | Chiron Corporation | Adjuvant formulation comprising a submicron oil droplet emulsion |
| EP0761231A1 (en) | 1992-06-25 | 1997-03-12 | SMITHKLINE BEECHAM BIOLOGICALS s.a. | Vaccine composition containing adjuvants |
| EP0689454A1 (en) | 1993-03-23 | 1996-01-03 | Smithkline Beecham Biolog | Vaccine compositions containing 3-o deacylated monophosphoryl lipid a |
| EP0735898A1 (en) | 1993-12-23 | 1996-10-09 | SMITHKLINE BEECHAM BIOLOGICALS s.a. | Vaccines |
| WO1996002555A1 (en) | 1994-07-15 | 1996-02-01 | The University Of Iowa Research Foundation | Immunomodulatory oligonucleotides |
| EP0835318A2 (en) | 1995-06-29 | 1998-04-15 | SMITHKLINE BEECHAM BIOLOGICALS s.a. | Vaccines against hepatitis c |
| WO1998016247A1 (en) | 1996-10-11 | 1998-04-23 | The Regents Of The University Of California | Immunostimulatory polynucleotide/immunomodulatory molecule conjugates |
| WO1998018810A1 (en) | 1996-10-30 | 1998-05-07 | The University Of Iowa Research Foundation | Immunostimulatory nucleic acid molecules |
| WO1998037919A1 (en) | 1997-02-28 | 1998-09-03 | University Of Iowa Research Foundation | USE OF NUCLEIC ACIDS CONTAINING UNMETHYLATED CpG DINUCLEOTIDE IN THE TREATMENT OF LPS-ASSOCIATED DISORDERS |
| WO1998040100A1 (en) | 1997-03-10 | 1998-09-17 | Ottawa Civic Loeb Research Institute | USE OF NUCLEIC ACIDS CONTAINING UNMETHYLATED CpG DINUCLEOTIDE AS AN ADJUVANT |
| WO1998052581A1 (en) | 1997-05-20 | 1998-11-26 | Ottawa Civic Hospital Loeb Research Institute | Vectors and methods for immunization or therapeutic protocols |
| WO1998055495A2 (en) | 1997-06-06 | 1998-12-10 | Dynavax Technologies Corporation | Immunostimulatory oligonucleotides, compositions thereof and methods of use thereof |
| WO1998057659A1 (en) | 1997-06-14 | 1998-12-23 | Smithkline Beecham Biologicals S.A. | Adjuvant compositions for vaccines |
| WO1999011241A1 (en) | 1997-09-05 | 1999-03-11 | Smithkline Beecham Biologicals S.A. | Oil in water emulsions containing saponins |
| WO1999044636A2 (en) | 1998-03-05 | 1999-09-10 | The Medical College Of Ohio | Il-12 enhancement of immune responses to t-independent antigens |
| WO1999052549A1 (en) | 1998-04-09 | 1999-10-21 | Smithkline Beecham Biologicals S.A. | Adjuvant compositions |
| WO1999057280A2 (en) | 1998-05-01 | 1999-11-11 | Chiron Corporation | Neisseria meningitidis antigens and compositions |
| WO2000007621A2 (en) | 1998-08-05 | 2000-02-17 | Smithkline Beecham Biologicals S.A. | Vaccine comprising an iscom consisting of sterol and saponin which is free of additional detergent |
| WO2000023105A2 (en) | 1998-10-16 | 2000-04-27 | Smithkline Beecham Biologicals S.A. | Adjuvant systems and vaccines |
| WO2000056358A2 (en) | 1999-03-19 | 2000-09-28 | Smithkline Beecham Biologicals S.A. | Vaccine against streptococcus pneumoniae capsular polysaccharides |
| WO2000062800A2 (en) | 1999-04-19 | 2000-10-26 | Smithkline Beecham Biologicals Sa | Adjuvant composition comprising saponin and an immunostimulatory oligonucleotide |
| WO2001021207A2 (en) | 1999-09-24 | 2001-03-29 | Smithkline Beecham Biologicals S.A. | Use of combination of polyoxyethylene sorbitan ester and octoxynol as adjuvant and its use in vaccines |
| WO2001021152A1 (en) | 1999-09-24 | 2001-03-29 | Smithkline Beecham Biologicals S.A. | Adjuvant comprising a polyxyethylene alkyl ether or ester and at least one nonionic surfactant |
| WO2001034642A2 (en) | 1999-11-12 | 2001-05-17 | University Of Iowa Research Foundation | Control of neisserial membrane synthesis |
| WO2002009746A2 (en) | 2000-07-31 | 2002-02-07 | Glaxosmithkline Biologicals S.A. | Vaccines comprising outer membrane vesciles from gram negative bacteria |
| WO2002097646A2 (en) | 2001-05-31 | 2002-12-05 | Koninklijke Philips Electronics N.V. | Parallel data communication having skew intolerant data groups |
| WO2004048404A2 (en) | 2002-11-22 | 2004-06-10 | Chiron Srl | Multiple variants of meningococcal protein nmb1870 |
| WO2006024954A2 (en) * | 2004-09-01 | 2006-03-09 | Novartis Vaccines And Diagnostics Srl | Domains and epitopes of meningococcal protein nmb1870 |
| WO2007060548A2 (en) * | 2005-11-25 | 2007-05-31 | Novartis Vaccines And Diagnostics Srl | Chimeric, hybrid and tandem polypeptides of meningococcal nmb1870 |
Non-Patent Citations (84)
| Title |
|---|
| "Remington's Pharmaceutical Science", 1980, MACK PUBLISHING COMPAN |
| "Short Protocols in Molecular Biology", 1999, WILEY & SONS |
| "Vaccine", 1995, PLENUM PRESS |
| ADU-BOBIE ET AL., INFECT IMMUN., vol. 72, 2004, pages 1914 - 1919 |
| ALTSCHUL ET AL., J. MOL. BIOL., vol. 215, 1990, pages 403 - 410 |
| ALTSCHUL ET AL., NUCLEIC ACIDS RES., vol. 25, 1977, pages 3389 - 3402 |
| ANDERSSON ET AL., J. IMMUNOLOGICAL METHODS, vol. 255, no. 1-2, 2001, pages 135 - 48 |
| BALLAS ET AL., J. IMMUNOL, vol. 157, 1996, pages 1840 - 1845 |
| BEERNINK ET AL., INFECT IMMUN, vol. 76, 2008, pages 4232 - 4240 |
| BEERNINK ET AL., J INFECT DIS, vol. 195, 2007, pages 1472 - 9 |
| BEERNINK PETER T ET AL: "Bactericidal antibody responses induced by meningococcal recombinant chimeric factor H-binding protein vaccines", INFECTION AND IMMUNITY, AMERICAN SOCIETY FOR MICROBIOLOGY, WASHINGTON, US, vol. 76, no. 6, 1 June 2008 (2008-06-01), pages 2568 - 2575, XP002534267, ISSN: 0019-9567 * |
| BEERNINK PETER T ET AL: "Rapid genetic grouping of factor h-binding protein (genome-derived neisserial antigen 1870), a promising group B meningococcal vaccine candidate", CLINICAL AND VACCINE IMMUNOLOGY, AMERICAN SOCIETY FOR MICROBIOLOGY, WASHINGTON, DC, US, vol. 13, no. 7, 1 July 2006 (2006-07-01), pages 758 - 763, XP002534266, ISSN: 1556-6811 * |
| BORROW ET AL., INFECT IMMUN., vol. 69, 2001, pages 1568 |
| CANTINI ET AL., J BIOL CHEM, 2009 |
| CANTINI ET AL., J BIOL CHEM, vol. 281, 2006, pages 7220 - 7 |
| CANTINI ET AL., J. BIOL. CHEM., 2009 |
| CANTINI ET AL.: "Solution structure of the immunodominant domain of protective antigen GNA1870 of Neisseria meningitidis", J BIOL CHEM, vol. 281, 2006, pages 7220 - 7, XP002547101, DOI: doi:10.1074//JBC.M508595200 |
| CHU ET AL., J. EXP. MED, vol. 186, 1997, pages 1623 - 1631 |
| COWDERY ET AL., J. IMMUNOL, vol. 156, 1996, pages 4570 - 4575 |
| DAVIS ET AL., J. IMMUNOL, vol. 160, 1998, pages 810 - 876 |
| DOLAN-LIVENGOOD ET AL., J. INFECT. DIS., vol. 187, no. 10, 2003, pages 1616 - 28 |
| EARNHART ET AL., VACCINE, vol. 25, 2007, pages 466 - 80 |
| FISSEHA ET AL., INFECT. IMMUN., vol. 73, no. 7, 2005, pages 4070 - 4080 |
| FISSHA ET AL., INFECT IMMUN, vol. 73, 2005, pages 4070 |
| FLETCHER ET AL., INFECT IMMUN, 2004, pages 2088 - 2100 |
| FLETCHER ET AL., INFECT IMMUN, vol. 72, 2004, pages 2088 - 2100 |
| FLETCHER ET AL., INFECT IMMUN., vol. 72, 2004, pages 2088 - 100 |
| FLETCHER ET AL., INFECTION AND IMMUNITY, vol. 72, no. 4, 2004, pages 2088 - 100 |
| FRASCH, C. E.; CHAPMAN, J. INFECT. DIS., vol. 127, 1973, pages 149 - 154 |
| FROSCH ET AL., MOL MICROBIOL., vol. 4, no. 7, 1990, pages 1215 - 1218 |
| GIULIANI ET AL., INFECT IMMUN, vol. 73, 2005, pages 1151 - 60 |
| GIULIANI ET AL., INFECT. IMMUN, vol. 73, 2005, pages 1151 - 60 |
| GIULIANI ET AL., PROC NATL ACAD SCI U S A, vol. 103, 2006, pages 10834 - 9 |
| GIULIANI ET AL.: "The region comprising amino acids 100 to 255 of Neisseria meningitidis lipoprotein GNA 1870 elicits bactericidal antibodies", INFECT IMMUN, vol. 73, 2005, pages 1151 - 60, XP002384460, DOI: doi:10.1128/IAI.73.2.1151-1160.2005 |
| GIULIANI M M ET AL: "The region comprising amino acids 100 to 255 of Neisseria meningitidis lipoprotein GNA 1870 elicits bactericidal antibodies", INFECTION AND IMMUNITY, AMERICAN SOCIETY FOR MICROBIOLOGY, WASHINGTON, US, vol. 73, no. 2, 1 February 2005 (2005-02-01), pages 1151 - 1160, XP002384460, ISSN: 0019-9567 * |
| GIULIANI, INFECT IMMUN, vol. 73, 2005, pages 1151 - 60 |
| GIULIANI, INFECT. IMMUN., vol. 73, 2005, pages 1151 - 1160 |
| GOLDSCHNEIDER ET AL., J. EXP. MED., vol. 129, 1969, pages 1307 |
| GUNN J. S.; KHENG, B. L.; KRUEGER J.; KIM K.; GUO L.; HACKETT M.; MILLER S. I., MOL. MICROBIOL., vol. 27, 1998, pages 1171 - 1182 |
| HALPERN ET AL., CELL IMMUNOL, vol. 167, 1996, pages 72 - 78 |
| HIGGINS D ET AL., NUCLEIC ACIDS RES, vol. 22, 1994, pages 4673 - 4680 |
| KLINMAN ET AL., PNAS USA, vol. 93, 1996, pages 2879 - 2883 |
| KOEBERLING ET AL., J INFECT DIS, vol. 198, 2008, pages 262 - 270 |
| KRIEG CURR OPIN MOL THER, vol. 3, 2001, pages 15 - 24 |
| KRIEG ET AL., NATURE, vol. 374, 1995, pages 546 - 549 |
| KRIEG VACCINE, vol. 19, 2000, pages 618 - 622 |
| LIPFORD ET AL., EAR. J. IMMUNOL., vol. 27, 1997, pages 2340 - 2344 |
| MADICO ET AL., J IMMUNOL, vol. 177, 2006, pages 501 - 10 |
| MAIDEN ET AL., PROC. NATL. ACAD. SCI. USA, vol. 95, 1998, pages 3140 |
| MASIGNANI ET AL., J EXP MED, vol. 197, 2003, pages 789 - 799 |
| MASIGNANI ET AL., J EXP MED, vol. 197, 2003, pages 789 - 99 |
| MASIGNANI ET AL., J. EXP. MED., 2003 |
| MESSINA ET AL., J. IMMUNOL, vol. 147, 1991, pages 1759 - 1764 |
| MOE ET AL., INFECT. IMMUN., vol. 67, 1999, pages 5664 |
| MOLDOVEAMI, VACCINE, vol. 16, 1988, pages 1216 - 1224 |
| O'DWYER ET AL., INFECT IMMUN, vol. 72, 2004, pages 6511 - 80 |
| PAGOTTO ET AL., GENE, vol. 244, 2000, pages 13 - 19 |
| PORRO ET AL., PROG CLIN BIOL RES., vol. 397, 1998, pages 315 - 25 |
| ROMAN ET AL., NAT. MED, vol. 3, 1997, pages 849 - 854 |
| RUSSELL ET AL., EMERGING INFECT DIS, vol. 10, 2004, pages 674 - 678 |
| RUSTICI ET AL., SCIENCE, vol. 259, 1993, pages 361 - 365 |
| SACCHI CT ET AL., CLIN DIAGN LAB IMMUNOL, vol. 5, 1998, pages 845 - 55 |
| SACCHI ET AL., CLIN. DIAG. LAB. IMMUNOL., vol. 5, 1998, pages 348 |
| SACCHI ET AL., J. INFECT DIS, vol. 182, 2000, pages 1169 - 1176 |
| SAMBROOK ET AL.: "Molecular Cloning: A Laboratory Manual", 1989, COLD SPRING HARBOR |
| STACEY ET AL., J. IMMUNOL., vol. 157, 1996, pages 2116 - 2122 |
| STEEGHS ET AL., INFECT IMMUN, vol. 67, 1999, pages 4988 - 93 |
| STEEGHS ET AL., J ENDOTOXIN RES, vol. 10, 2004, pages 113 - 9 |
| STEPHENS ET AL., INFECT IMMUN, vol. 59, no. 11, 1991, pages 4097 - 102 |
| SWARTLEY ET AL., J BACTERIOL., vol. 176, no. 5, 1994, pages 1530 - 4 |
| SZOKA ET AL., ANN. REV. BIOPHYS. BIOENG., vol. 9, 1980, pages 467 |
| URWIN ET AL., EPIDEM. AND INFECT., vol. 120, 1998, pages 257 |
| VAN DER LEY ET AL., INFECT IMMUN, vol. 69, 2001, pages 5981 - 90 |
| VAN DER LEY ET AL., PROCEEDINGS OF THE NINTH INTERNATIONAL PATHOGENIC NEISSERIA CONFERENCE, 1994 |
| WEINER ET AL., PNAS USA, vol. 94, 1997, pages 10833 - 10837 |
| WELSCH ET AL., J IMMUNOL, vol. 172, 2004, pages 5606 - 15 |
| WELSCH ET AL., J IMMUNOL, vol. 172, 2004, pages 5606 - 5615 |
| WELSCH ET AL., J IMMUNOL., vol. 172, no. 9, 2004, pages 5606 - 15 |
| WELSCH JO ANNE ET AL: "Complement-dependent synergistic bactericidal activity of antibodies against factor H-binding protein, a sparsely distributed meningococcal vaccine antigen", THE JOURNAL OF INFECTIOUS DISEASES 1 APR 2008,, vol. 197, no. 7, 4 March 2008 (2008-03-04), pages 1053 - 1061, XP002547100 * |
| YAMAMOTO ET AL., JPN. J. CANCER RES., vol. 79, 1988, pages 866 - 873 |
| YI ET AL., J. IMMUNOL, vol. 157, 1996, pages 4918 - 4925 |
| YI ET AL., J. IMMUNOL, vol. 157, 1996, pages 5394 - 5402 |
| YI ET AL., J. IMMUNOL, vol. 160, 1998, pages 4755 - 4761 |
| YI ET AL., J. IMMUNOL, vol. 160, 1998, pages 5898 - 5906 |
Also Published As
| Publication number | Publication date |
|---|---|
| AU2009223613A1 (en) | 2009-09-17 |
| US20120107339A1 (en) | 2012-05-03 |
| US9511131B2 (en) | 2016-12-06 |
| WO2009114485A2 (en) | 2009-09-17 |
| EP2265640B1 (en) | 2015-11-04 |
| CA2717870A1 (en) | 2009-09-17 |
| EP2265640A2 (en) | 2010-12-29 |
| ES2557282T3 (en) | 2016-01-25 |
| WO2009114485A3 (en) | 2010-04-22 |
| AU2009223613B2 (en) | 2014-09-25 |
Similar Documents
| Publication | Publication Date | Title |
|---|---|---|
| EP2265640B1 (en) | Chimeric factor h binding proteins (fhbp) containing a heterologous b domain and methods of use | |
| US10905754B2 (en) | Factor H binding proteins (fHbp) with altered properties and methods of use thereof | |
| US9266942B2 (en) | Chimeric factor H binding proteins (fHbp) and methods of use | |
| US12129282B2 (en) | Factor H binding protein variants and methods of use thereof | |
| US9914756B2 (en) | Non-naturally occurring factor H binding proteins (fHbp) and methods of use thereof |
Legal Events
| Date | Code | Title | Description |
|---|---|---|---|
| PUAI | Public reference made under article 153(3) epc to a published international application that has entered the european phase |
Free format text: ORIGINAL CODE: 0009012 |
|
| AC | Divisional application: reference to earlier application |
Ref document number: 2265640 Country of ref document: EP Kind code of ref document: P |
|
| AK | Designated contracting states |
Kind code of ref document: A1 Designated state(s): AT BE BG CH CY CZ DE DK EE ES FI FR GB GR HR HU IE IS IT LI LT LU LV MC MK MT NL NO PL PT RO SE SI SK TR |
|
| STAA | Information on the status of an ep patent application or granted ep patent |
Free format text: STATUS: THE APPLICATION IS DEEMED TO BE WITHDRAWN |
|
| 18D | Application deemed to be withdrawn |
Effective date: 20140301 |