- Letter to the Editor
- Open access
- Published:
Abnormal pelvic morphology and high cervical length are responsible for high-risk pregnancies in women displaying achondroplasia
Orphanet Journal of Rare Diseases volume 11, Article number: 166 (2016)
Abstract
Pregnancies of women displaying achondroplasia are at high risk of adverse events. Early sonographic assessment of affected women can indicate an unusually long cervical length. It is the consequence of pathological anatomy of the pelvis. Thus, there is a foreseeable dystocia owing to cephalopelvic disproportion. Furthermore, this situation could also complicate cervical ripening prior to fetal extraction.
Dear Editors,
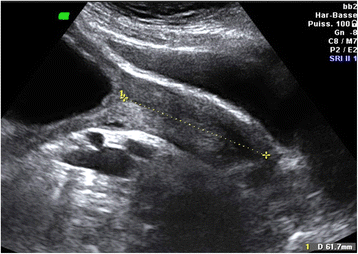
We would like to bring Orphanet Journal of Rare Diseases readers’attention to a specific high-risk pregnancy management. We report the case of a 30-year-old, gravida 1, para 0, with achondroplasia who became spontaneously pregnant. Clinical examination highlighted a pathological anatomy of the pelvis. Pelvic computed tomography showed marked shortening of the obstetric conjugate diameter (5.4 cm) (Fig. 1). In view of the patient’s disease, early sonographic assessment of the fetus was performed. An unusually long cervical length was observed: 61.7 mm at 16 weeks of gestation (Fig. 2). This measurement is way above the 95th centile (49.3 mm) [1].
There are few data on the obstetric management of women with skeletal disorders such as achondroplasia or osteogenesis imperfect [2]. Achondroplasia is a genetic skeletal disorder with a prevalence of close to 1/20,000 pregnancies. It is characterized by a rhizomelic form of dwarfism with a prominent forehead and a low nasal bridge [3]. Although most affected women present premature ovarian failure, their fertility does not seem to be strongly affected, but not all obstetricians are used to managing such pregnancies. First, there is a need for routine cesarean section because of foreseeable dystocia owing to cephalopelvic disproportion. In the case of fetal demise or of termination of pregnancy requested because of an eligible malformation or an affected fetus, the abnormal pelvic morphology and biometry make vaginal delivery impossible when the biparietal diameter exceeds the obstetric conjugate, because of impaction resulting from lumbosacral hyperlordosis. Management of 1st or early 2nd trimester fetal demise is also risky. We noticed that women with achondroplasia have an abnormally high cervical length compared with unaffected women. This special feature, which may protect against preterm delivery, could also complicate cervical ripening prior to fetal extraction. The use of mechanical dilatation by osmotic cervical dilators could be compromised because of the abnormal cervical length, which could easily exceed the length of the mechanical device (impossibility to catheterize the internal orifice). If vacuum suction is planned, ultrasound guidance is needed in order to avoid cervical injury. We think that obstetricians should be aware of the risks associated with this specific pregnancy risk for women with achondroplasia. Termination of pregnancy in such cases warrants specific care to avoid high maternal morbidity.
References
Crispi F, Llurba E, Pedrero C, Carreras E, Higueras T, Hermosilla E, Cabero L, Gratacós E. Gestational age-dependent normal values of ultrasonographic measurement of cervical length in the Spanish population. Prog Obstet Ginecol. 2004;47:264–71.
Carter EM, Davis JG, Raggio CL. Advances in understanding etiology of achondroplasia and review of management. Curr Opin Pediatr. 2007;19:32–7.
Cozzolino M, Perelli F, Maggio L, Coccia ME, Quaranta M, Gizzo S, Mecacci F. Management of osteogenesis imperfecta type I in pregnancy; a review of literature applied to clinical practice. Arch Gynecol Obstet. 2016;293:1153–9.
Acknowledgements
Not applicable.
Funding
No funding.
Availability of data and material
Not applicable.
Authors’ contributions
AGC performed the pregnancy follow up. AV wrote the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
The patient’s oral and written consent for publication has been obtained.
Ethics approval and consent to participate
The patient’s written and consent has been obtained.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (https://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Vivanti, A.J., Cordier, AG., Baujat, G. et al. Abnormal pelvic morphology and high cervical length are responsible for high-risk pregnancies in women displaying achondroplasia. Orphanet J Rare Dis 11, 166 (2016). https://doi.org/10.1186/s13023-016-0529-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13023-016-0529-5